Maternal mortality in the U.S. has become an alarming public health crisis, with recent studies indicating a rise in pregnancy-related deaths that continues to outpace other high-income countries. Shockingly, over 80 percent of these deaths are deemed preventable, highlighting significant gaps in maternal healthcare. Disparities in maternal health outcomes across states and racial groups only exacerbate the issue, as American Indian and Alaska Native women experience markedly higher mortality rates than their white counterparts. The implications of high maternal mortality rates extend beyond pregnancy, affecting postpartum care and overall maternal health disparities in the nation. As we delve into this pressing topic, it becomes crucial to identify effective strategies to combat preventable maternal deaths and enhance care during and after pregnancy.
The rising rates of maternal fatalities in the United States pose a serious challenge for public health, raising concerns about the safety and efficacy of pregnancy and childbirth experiences. With a significant portion of pregnancy-related deaths classified as avoidable, the focus is increasingly on improving healthcare systems and support during and after delivery. Many women face elevated risks due to various factors, including socioeconomic disparities and inadequate access to quality care, particularly during the postpartum phase. This troubling trend calls for a thorough examination of maternal health conditions and the immediate need for interventions to curb the surge in these tragic outcomes. Understanding how social determinants impact maternal well-being is vital for developing comprehensive solutions to intervene in this growing crisis.
Understanding Maternal Mortality Rates in the U.S.
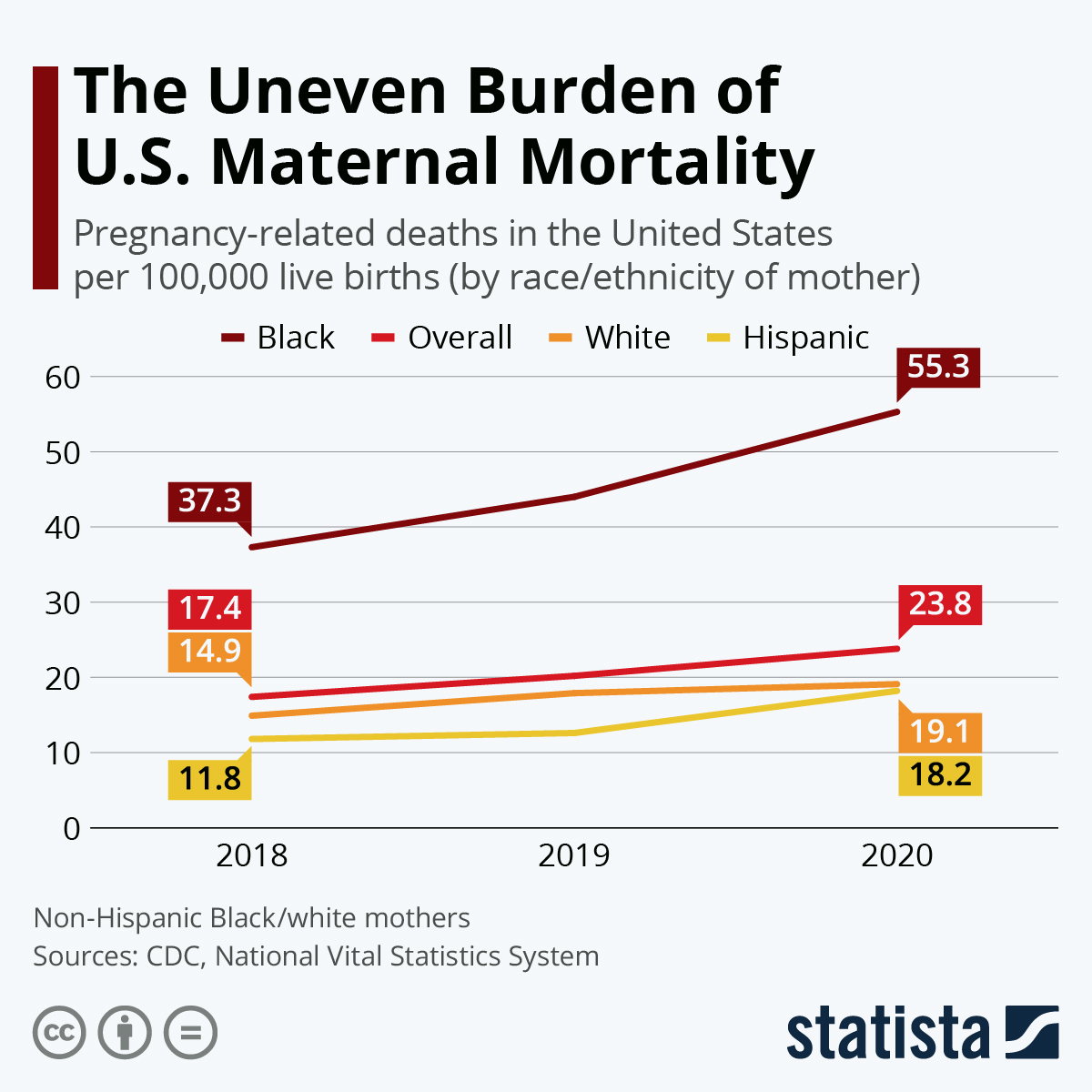
Maternal mortality in the U.S. remains a pressing public health issue, with pregnancy-related deaths significantly surpassing those in other high-income nations. A recent study indicates that about 80 percent of these deaths are preventable, emphasizing the critical need for improved healthcare during and after pregnancy. The U.S. recorded 32.6 maternal deaths per 100,000 live births in 2022, marking a stark increase from 25.3 in 2018, reflecting not just a troubling trend, but an urgent call for systemic change. Policy reform aimed at equitable healthcare access is crucial to reducing these mortality rates, particularly for disadvantaged population groups who face higher risks based on race and geography.
The rise in maternal mortality is characterized by stark disparities; American Indian and Alaska Native women, for instance, experience mortality rates nearly four times higher than their white counterparts. This suggests that maternal health disparities are deeply rooted in social determinants, such as income, education, and access to quality healthcare services. Effective policy changes must address these variances, fostering an environment where all women receive essential prenatal and postpartum care to mitigate risks associated with pregnancy-related deaths.
