
Neurological Basis of Social Connection: Key Insights Revealed
The neurological basis of social connection is becoming increasingly recognized as a vital component of human health and well-being. Health professionals assert that social connection is as essential as food and water, forming a key aspect of our mental health and social needs. Recent research has illuminated how our brains are wired to seek companionship, revealing the intricate biological basis of social behavior. As loneliness reaches epidemic proportions, understanding the neurological mechanisms behind our need for social interaction could illuminate the profound effects of isolation on health. This exploration not only underscores the importance of social bonds but also paves the way for innovative approaches to enhance mental wellness.
Understanding the brain’s role in fostering interpersonal relationships sheds light on our intrinsic need for companionship and human interaction. The intricate interplay of neural pathways and circuits that drive social engagement reveals much about the psychological underpinnings of social behavior. With a growing recognition of the effects of loneliness on mental well-being, it’s evident that our biological mechanisms are finely tuned to facilitate social connections. By investigating these neural architectures, we can better comprehend how a lack of social interaction not only affects individuals but society as a whole. Ultimately, this exploration into our social nature offers insights critical for addressing the mental health challenges we face today.
The Biological Basis of Social Connection
Understanding the biological basis of social connection is crucial for uncovering the underlying needs that drive human behavior. Research indicates that social interactions activate specific neural circuits in the brain, much like our responses to hunger and thirst. These neural pathways, particularly in the hypothalamus, dictate our social needs and can illuminate how essential them are for our health, thus positioning social connection on the same level as essential needs such as food and water.
Recent studies underscore that social connection isn’t merely an emotional experience; it has a biological foundation. By studying neural activities associated with social behavior, scientists can reveal how deficits in social interactions lead to mental health issues. Essentially, isolation can trigger an adverse reaction in the brain, manifesting as a form of distress that can be comparable to physical pain. Such insights are pivotal in understanding how our mental health is intricately tied to our social interactions.
Frequently Asked Questions
What is the neurological basis of social connection in humans?
The neurological basis of social connection in humans involves the interactions of specific brain regions, particularly the hypothalamus, which governs the instinctive need for social interaction. Recent research reveals that social needs are encoded similarly to basic physiological needs like hunger and thirst, driven by neural circuits that regulate both desire for companionship and responses to social isolation.
How does social interaction impact mental health and social needs?
Social interaction plays a crucial role in mental health as it satisfies intrinsic social needs similar to other basic human needs. Engaging in regular social contact can mitigate feelings of loneliness, which is linked to various mental health issues such as depression and anxiety. Understanding the neurological basis of this need for social connection helps explain its profound impact on overall well-being.
What are the effects of loneliness on health in relation to social connection?
Loneliness has several detrimental effects on health, including increased risk of chronic diseases, mental health disorders, and even early mortality. The neurological basis of social connection highlights how disruptions in social interactions can lead to feelings of isolation, triggering neural responses that negatively affect both psychological well-being and physical health.
What role do touch and sensory inputs play in the biological basis of social behavior?
Touch and sensory inputs are critical components of social behavior, as studies show that physical interactions, such as hugging or handshakes, significantly enhance social bonds. The neurological basis of social connection involves the brain’s response to tactile stimuli, indicating that physical closeness and interaction fulfill essential social needs that contribute to mental health.
How do researchers study the biological basis of social behavior in animals?
Researchers study the biological basis of social behavior in animals by isolating subjects and observing their neural activity in response to social deprivation and reunion phases. For instance, mice have been used in studies to identify which neurons are activated during these phases, providing insights into the fundamental mechanisms governing social connection and the drive for interaction.
What can the neurological insights into social connection tell us about human interactions today?
Neurological insights into social connection suggest that as our social interactions increasingly occur through digital mediums, we may be missing vital elements like physical touch. This study reinforces the importance of face-to-face interactions for maintaining mental health and fulfilling our biological need for social engagement, emphasizing the need for genuine human contact in an increasingly isolated world.
| Key Point | Details |
|---|---|
| Social Connection as a Basic Need | Health professionals recognize social contact as a fundamental need, comparable to food and shelter. |
| Public Health Concern | The U.S. Surgeon General has emphasized social isolation as a critical public health issue. |
| Research Focus | A study published in Nature investigates how the brain encodes the need for social interaction. |
| Hypothalamus Role | Researchers identified the hypothalamus as key in regulating social behavior akin to hunger and thirst. |
| Mechanisms of Social Drive | The desire for social interaction may stem more from a need to avoid negative feelings than from a desire for pleasure. |
| Isolation Effects | Prolonged isolation can lead to a dislike of social interactions in mice, highlighting the complex impact of loneliness. |
| Importance of Touch | Touch is vital for fulfilling social needs, influencing behavioral preferences in mice and, potentially, humans. |
| Implications for Human Behavior | Understanding the neurological basis of social connection can inform us about its psychological impacts and the importance of social bonds in mental health. |
Summary
The neurological basis of social connection reveals that human social needs are intricately connected to our basic survival instincts, much like hunger and thirst. Research indicates that our brains are wired to seek companionship, emphasizing that social interaction is not merely a source of pleasure, but also an essential element for mental health. With rising concerns about social isolation, the findings of this research underscore the critical nature of fostering social connections in our increasingly digital world. Understanding the mechanisms behind these needs can help improve mental health strategies and enrich our interpersonal relationships.
