The FDA-approved smoking cessation pill, varenicline, has emerged as a pivotal tool in addressing the escalating vaping epidemic among teens and young adults. A recent study published in JAMA highlights its effectiveness, showing that participants aged 16 to 25 who used varenicline were three times more successful at quitting vaping compared to those receiving only behavioral counseling. This groundbreaking research not only underscores the pressing need for effective cessation strategies but also reveals the potential of pharmacological treatments in combating nicotine addiction. With vaping becoming increasingly common, particularly among adolescents, understanding the success of varenicline could reshape the landscape of smoking cessation efforts. As we delve into the world of vaping cessation, it’s crucial to recognize how FDA-approved treatments like varenicline can significantly impact the lives of young nicotine users seeking to break free from their dependence.
In the realm of nicotine dependence, alternative solutions such as varenicline — a clinically endorsed pill for quitting smoking — are gaining widespread attention. Designed specifically for individuals struggling with the habit of vaping, this treatment shows promise in helping younger populations achieve lasting cessation. Research indicates that combining this medication with behavioral therapies yields remarkable results, especially among teenagers and young adults. As communities strive to find effective means to counter the viral rise of vaping, understanding the benefits of such FDA-sanctioned therapies becomes increasingly relevant. Addressing the addiction crisis among youths can pave the way for healthier futures, where quitting nicotine is a manageable milestone.
The Impact of Varenicline on Vaping Cessation
Varenicline, an FDA-approved smoking cessation pill, has demonstrated significant efficacy in helping teens and young adults overcome their vaping habits. In a recent clinical study, participants aged 16 to 25 who were prescribed varenicline were over three times more successful in quitting vaping when compared to those taking placebo. This highlights the potential for medication like varenicline to serve as a pivotal tool in addressing the growing issue of nicotine addiction among younger populations. By engaging in a structured treatment plan that includes behavioral counseling alongside medication, these individuals can tackle the psychological and physical challenges associated with quitting.
Moreover, the accessibility of varenicline for those as young as 16 expands the opportunities for effective intervention. Given the alarming rates of vaping among teens, with approximately 25% of young adults and 8% of high schoolers vaped recently, there is an urgent need for FDA-approved treatments like varenicline. These findings from Harvard-affiliated Mass General Brigham illuminate not only the success rates but also the overall safety of varenicline, as participants did not shift to traditional cigarette smoking post-treatment. This establishes varenicline as a cornerstone in the fight against youth nicotine addiction.
Understanding Vaping Trends Among Teens
The prevalence of vaping among teens is a pressing health issue that necessitates comprehensive strategies for cessation. Recent studies indicate that the popularity of vaping has surged, leading to a significant public health concern given its association with nicotine addiction and its potential to act as a gateway to more harmful substances. Vaping products, often perceived as safer than traditional cigarettes, still pose substantial risks, including exposure to carcinogens and heavy metals. Understanding the trends and patterns of vaping among youth is essential for developing targeted prevention and treatment initiatives.
Effective vaping cessation programs must engage with this demographic using relatable and impactful messaging. It is important for healthcare providers to discuss the realities of nicotine addiction and the long-term health consequences of vaping, as well as to promote evidence-based FDA-approved treatments. By informing young people about the resources available to them, such as varenicline, there is a better chance of altering the trajectory of nicotine use among future generations. Empowering teens with knowledge and medication options can make a significant difference in curbing the vaping epidemic.
Innovative Behavioral Support for Teens Quitting Vaping
In addition to pharmacological interventions, behavioral support is a fundamental component of successful vaping cessation among teens. The study conducted by Mass General Brigham incorporated weekly behavioral counseling alongside varenicline, reflecting an integrative approach to treatment. This combination allows young individuals to address the emotional and cognitive aspects of addiction while receiving medical support. Behavioral therapy provides crucial coping strategies and lifestyle changes necessary for long-term cessation, which can enhance the efficacy of medications like varenicline.