The Importance of Postpartum Care in Maternal Health
Postpartum care is an often-overlooked aspect of maternal health that has a profound impact on long-term wellness for new mothers. The U.S. healthcare system traditionally emphasizes the immediate post-birth recovery period, often neglecting a more extended approach to postpartum care. However, findings indicate that a significant proportion of pregnancy-related deaths occur in the months following childbirth, highlighting the necessity of comprehensive services that extend beyond the initial six weeks. This shift from reactive to proactive healthcare measures could drastically lower rates of preventable maternal deaths.
Holistic postpartum care should include mental health support, management of pre-existing conditions, and education about warning signs that could avert complications. With late maternal deaths accounting for nearly a third of total pregnancy-related fatalities, it is crucial to recognize that recovery does not end at the hospital discharge. By adopting a more inclusive and longitudinal approach to maternal care, healthcare providers can better address the complexities of maternal health, ultimately leading to improved outcomes and quality of life for mothers.
Factors Contributing to Preventable Maternal Deaths
Preventable maternal deaths highlight systemic issues within the U.S. healthcare landscape, marked by inequitable access to care, particularly for marginalized communities. The findings from recent studies suggest that many contributing factors such as chronic health conditions, a lack of affordable insurance, and inadequate prenatal care lead to high maternal mortality rates. Additionally, the COVID-19 pandemic has exacerbated these issues, as many hospitals faced capacity challenges while healthcare access became constrained. Addressing these barriers is essential to reducing preventable deaths.
Moreover, social determinants of health play a crucial role in these disparities. Economic instability, educational inequities, and systemic racism contribute to the heightened risks faced by women of color and those living in rural areas. Comprehensive public health strategies that advocate for policy changes, improved insurance coverage, and access to high-quality maternal services are necessary to combat these preventable deaths. The implementation of better tracking systems for maternal health outcomes can also lead to enhanced monitoring, informing strategies for reducing pregnancy-related deaths.
Addressing Maternal Health Disparities Across Racial Lines
Maternal health disparities are starkly evident, with significant differences based on race and ethnicity. American Indian and Alaska Native women experience the highest mortality rates, while non-Hispanic Black women also face disproportionately high rates compared to white women. These disparities suggest deep-rooted societal issues, including discrimination and inequities in healthcare access and quality. Efforts to diversify healthcare policy and increase representation within the medical community are critical to addressing these disparities.
