
Alzheimer’s Disease Research: Insights from Beth Stevens
Alzheimer’s disease research is at the forefront of a scientific evolution, driven by the groundbreaking investigations of neuroscientist Beth Stevens. Exploring the role of microglial cells, the brain’s immune system, Stevens has revealed their pivotal function in maintaining neural health through processes like synaptic pruning. However, when microglia malfunction, the consequences can be dire, leading to neurodegenerative diseases such as Alzheimer’s and Huntington’s. At the Stevens Lab, significant strides are being made to identify biomarkers and therapeutic strategies that could drastically improve the lives of millions grappling with Alzheimer’s. Through her passion and dedication, Stevens embodies the relentless pursuit of knowledge necessary to unlock the mysteries of the brain and offer hope where there is none.
Investigations into dementia-related illnesses are shaping the landscape of neurological science, particularly in understanding how the brain’s defense mechanisms impact overall cognition. Beth Stevens’ work elucidates the essential role of glial cells—critical components of the brain’s immune response—in managing neural integrity and function. These glial cells are not only instrumental in synapse management but also play a crucial role in thwarting neurodegenerative disorders, emphasizing the intersection of brain health and immune functionality. As researchers continue to explore these complex interactions, the insights garnered from such studies have the potential to revolutionize approaches towards treating cognitive decline. This avenue of research opens up new frontiers in discovering effective strategies to combat the effects of age-related brain deterioration.
Understanding Microglial Cells and Their Role in Neurodegenerative Diseases
Microglial cells are a vital component of the brain’s immune system, acting as sentinels that monitor the health of the central nervous system. In recent years, research has illuminated their critical role in maintaining brain homeostasis and synaptic integrity. When functioning properly, these cells assist in the removal of damaged neurons and facilitate synaptic pruning, a process essential for optimal neural connections. However, when microglial cells become dysfunctional, they can contribute to the progression of neurodegenerative diseases, including Alzheimer’s disease. This aberrant activity can lead to improper synaptic pruning, resulting in cognitive decline and other devastating symptoms.
Current investigations into microglial biology are unveiling connections between these immune cells and various neurodegenerative disorders. As researchers like Beth Stevens demonstrate, understanding how microglia interact with neuronal environments can reveal new targets for therapeutic intervention. By exploring the intricate signaling pathways in which microglia engage, scientists are shifting towards a more nuanced understanding of brain health and disease. Such insights are essential for developing innovative treatments aimed at mitigating the effects of diseases like Alzheimer’s, ultimately improving patient outcomes and transforming care approaches.
The Groundbreaking Research of Beth Stevens on Alzheimer’s Disease
Beth Stevens has made significant contributions to the field of Alzheimer’s disease research through her groundbreaking studies on microglial cells. By focusing on how these immune cells manage synaptic pruning, Stevens and her team have uncovered crucial information that links dysregulated microglial activity to the pathogenesis of Alzheimer’s. Such findings highlight the importance of early intervention strategies that aim to restore normal microglial function before irreversible damage occurs. The implications of her research are vast, potentially paving the way for novel biomarkers that could predict the onset of Alzheimer’s symptoms long before conventional clinical signs manifest.
Her exploration into the brain’s immune system has opened new avenues for effectively tackling neurodegenerative diseases. Stevens emphasizes that supporting foundational research, driven by curiosity, is essential for scientific advancement. The link between microglial dysfunction and diseases such as Alzheimer’s demonstrates how fundamental insights into synaptic biology can lead to practical applications in diagnostics and therapeutics. Through the investigation of microglial behavior, researchers can better understand the complexities of brain disorders, thus enhancing strategies for prevention and treatment for millions impacted by these conditions.
The Importance of Synaptic Pruning in Brain Development and Disease
Synaptic pruning is a biological process essential for the proper development and function of neural circuits in the brain. During early brain development, microglial cells play a critical role in the selective elimination of excess synapses, ensuring that neural connections are optimized for efficient communication. This pruning process is not only vital for healthy brain development but continues to be an important mechanism throughout life, influencing learning, memory, and overall cognitive function. Disruptions in this mechanism have been linked to various neurodegenerative diseases, including Alzheimer’s, highlighting the importance of understanding how synaptic pruning goes awry.