Utilizing services like ‘This is Quitting,’ a text-based support platform aimed at younger users, complements traditional counseling. By fostering a community of support through digital platforms, teens can voice their struggles and successes, ultimately feeling less isolated in their journey to quit. This dual approach not only promotes accountability but also reinforces the commitment to quit vaping, showing promising results in treatment efficacy among young adults. As this age group continues to face unique challenges, innovative support systems are key to overcoming nicotine dependence.
The Role of Public Health in Combating Vaping
Public health initiatives play a crucial role in addressing the vaping epidemic among teens. Educational campaigns aimed at raising awareness about the dangers of vaping and the availability of effective cessation tools such as varenicline are essential. These campaigns should be tailored to resonate with youth, employing platforms they frequently engage with, such as social media, to disseminate accurate and compelling information about vaping risks. By leveraging influencers and relatable content, public health messaging can work to shift perceptions of vaping from a benign activity to a serious health risk.
Furthermore, increasing access to cessation resources, including prescriptions for varenicline and behavioral support services, is fundamental in public health strategies. Targeted outreach to schools and community centers can help identify at-risk youth and provide them with the necessary tools to quit vaping. Collaborating with stakeholders, including healthcare providers and educators, can help create a supportive environment that fosters discussions around nicotine addiction and promotes healthier choices among adolescents. Community-driven initiatives not only empower youth but also contribute to a broader societal effort to reduce nicotine dependence.
Research Insights into Nicotine Addiction
Ongoing research into nicotine addiction is critical for understanding the dynamics of vaping and the effective methods for cessation. Studies like the one from Mass General Brigham are pioneering efforts to investigate the impacts of varenicline on young individuals, emphasizing the need for tailored interventions that address the unique health behaviors of teens. As data reveal more about the biological and psychological factors associated with nicotine dependency, healthcare professionals can refine treatment approaches, ensuring they meet the specific needs of adolescents battling against vaping.
Future research should also consider the long-term effects of vaping and the potential for dual addictions, particularly among teens who shift from vaping to traditional cigarettes. By examining the nuances of addiction trajectories and developing comprehensive treatment methodologies, healthcare providers can better assist young individuals in overcoming their dependencies. Collaboration between researchers, healthcare professionals, and policymakers is essential to inform best practices in vaping cessation and enhance the effectiveness of FDA-approved treatments like varenicline.
Addressing Safety Concerns in Vaping Treatment
While varenicline shows promise in helping teens quit vaping, it is essential to address concerns regarding safety and potential side effects. The recent study underscores that no participants who quit vaping transitioned to cigarette smoking, which is a critical outcome in evaluating the safety of varenicline. Monitoring participants during follow-ups allows researchers to assess not only the effectiveness of the treatment but also the overall health of the individuals involved. This vigilance is crucial as it helps ensure that innovative treatments do not introduce new risks.
Additionally, healthcare providers should communicate transparently about the safety profile of varenicline, reassuring teens and their caregivers of its low risk compared to other nicotine products. Strategies must also include thorough patient education on the importance of following prescribed guidelines and reporting any adverse effects. This approach fosters a culture of safety and trust, encouraging young individuals to seek help in their quitting journey while feeling supported by the healthcare system.
Community Engagement in Vaping Cessation Efforts
Community engagement plays a vital role in the effectiveness of vaping cessation programs, especially among teens. Involving local organizations, schools, and healthcare providers in outreach initiatives can create a robust support network for young people struggling with nicotine addiction. Community-driven programs can also facilitate workshops and informational sessions that educate families about the dangers of vaping and the tools available for cessation, including varenicline. By harnessing community resources, we can build a comprehensive framework that encourages collaboration and mutual support.