How Much Sleep Do You Need? Expert Insights and Tips
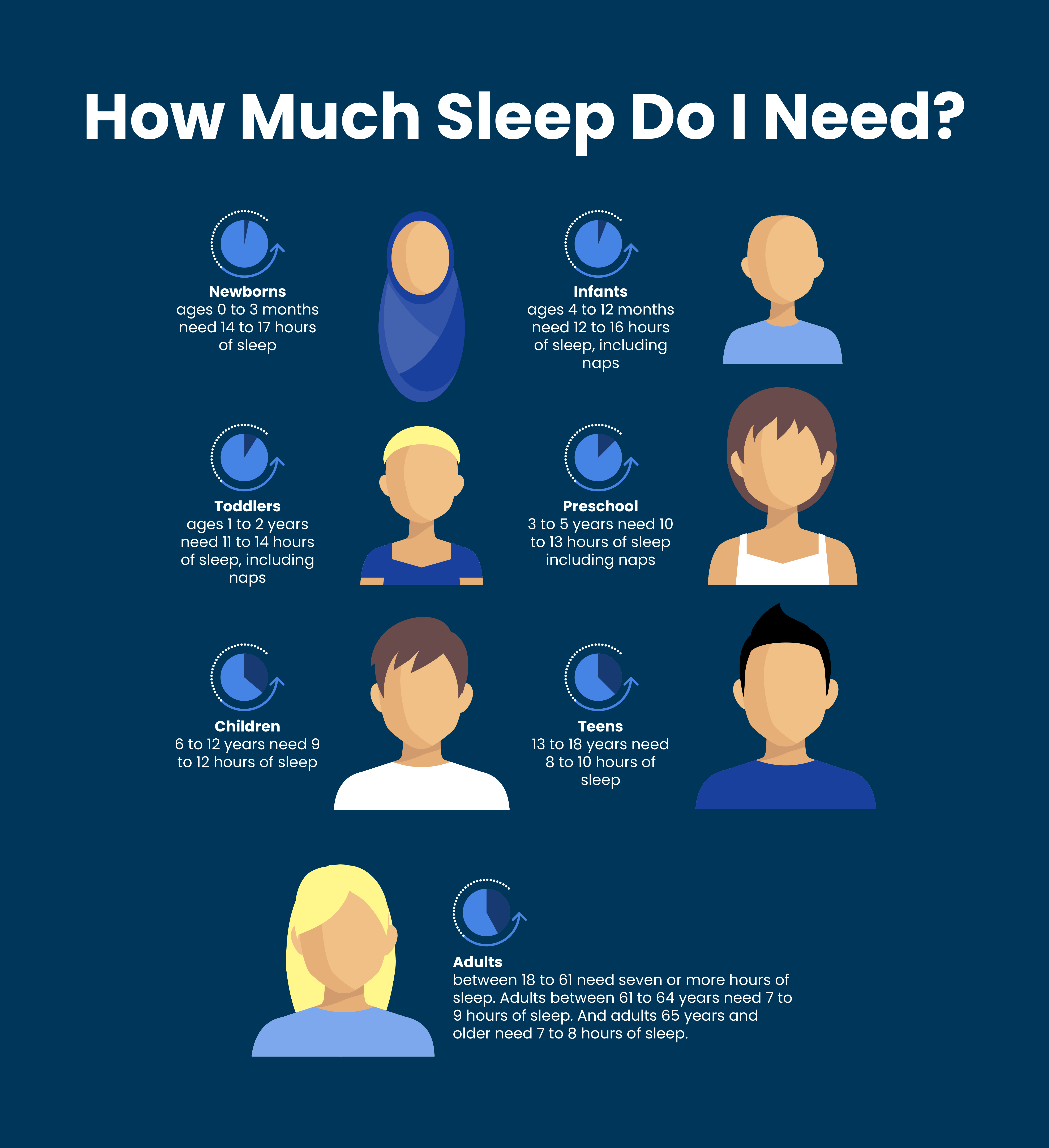
When pondering how much sleep do you need, it’s essential to recognize the significant role that adequate rest plays in overall well-being. Most adults require between seven to nine hours of quality sleep each night to function optimally; however, individual needs can vary. Poor sleep can lead to various health issues, emphasizing the importance of sleep in maintaining both physical and mental wellness. Exploring effective sleep tips like establishing a consistent sleep schedule can dramatically improve your rest quality. If you struggle with insomnia solutions or lingering fatigue, consulting a sleep doctor may provide the guidance you need to reclaim restorative sleep.