Research has shown that improper synaptic pruning can lead to an imbalance in neural connectivity, which is characteristic of Alzheimer’s disease and other cognitive disorders. By studying microglial activity in relation to synaptic pruning, researchers aim to uncover the underlying etiologies of these disorders. Understanding the delicate balance of neural networking could inform future therapeutic strategies aimed at correcting synaptic abnormalities. It is crucial for the scientific community to continue exploring these processes to not only illuminate the mechanisms of disease but also to foster the development of innovative treatments that can mitigate the impact of neurodegenerative diseases on individuals and society.
Revolutionizing Alzheimer’s Disease Therapeutics Through Misguided Immune Responses
The immune system’s response plays a dual role in neurodegenerative diseases, particularly in the context of Alzheimer’s disease. Misguided immune responses can lead to detrimental effects, exacerbating existing neuroinflammation and contributing to neuronal death. Research led by scientists like Beth Stevens has shown how microglial cells, when activated incorrectly, can result in the over-pruning of synapses, adversely affecting cognitive functions. This relationship between immune dysfunction and neuronal health is a burgeoning area of study, as understanding it could lead to more targeted interventions for Alzheimer’s.
To combat these adverse immune responses, ongoing research is focusing on the mechanisms that govern microglial activity. By elucidating these pathways, scientists hope to identify potential intervention points, allowing for the modulation of microglial behavior to promote neuroprotection and support neuronal health. The goal of this research is not only to improve therapeutic outcomes for those suffering from Alzheimer’s but also to provide a deeper understanding of how neurodegenerative diseases can be approached from an immune system perspective, ultimately reshaping treatment paradigms in neurology.
NIH Support: The Backbone of Alzheimer’s Disease Research
The National Institutes of Health (NIH) has played a pivotal role in advancing Alzheimer’s disease research, providing essential funding to scientists exploring the complexities of neurodegeneration. The support received by researchers like Beth Stevens has enabled the pursuit of critical questions about the brain’s immune system and its relationship to diseases such as Alzheimer’s. NIH funding has facilitated the exploration of exciting new hypotheses and innovative research methodologies, driving forward our understanding of how microglial cells function and contribute to synaptic health.
This commitment to foundational research underscores the importance of sustained investment in understanding the biological underpinnings of Alzheimer’s disease. The findings derived from well-supported studies not only enrich the scientific community’s knowledge but also lead to actionable insights that can translate to therapeutic and diagnostic advancements. With NIH backing, the potential for breakthroughs increases exponentially, offering hope to millions affected by Alzheimer’s disease and other neurodegenerative conditions.
The Intersection of Curiosity-Driven Science and Clinical Applications
Curiosity-driven science lies at the heart of groundbreaking discoveries in the field of Alzheimer’s research, particularly in understanding the role of microglial cells. Beth Stevens’ journey exemplifies how initial explorations into seemingly unrelated areas—like the visual system of mice—can yield valuable insights into complex neurological conditions. By allowing scientists the freedom to follow their research interests, we can uncover significant connections that lead to clinical applications in treating diseases such as Alzheimer’s.
As Stevens points out, the connection between foundational research and clinical outcomes is not always immediately apparent. However, it is this very inquiry-based approach that enables researchers to tackle questions that cannot be addressed in human studies. This innovative mindset fosters a deeper understanding of brain function and disease, paving the way for targeted therapies that aim to improve quality of life for individuals affected by neurodegenerative diseases. Thus, supporting curiosity-driven research will be essential for the future of Alzheimer’s disease intervention.