Moreover, peer-led initiatives can be particularly effective in combating vaping among teens. Programs that empower young leaders to educate their peers about the risks of vaping and share their cessation journeys can resonate more deeply than traditional methods. Through storytelling and shared experiences, teens can influence one another positively, creating an environment that prioritizes health over nicotine dependency. By placing youth at the forefront of prevention and cessation efforts, communities can enhance their effectiveness and inspire lasting behavioral change.
Cultural Factors Influencing Vaping Behavior
Understanding the cultural factors that influence vaping behavior among teens is crucial for developing effective interventions. Cultural narratives around vaping often depict it as a trendy and socially acceptable alternative to smoking, which can perpetuate its appeal to adolescents. By analyzing these cultural perceptions, public health professionals can craft messages that challenge these narratives and highlight the real health consequences associated with vaping. Effective communication strategies must resonate with the values and interests of teens, helping them see quitting as a desirable path.
Additionally, engaging cultural figures and influencers in these efforts can amplify the reach and impact of cessation campaigns. When peers and public figures openly discuss their own experiences with vaping, including struggles and successes in quitting, it can demystify the challenges of addiction and make the goal of cessation seem more attainable. Tailoring messages to reflect the diverse backgrounds and experiences of teens can help foster a more inclusive dialogue about vaping, ultimately encouraging a broader cultural shift away from nicotine dependence.
Future Directions in Vaping Research and Treatment
As vaping continues to evolve, future research must adapt to emerging trends and address the challenges of nicotine addiction among youths. Investigating the long-term effects of vaping on health, developing diverse cessation strategies, and exploring the efficacy of alternative treatments, alongside varenicline, are necessary areas of focus. The ongoing dialogue in the scientific community about vaping will enable us to understand better how addiction operates among evolving nicotine products and the best ways to combat it in younger populations.
Moreover, collaboration between researchers, clinicians, and public health officials is essential in translating study findings into actionable policies and practices. By leveraging insights gained from research, stakeholders can work together to enhance prevention efforts, increase access to cessation resources, and promote a unified message against vaping. The ultimate goal is to foster an environment where young individuals can make informed decisions about their health and be supported in their journey to quit nicotine entirely.
Frequently Asked Questions
What is the FDA-approved smoking cessation pill for quitting vaping?
The FDA-approved smoking cessation pill for quitting vaping is varenicline. It is designed to help individuals, including teens and young adults, to break their nicotine addiction effectively.
How effective is varenicline in helping young adults quit vaping?
Varenicline has shown to be highly effective in helping young adults quit vaping. Clinical studies indicate that participants who used varenicline were more than three times as likely to quit compared to those who received a placebo.
Can teens use varenicline as a smoking cessation pill?
Yes, teens aged 16 to 25 can use varenicline as a smoking cessation pill to help them quit vaping. It has been studied specifically for this vulnerable population and is deemed safe and effective.
What are the benefits of using varenicline for vaping cessation?
The benefits of using varenicline for vaping cessation include significantly higher success rates in quitting compared to other methods, the ability to reduce cravings, and a positive impact on health without leading to a switch to cigarette smoking.
Are there any side effects associated with varenicline as a smoking cessation pill?
While varenicline is generally safe for use, some individuals may experience side effects. It’s important for users to discuss these with their healthcare provider to manage any potential risks.
How does varenicline work to help people quit vaping?
Varenicline works by stimulating nicotine receptors in the brain, which helps reduce withdrawal symptoms and cravings associated with quitting nicotine. This dual-action approach aids in breaking the vaping habit more effectively.
Is behavioral counseling necessary when using varenicline for vaping cessation?
While varenicline can be effective on its own, combining it with behavioral counseling can enhance quitting success rates. The best results often come from a comprehensive treatment plan that includes both medication and counseling.