To diminish these gaps, there must be an emphasis on culturally competent care that acknowledges and addresses the unique needs of diverse racial populations. This includes implementing community-based interventions that focus on education, access to prenatal and postpartum care, and outreach programs designed to connect underserved populations with the resources they need. Government initiatives should also support research aimed at understanding these disparities to inform effective policy changes and drive health equity across all demographics.
The Role of Chronic Conditions in Maternal Mortality
Chronic health conditions are emerging as significant contributors to maternal mortality rates in the U.S. Recent studies have shown an alarming trend: younger women are increasingly at risk of developing conditions like hypertension, which have traditionally impacted older demographics. The rise in chronic diseases among pregnant individuals can be attributed to various factors, including lifestyle changes and systemic inequalities in healthcare access, which require urgent attention.
Addressing chronic conditions within maternal healthcare requires a multi-tiered approach, including education, early screening, and tailored management strategies. Ensuring continuous monitoring of medical conditions prior to and throughout pregnancy could significantly reduce risks. Additionally, healthcare systems must prioritize preventative care and implement integrated health strategies that allow for comprehensive management of chronic illnesses, which in turn can lower rates of maternal mortality and improve overall pregnancy outcomes.
The Impact of State-Level Variations on Maternal Health Outcomes
State-level variations in maternal health outcomes pose significant challenges to achieving nationwide improvements in maternal mortality rates. The disparities illustrate how healthcare access, quality, and policies can differ drastically across the U.S., leading to better outcomes in some regions, notably California, which serves as a benchmark for effective maternal health strategies. Understanding these differences can guide targeted interventions tailored to each state’s unique challenges.
High maternal mortality rates in certain states point to systemic issues such as limited access to prenatal care, varying healthcare policies, and differences in public health funding. Addressing these issues at the policy level is vital to establishing a more equitable healthcare system. State governments must commit to improving maternal health by investing in supportive services for expectant mothers and by adopting best practices shared among states with successful outcomes, ultimately striving for a unified approach to maternal health challenges.
Innovations Needed in Maternity Care Systems
Innovation in maternity care is essential for addressing the high rates of preventable maternal deaths in the U.S. Current healthcare systems often lack the flexibility and resources needed to provide comprehensive care throughout the entire pregnancy and postpartum period. By investing in new models of care that prioritize continuity and communications among caregivers, maternal health outcomes could see significant improvement. Programs that emphasize team-based approaches involving obstetricians, midwives, and maternal-fetal specialists have been shown to enhance care quality and reduce complications.
Emerging technology also presents new opportunities for monitoring maternal health, such as telehealth services that allow for remote consultations and continuous health monitoring. The integration of such technologies can bridge gaps in care for women living in rural or underserved urban areas, providing them with timely interventions and support. As these innovations are implemented, ongoing evaluation and research must continue to gauge their effectiveness in improving maternal healthcare and address areas requiring further reform.
The Long-Term Consequences of Maternal Mortality
The impact of maternal mortality extends beyond the individual mother; it has lasting consequences for families and communities. The loss of a mother can lead to severe emotional and financial hardships, affecting children’s stability and well-being. Additionally, communities face broader socio-economic implications with increased healthcare costs and loss of productivity when mothers die preventably. Acknowledging the ripple effects of maternal mortality emphasizes the urgent need to prioritize maternal health within public health agendas.
Moreover, the societal undervaluation of maternal health often results in insufficient investment in programs aimed at preventing maternal deaths. Such neglect compromises not only the health of mothers but also the development and health of the next generation. Initiatives focused on improving maternal health must be framed within a broader context of family and community health, advocating for integrated policies that emphasize family well-being, reproductive health, and generational health outcomes.
Systemic Changes for Improving Maternal Health
Addressing the high maternal mortality rates in the U.S. necessitates systemic changes within healthcare systems. To effectively combat the prevalence of pregnancy-related deaths, investments in public health infrastructure are paramount. Funding cuts that target maternal health compromise the ability to monitor outcomes, track disparities, and implement effective interventions. It is essential for policymakers to recognize the need for sustained investment in maternal healthcare as a crucial area of public health.