Innovations in Alzheimer’s Disease Biomarkers and Therapeutics
The advancement of biomarkers in Alzheimer’s disease is crucial for early detection and intervention. As Beth Stevens emphasizes, understanding microglial functioning and its impact on synaptic pruning can provide critical insights into the inflammatory processes underlying the disease. Identifying reliable biomarkers can help in assessing individual risk and potentially directing treatments at the most opportune moments in the disease course. The goal is to transform our current approach from a reactionary stance to one that emphasizes prevention and timely therapeutic intervention.
Recent investigations in Stevens’ lab have the potential to influence the development of novel therapeutics aimed at restoring normal microglial function, preventing the harmful effects of improper synaptic pruning. By focusing research efforts on the identification and application of these biomarkers, scientists can create a roadmap for managing Alzheimer’s disease more effectively. Ultimately, innovation in biomarker research holds the key to enhancing patient care and establishing new standards in how we approach Alzheimer’s disease treatment.
Implications of Neuroinflammation in Alzheimer’s Progression
Neuroinflammation has emerged as a significant contributor to the progression of Alzheimer’s disease, with microglial cells taking center stage in this narrative. Chronic activation of microglia can lead to neurotoxic effects, exacerbating neuronal loss and cognitive decline. Understanding the intricacies of how neuroinflammatory responses are regulated is critical for developing strategies to slow or prevent Alzheimer’s progression. The work of researchers like Beth Stevens expands upon this concept, highlighting the need for a concerted effort to investigate these immune dynamics in the context of neurodegeneration.
This research could lead to innovative therapeutic approaches aimed at modulating microglial behavior to foster a more protective environment for neurons. By targeting neuroinflammatory pathways, scientists can develop drugs that potentially alleviate symptoms and halt disease advancement. This promising area of exploration emphasizes the potential for harnessing the immune system to combat neurological diseases, indicating that a deeper understanding of neuroinflammation may be a gateway to novel Alzheimer’s disease management strategies.
Advancements in Alzheimer’s Education: A Community Perspective
Educating communities about Alzheimer’s disease is essential for managing its impact on individuals and families. Comprehensive education initiatives can demystify the complexities of the disease, fostering understanding and support for those affected. By sharing insights from research, particularly regarding the role of microglial cells and neuroinflammation, communities can become better equipped to engage with and support Alzheimer’s patients. Such educational efforts are critical in building a compassionate society that recognizes the value of medical research and its implications for public health.
Furthermore, community engagement can drive advocacy for continued support of Alzheimer’s disease research. By understanding the science behind neurodegenerative diseases, community members can advocate for necessary funding and resources that facilitate research advancements. The role of institutions like the NIH in providing grants illustrates the importance of public investment in scientific endeavors. As communities rally around the knowledge gained from studies on Alzheimer’s, they create an environment ripe for collaboration that ultimately leads to a better understanding of, and solutions for, the challenges posed by neurodegenerative diseases.
Frequently Asked Questions
How do microglial cells contribute to Alzheimer’s disease research?
Microglial cells are crucial for understanding Alzheimer’s disease as they act as the brain’s immune system. They help remove damaged cells and prune synapses, which is essential for healthy brain function. Research by Beth Stevens highlights how improper synaptic pruning by microglia can lead to the progression of Alzheimer’s and other neurodegenerative diseases.
What is the role of synaptic pruning in neurodegenerative diseases like Alzheimer’s?
Synaptic pruning is a process where microglial cells eliminate unnecessary synapses in the brain. In the context of Alzheimer’s disease, researchers like Beth Stevens have discovered that improper pruning may contribute to neurodegeneration. This emphasizes the importance of understanding synaptic mechanisms in Alzheimer’s disease research.
What advances in Alzheimer’s disease treatments have stemmed from microglial research?
Research into microglial cells, particularly by scientists like Beth Stevens, has paved the way for new biomarkers and potential medications for Alzheimer’s disease. By understanding the role of the brain’s immune system in synaptic pruning and damage control, researchers are developing innovative approaches to treat neurodegenerative diseases.
How does Beth Stevens’ research impact our understanding of the brain’s immune system in Alzheimer’s disease?