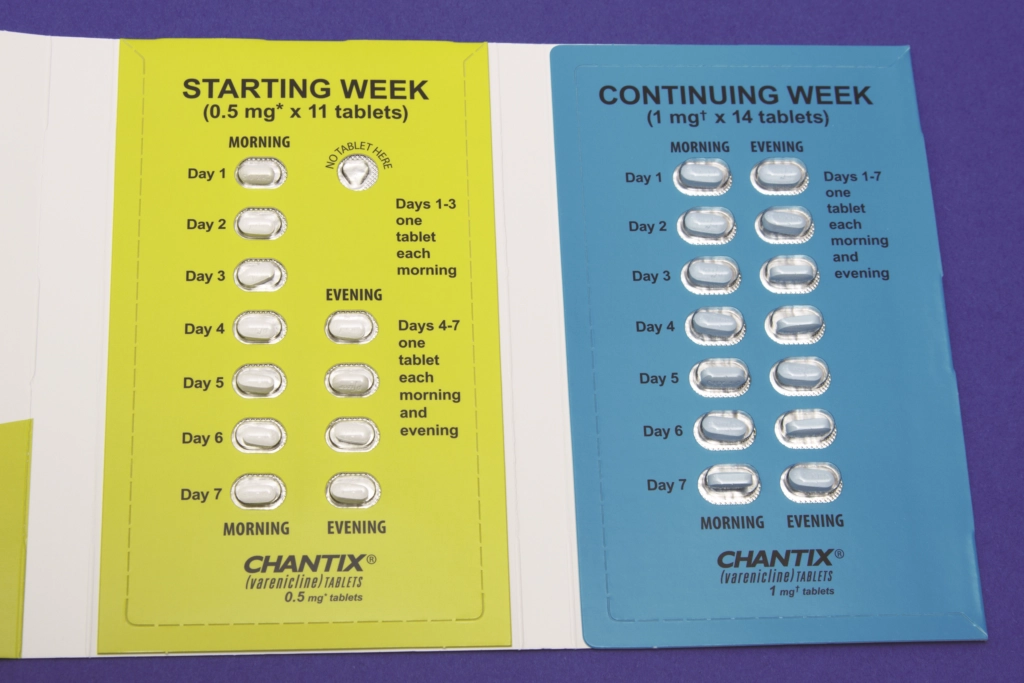
How long should someone take varenicline to quit vaping?
Typically, varenicline is prescribed for a period of 12 weeks, during which users receive support and monitoring to maximize their chances of quitting vaping successfully.
What is the success rate of varenicline for vaping cessation among young adults?
In clinical studies, about 51% of young adults using varenicline were able to stop vaping after 12 weeks, which is considerably higher than the success rates of those using placebo treatments.
What should I do if varenicline does not work for quitting vaping?
If varenicline does not work, it’s advisable to consult a healthcare provider for alternative treatment options or therapeutic approaches that may better suit your individual needs.
| Key Point | Details |
|---|---|
| FDA-approved Medication | Varenicline is the key smoking cessation pill, approved for adults but effective in teens 16-25. |
| Clinical Trial Success Rates | Participants taking varenicline were 3 times more likely to quit vaping than those with placebos (51% vs 14% at 12 weeks). |
| Behavioral Support | All groups received weekly counseling and access to the ‘This is Quitting’ text support service, highlighting the added importance of medication. |
| Vaping Among Youth | Approximately 25% of 18-25 year-olds and 8% of high schoolers were found to vape, underlining the critical need for effective smoking cessation tools. |
| Safety of Varenicline | The study concluded that varenicline was safe for use in the younger population without leading to a switch to cigarette smoking. |
Summary
The smoking cessation pill, varenicline, has proven to be a groundbreaking solution in aiding teens and young adults to quit vaping effectively. As highlighted in a recent clinical trial, this FDA-approved medication demonstrates significant success, with participants quitting at three times the rate of those using placebo treatments. With the alarming rise of vaping among youth, the findings underscore the urgent need for accessible, effective smoking cessation options. Varenicline not only facilitates quitting but does so safely, marking a vital step in addressing nicotine addiction within this vulnerable group.