Moreover, systemic changes should include increasing awareness and training regarding the unique healthcare needs of pregnant and postpartum individuals among healthcare providers. Continuous education on potential risks and up-to-date practices can empower healthcare professionals to deliver timely and effective care. Supporting initiatives that focus on reducing bias and improving communication between providers and patients can also foster a more supportive environment, ultimately leading to better maternal health outcomes.
Frequently Asked Questions
What is contributing to the high maternal mortality rates in the U.S.?
High maternal mortality rates in the U.S. are attributed to a combination of factors, including an inequitable healthcare system, lack of access to quality prenatal care, and systemic biases that affect maternal health across different racial and ethnic groups.
How do maternal health disparities impact pregnancy-related deaths in the U.S.?
Maternal health disparities significantly impact pregnancy-related deaths in the U.S. For instance, American Indian and Alaska Native women face the highest mortality rates, highlighting the urgent need to address these inequities through targeted healthcare policies and improved access to care.
What role does postpartum care play in preventing maternal mortality?
Postpartum care is crucial in preventing maternal mortality, as nearly one-third of pregnancy-related deaths occur beyond the immediate postpartum period. Comprehensive care extending throughout the first year postpartum is essential for monitoring health and addressing emerging risks.
Are most pregnancy-related deaths in the U.S. preventable?
Yes, over 80 percent of pregnancy-related deaths in the U.S. are considered preventable, indicating a critical opportunity for healthcare systems to improve maternal health outcomes through better prenatal and postpartum care.
What measures can help reduce high maternal mortality rates in the U.S.?
To reduce high maternal mortality rates, the U.S. needs to invest in public health infrastructure, enhance the quality of maternity care, and implement policies that address the specific needs of diverse populations, especially in states with higher mortality rates.
How has the COVID-19 pandemic affected maternal health in the U.S.?
The COVID-19 pandemic has been linked to an increase in pregnancy-related deaths, with significant spikes observed in 2021. The pandemic exacerbated existing health disparities and underscored the need for robust maternal healthcare systems.
What are the leading causes of pregnancy-related deaths in the U.S.?
Cardiovascular disease has emerged as the leading cause of pregnancy-related deaths in the U.S., accounting for over 20% of such fatalities. This shift from complications like hemorrhage to chronic conditions signifies a changing landscape of maternal health risks.
Why is late maternal death significant to maternal health discussions?
Late maternal deaths, occurring between 42 days and one year postpartum, are significant because they highlight the need for continuity of care and comprehensive support for women recovering after childbirth, a time often overlooked by healthcare systems.
What data tracking challenges exist regarding maternal mortality in the U.S.?
Until 2018, there was no standardized national system for tracking maternal deaths in the U.S., making it difficult to obtain accurate and comprehensive data on pregnancy-related deaths, which is now being addressed with improved death certificate protocols.
What actions are needed to improve maternal health outcomes in the U.S.?
Improving maternal health outcomes in the U.S. requires increased investment in public health initiatives focused on reducing maternal mortality rates, addressing health disparities, and expanding access to quality reproductive care throughout pregnancy and postpartum.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality | The U.S. leads high-income countries in maternal mortality rates, with a significant rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Disparities | Notable disparities exist by state, race, and ethnicity, with American Indian and Alaska Native women facing the highest mortality rates. |
| Leading Cause of Death | Cardiovascular disease is now the leading cause of pregnancy-related deaths, accounting for over 20%. |
| Impact of COVID-19 | The pandemic may have exacerbated the rise in maternal deaths, especially in 2021. |
| Postpartum Care | Late maternal deaths (42 days to 1 year after pregnancy) account for nearly a third of deaths, indicating the need for improved postpartum care. |
| Investment in Healthcare | Increased investment is needed in healthcare infrastructure and innovative solutions to improve maternal health outcomes. |
Summary
Maternal mortality in the U.S. has reached alarming levels, continuing to rise despite being in a high-income country. The trends from the latest studies highlight that over 80% of these deaths are preventable, emphasizing the urgent need for enhanced prenatal and postpartum care. Danial disparities influenced by race and state policies underscore the critical nature of addressing the healthcare inequalities contributing to this public health crisis. Investment in healthcare infrastructure and innovative solutions is essential to ensure better maternal health outcomes and reduce mortality rates in the future.