Beth Stevens’ research has significantly advanced our understanding of how the brain’s immune system, particularly microglial cells, functions in the context of Alzheimer’s disease. Her findings suggest that these cells, when functioning correctly, protect against neurodegeneration, but can exacerbate the disease when their pruning mechanisms go awry.
What are potential biomarkers for Alzheimer’s disease identified through microglial research?
Through the exploration of microglial cells, researchers have identified potential biomarkers linked to Alzheimer’s disease. These biomarkers may help in the early detection of neurodegenerative diseases, highlighting the importance of ongoing research in microglial function and Alzheimer’s pathology.
What challenges are faced in Alzheimer’s disease research related to microglial cells?
Challenges in Alzheimer’s disease research concerning microglial cells include understanding the dual roles these cells play in neuroprotection and neurodegeneration. As highlighted by Beth Stevens, their improper functioning can lead to exacerbated disease conditions, making it crucial to delineate these mechanisms to inform treatment strategies.
What foundational research supports the study of Alzheimer’s disease and microglial function?
Foundational research has been pivotal in advancing the study of Alzheimer’s disease, particularly research that focuses on microglial function. Supported by NIH grants, many breakthroughs have emerged from basic science that explores how these immune cells interact with neuronal processes, leading to greater insights into neurodegenerative diseases.
How can the understanding of microglia influence future Alzheimer’s disease therapies?
Understanding the role of microglia in the context of Alzheimer’s disease can radically influence future therapies. Insights from studies, such as those conducted by Beth Stevens, may lead to targeted treatments that modulate microglial activity to promote synaptic health and reduce neurodegeneration.
| Key Aspect | Details |
|---|---|
| Research Focus | Analysis of microglial cells and their role in Alzheimer’s disease and other disorders. |
| Importance of Microglia | Microglia act as the brain’s immune system, removing damaged cells and pruning synapses. |
| Research Impact | Findings help develop biomarkers and medications for treating neurodegenerative diseases. |
| Funding and Support | Stevens’ research is supported significantly by NIH and federal grants. |
| Long-term Vision | Research may lead to new understandings and treatments for Alzheimer’s disease. |
| Broader Implications | Basic research on microglia can lead to discoveries applicable to human health. |
Summary
Alzheimer’s disease research has revealed critical insights into the role of microglial cells in brain health. By understanding how these cells contribute to synaptic pruning and brain immunity, researchers like Beth Stevens are pioneering new ways to identify and treat neurodegenerative diseases. The ongoing support from institutions like the NIH underscores the value of curiosity-driven science, which often leads to significant advancements in medical knowledge and patient care. As research progresses, we look toward a future where improved treatments can enhance the quality of life for the millions affected by Alzheimer’s disease.
TIM-3 Therapy for Alzheimer’s: A Revolutionary Discovery
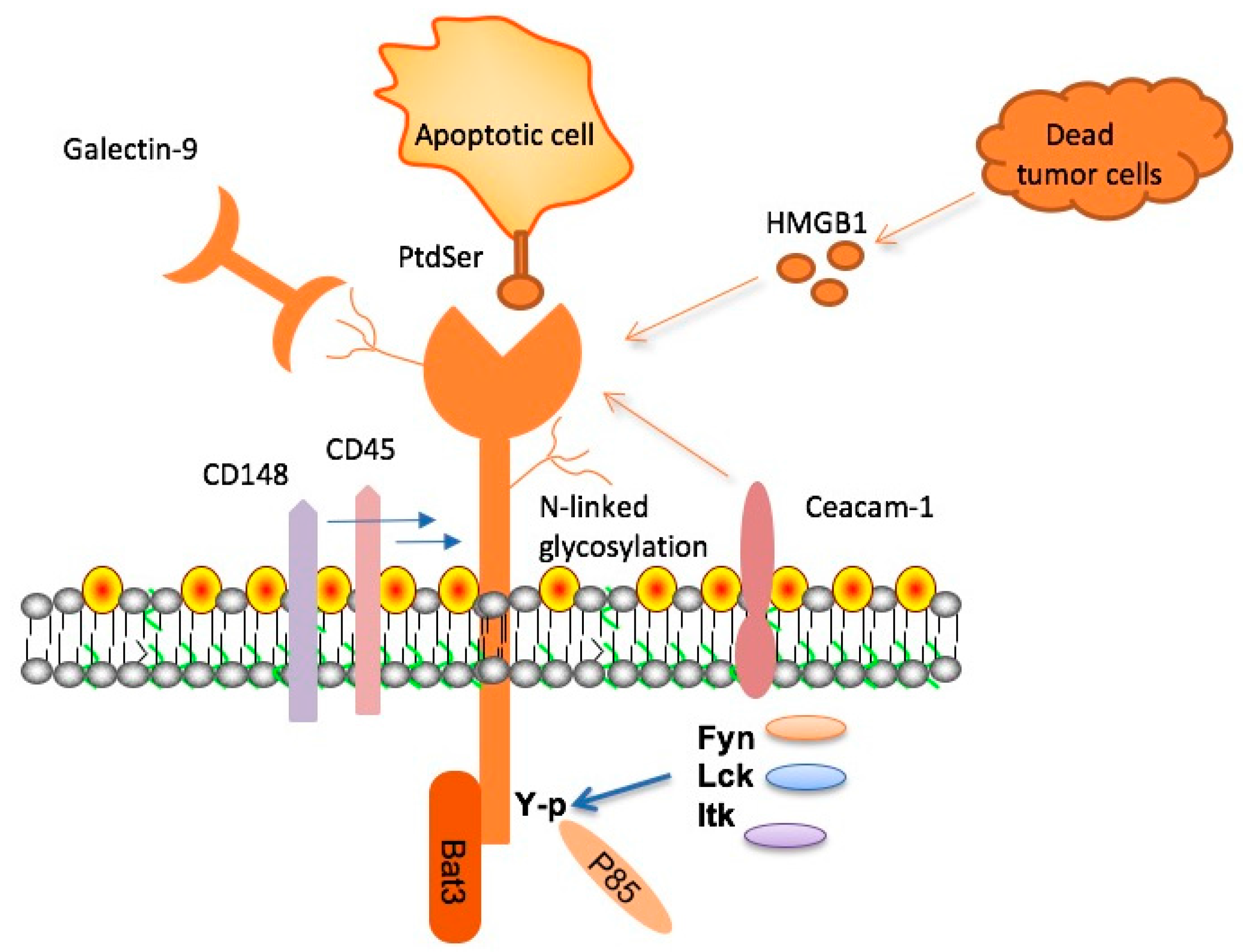
TIM-3 therapy for Alzheimer’s is an innovative approach that leverages the immune system’s mechanisms to combat Alzheimer’s disease, a condition that afflicts millions worldwide. Recent research highlights the potential of TIM-3, a checkpoint molecule, to enable microglia – the brain’s immune cells – to effectively clear toxic amyloid plaques linked to cognitive decline. This breakthrough is particularly significant as it aligns with developments in Alzheimer’s disease research that suggest harnessing immune strategies can enhance cognitive function improvement. By releasing the inhibitory effects of TIM-3, scientists aim to rejuvenate microglia, restoring their ability to facilitate plaque clearance and memory enhancement. As we explore the intricate connection between the immune system and Alzheimer’s, TIM-3 therapy may emerge as a promising candidate in the landscape of treatment strategies.
The exploration of TIM-3 in Alzheimer’s treatment reflects broader innovations in addressing neurodegenerative diseases through immune modulation. By targeting checkpoint molecules similar to those used in cancer therapies, researchers are investigating how therapeutic strategies aimed at this genetic factor can lead to advancements in cognitive health. Additionally, the unique role of microglia in maintaining brain homeostasis while combating plaque formation by amyloid beta underscores the delicate balance necessary for cognitive preservation. This situation invites further inquiry into how immune dysfunction contributes to Alzheimer’s, potentially reinforcing the relationship between immunological health and neurodegeneration. With studies like these paving the way, they challenge conventional approaches and stimulate a new paradigm in Alzheimer’s disease management.
The Role of TIM-3 in Alzheimer’s Disease Therapy
Recent research highlights the potential of TIM-3 therapy for Alzheimer’s disease, revealing that blocking this immune checkpoint molecule could enhance the ability of microglia to target and remove amyloid plaques from the brain. When researchers deleted the TIM-3 gene in a laboratory setting, they observed that mice demonstrated improved cognitive function and plaque clearance. This finding is significant because it suggests that TIM-3 plays a restrictive role in the brain’s immune response, and by inhibiting it, we may be able to shift the immune system’s balance toward more effectively combating Alzheimer’s pathology.
The therapeutic strategy surrounding TIM-3 focuses on its dual function within the immune system; while it is crucial for regulating T cell activity to prevent autoimmunity, its overexpression in Alzheimer’s patients hinders microglial functionality. By utilizing anti-TIM-3 antibodies or other small molecules that block its action, researchers could potentially restore microglial activity, facilitating the clearance of harmful plaques and leading to significant cognitive improvements. This approach may usher in new, targeted Alzheimer’s treatments that effectively harness the body’s immune mechanisms.
Understanding Microglia’s Role in Alzheimer’s Disease
Microglia are the brain’s primary immune cells, and they perform essential roles in maintaining healthy cognitive function. In Alzheimer’s disease, however, the role of microglia becomes complicated. Elevated levels of TIM-3 inhibit their function, preventing the clearing of amyloid beta plaques that contribute to cognitive decline. Understanding this relationship highlights the need for innovative strategies, such as TIM-3 therapy, to restore normal microglial activity without compromising their critical functions in the brain.
In the context of Alzheimer’s disease research, it is crucial to explore the dual role of microglia not only in plaque removal but also in synaptic pruning and maintaining neurological health. Typically, microglia help eliminate excess synapses, fine-tuning circuits critical for memory and learning. With aging and the onset of Alzheimer’s, however, their function becomes impaired due to molecular signals like TIM-3, underscoring the significance of targeting these pathways for therapeutic interventions.
The Connection Between the Immune System and Alzheimer’s Disease
Emerging findings emphasize the intricate connection between the immune system and Alzheimer’s disease progression. As checkpoint molecules such as TIM-3 regulate immune responses, they can also impact the brain’s susceptibility to plaque accumulation. By understanding how the immune system interacts with Alzheimer’s pathology, researchers can identify new therapeutic avenues to modulate these interactions and potentially enhance cognitive function in patients.
Research into the immune system’s role in Alzheimer’s disease further underscores the potential for developing innovative treatments that can simultaneously address neuroinflammation and cognitive decline. By leveraging knowledge from cancer immunotherapy, where checkpoint inhibitors have shown promise, similar strategies may enhance the body’s immune response in combating Alzheimer’s, as studies suggest TIM-3 blockade could lead to improved microglial activity and plaque clearance.
Cognitive Function Improvement through TIM-3 Inhibition
The inhibition of TIM-3 has been associated with significant improvements in cognitive function in experimental models of Alzheimer’s disease. By allowing microglia to resume their natural role in clearing amyloid plaques, cognitive behaviors in mice were restored, resembling conditions prior to plaque accumulation. This breakthrough suggests that TIM-3 may be a critical target for therapeutic intervention aimed at not only halting progression but also reversing some cognitive deficits associated with Alzheimer’s.
Strategies focused on TIM-3 inhibition pave the way for a new class of Alzheimer’s treatments. These could potentially yield substantial benefits, especially considering the limited success of existing therapies. By prompting microglial activation, TIM-3 targeted treatments may restore cognitive abilities, offering hope where other strategies have fallen short. As pharmaceutical advancements progress, this mechanism holds promise for enhancing the quality of life for Alzheimer’s patients.
Current Strategies in Alzheimer’s Disease Research
Amid numerous drug trial failures in Alzheimer’s treatment, novel strategies leveraging immune pathways are gaining traction. Research focusing on checkpoint molecules like TIM-3 represents a paradigm shift in the understanding of Alzheimer’s pathology, providing fresh insights into manipulating the immune response to facilitate plaque clearance. Trials assessing the effectiveness of TIM-3 inhibitors are anticipated to yield critical data that could lead to viable solutions for challenging Alzheimer’s cases.
The emphasis on immune modulation through TIM-3 therapy underscores a broader trend in Alzheimer’s disease research that seeks to identify and exploit immune checkpoints for potential cognitive intervention. As new findings emerge, the prospect of integrating immunotherapy alongside conventional approaches may redefine treatment methodologies, creating a more comprehensive arsenal to combat Alzheimer’s and improve patient outcomes.
Future Implications of TIM-3 Research in Alzheimer’s Therapy
The implications of TIM-3 research are far-reaching and may transform Alzheimer’s therapeutics. As scientists explore the potential of TIM-3 inhibition, they are starting to bridge knowledge from immunology and neuroscience, potentially leading to groundbreaking treatments for Alzheimer’s that harness the body’s own immune responses. This could not only mitigate symptoms but also address the underlying mechanisms contributing to the disease, promising a future where Alzheimer’s can be effectively managed.
Looking ahead, the size and scope of ongoing studies into TIM-3 signaling pathways are crucial for determining the precise effects on human populations. Current investigations involving mouse models will help refine these treatment modalities, bringing researchers closer to human clinical applications. By understanding how TIM-3 inhibition can enhance microglial functionality, future therapies might significantly alter the landscape of Alzheimer’s disease management.
Mechanisms of Alzheimer’s Disease Progression
The mechanisms driving Alzheimer’s disease progression are complex and multifaceted, involving a range of biological processes. Central to this is the accumulation of amyloid plaques, which are not effectively cleared by microglia due to inhibitory signals like TIM-3. This accumulation leads to neuroinflammation and neuronal damage, underscoring the importance of understanding how to manipulate these pathways for effective treatment.
Research into the molecular intricacies of Alzheimer’s disease reveals the role of genetic factors in influencing disease severity and progression. Studies have shown that a heightened expression of TIM-3 in individuals with the disease correlates with cognitive decline, suggesting that targeting this molecule could restore lost cognitive functions. Comprehensive exploration of these mechanisms is vital for deciphering potential therapeutic interventions.
Clinical Trials and the Future of Alzheimer’s Treatments
The journey toward effective Alzheimer’s treatments is increasingly focused on clinical trials investigating TIM-3 inhibitors. With early results demonstrating promising outcomes in pre-clinical models, there is optimism about advancing these therapies to human trials. The unique role of TIM-3 in modulating immune responses presents a compelling case for its potential in restoring cognitive function and improving quality of life for patients.
As clinical trials continue to unfold, researchers are assessing not only efficacy but also long-term effects of TIM-3 targeted therapies. Understanding the pharmacodynamics and safety profile of these inhibitors will be paramount as they move toward approval processes. Future research directions will undoubtedly focus on optimizing these therapies to maximize benefits for Alzheimer’s patients and provide new hope in the fight against this debilitating disease.
Challenges and Considerations in Alzheimer’s Research
Despite the exciting prospects of TIM-3 as a therapeutic target in Alzheimer’s disease, challenges remain. Understanding the specific mechanisms by which TIM-3 affects microglial activity is crucial, as overly tampering with immune responses could lead to unforeseen consequences, including potential neuroinflammation. Balancing efficacy with safety is paramount in this evolving research landscape.
Furthermore, the variability of Alzheimer’s presentation among patients complicates the development of universally applicable treatments. As researchers strive to tailor TIM-3 therapies to individual genetic profiles, personalized approaches may emerge, maximizing effectiveness and minimizing risks. Continued exploration of the immune system’s role in Alzheimer’s will be critical for overcoming these hurdles and advancing therapeutic strategies.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s targets the TIM-3 molecule, which inhibits microglia, the brain’s immune cells, from clearing amyloid plaques. By blocking TIM-3, this therapy frees microglia to attack and remove these plaques, which can improve cognitive function and memory.
How does TIM-3 relate to Alzheimer’s disease research?
TIM-3 is linked to late-onset Alzheimer’s disease through genetic studies. Research has shown that high TIM-3 expression on microglia leads to reduced plaque clearance, making it a significant target in Alzheimer’s disease research for restoring cognitive function.
Could TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Yes, TIM-3 therapy has been demonstrated to enhance cognitive function in animal models of Alzheimer’s. By allowing microglia to effectively clear amyloid plaques, TIM-3 inhibition may lead to memory improvement in patients.
What role do microglia play in TIM-3 therapy for Alzheimer’s?
Microglia are the immune cells of the brain responsible for clearing away harmful plaques. In TIM-3 therapy, inhibiting TIM-3 enables these crucial cells to attack amyloid plaques more effectively, which is essential for treating Alzheimer’s disease.
What are the implications of TIM-3 therapy for future cancer treatment strategies?
While TIM-3 therapy primarily focuses on Alzheimer’s, its approach of blocking immune checkpoint molecules may offer insights into developing more effective cancer treatment strategies by enhancing immune responses against tumors, given TIM-3’s role in regulating immune activity.
How long did the research into TIM-3 therapy for Alzheimer’s take?
The research on TIM-3 therapy for Alzheimer’s spanned five years, focusing on the genetic implications and the impact of TIM-3 on microglial function, leading to potential therapeutic applications in human conditions.
What evidence supports the effectiveness of TIM-3 therapy in Alzheimer’s?
Evidence from mouse models indicates that deleting the TIM-3 gene enhances plaque clearance and improves cognitive behaviors. This suggests that TIM-3 therapy could be a viable option to improve cognitive function in Alzheimer’s patients.
What is the next step in TIM-3 therapy research for Alzheimer’s patients?
The next step is testing human anti-TIM-3 antibodies in mouse models of Alzheimer’s to evaluate their effectiveness in preventing plaque formation, paving the way for clinical applications in treating Alzheimer’s disease.
Is TIM-3 only relevant for Alzheimer’s disease or can it be applied to other conditions?
While TIM-3 is particularly relevant in Alzheimer’s disease due to its role in immune regulation and plaque clearance, its mechanisms may also provide insights for other neurodegenerative conditions and autoimmune diseases where immune checkpoints are involved.
What challenges exist in delivering TIM-3 therapy to human patients with Alzheimer’s?
Challenges include ensuring that TIM-3 inhibitors effectively reach the brain, as some therapies targeting amyloid plaques have previously failed due to vascular complications. Research is focusing on developing targeted therapies that minimize risks while maximizing therapeutic effects.
| Key Points | Details |
|---|---|
| TIM-3 Therapy for Alzheimer’s | The therapy utilizes TIM-3 molecule deletion to enhance clearance of plaques and restore memory. |
| Study Findings | Mice without TIM-3 had improved memory as microglia could clear Alzheimer’s plaques. |
| Role of TIM-3 | TIM-3 inhibits microglia from attacking harmful amyloid plaques in the brain. |
| Research Duration | The study took five years, involving multiple experiments and collaborators. |
| Potential Human Application | Proposed treatments include anti-TIM-3 antibodies or small molecules to block TIM-3’s function. |
Summary
The research into TIM-3 therapy for Alzheimer’s disease offers promising insights into potential new treatment avenues. By deleting the TIM-3 molecule, scientists can free microglial cells in the brain to clear away harmful plaques, resulting in improved cognitive functions in affected models. This groundbreaking approach not only highlights the interconnectedness of immune checkpoints in both cancer and Alzheimer’s, but it also reinforces the potential of TIM-3 as a viable target for therapeutic intervention, making TIM-3 therapy a noteworthy consideration in the battle against Alzheimer’s.