Understanding the necessary amount of nightly rest is crucial for optimal health and vitality. Many wonder about their personal sleep requirements or what factors contribute to a good night’s sleep. Recognizing the need for a tailored sleep routine can enhance your overall quality of life. This discussion encompasses everything from sleep cycles to the effects of environment on restfulness. By addressing points such as sleep hygiene and scheduling, you can pinpoint what your body truly requires for rejuvenation at night.
Understanding Individual Sleep Needs
The amount of sleep necessary for optimal functioning varies significantly from person to person. A common benchmark is the recommended seven to nine hours per night for adults, but self-awareness plays a crucial role in understanding your own needs. Monitoring sleep without the interruption of an alarm clock can provide insights into how much rest your body genuinely requires. This period of observation can reveal patterns, helping you to ascertain whether you’re feeling rested after several nights of uninterrupted sleep.
In addition to monitoring sleep duration, it’s also vital to evaluate sleep quality. Quality sleep involves experiencing a full range of sleep stages, particularly REM and deep sleep, which are essential for physical and mental health. If you’re consistently waking up feeling unrefreshed, it might indicate a need to adjust your sleep habits or review your sleep environment. Factors such as light exposure, room temperature, and noise levels can all impact sleep quality significantly.
How Much Sleep Do You Need?
So, how much sleep do you need for optimal health and functioning? While the average adult requires about 7-8 hours, this can vary based on individual lifestyle, health conditions, and age. Younger individuals, particularly teens, often require more sleep due to their developmental needs. Therefore, adjusting your sleep schedule to align with your personal requirements is essential for improving your overall sleep quality. Tracking your sleep habits through a journal or an app can help you determine your unique sleep needs.
In addition to duration, the timing of sleep matters. Establishing a consistent sleep-wake schedule reinforces your body’s natural circadian rhythms, making it easier to fall asleep and wake up. Irregular sleep patterns can lead to increased grogginess and additional health complications, such as cardiovascular issues. For long-term well-being, aim for a regular sleep schedule, and consider avoiding caffeine and electronics before bedtime to enhance your chances of getting restorative sleep.
The Importance of Sleep for Overall Health
Understanding the importance of sleep is vital for both physical and mental health. Studies have shown that inadequate or poor quality sleep can lead to a myriad of health issues, including weakened immune function, increased risk of chronic diseases such as diabetes and heart disease, and mental health disorders like anxiety and depression. Sleep is the body’s natural recovery system, allowing for cellular repair and overall rejuvenation.
Furthermore, sleep plays a critical role in cognitive functions such as memory consolidation, learning, and problem-solving abilities. A lack of sleep can hinder performance, affecting your ability to concentrate and make decisions. Prioritizing sleep is crucial for increased productivity and overall wellness, making sleep hygiene practices and a healthy sleep environment key components of lifestyle improvements.
Effective Sleep Tips for Better Rest
Implementing effective sleep tips can transform your nighttime routine and enhance sleep quality. Establish a calming pre-sleep regimen by engaging in relaxing activities such as reading, meditation, or gentle stretching. Avoiding stimulants like caffeine and electronic devices close to bedtime can also make a significant difference in your ability to fall asleep. Creating an inviting sleep environment, with factors such as darkness, quietness, and comfortable bedding, further encourages restful sleep.
In addition, physical activity during the day has been linked to better sleep at night. Regular exercise can help alleviate sleep disturbances and make it easier to fall asleep. However, be mindful of the timing; working out too close to bedtime may have the opposite effect and energize your body rather than tire it out. Consistency in your sleep practices is vital, so try to go to bed and wake up at the same time every day, even on weekends.
Common Sleep Disorders: When to Seek Help
If you’re consistently waking up feeling tired despite spending enough time in bed, it might be time to address potential underlying sleep disorders. Conditions such as insomnia, sleep apnea, or restless leg syndrome can drastically affect sleep quality and overall health. Symptoms such as snoring, gasping for air during sleep, or experiencing prolonged difficulty falling asleep warrant consultation with a sleep doctor for proper diagnosis and treatment.
Recognizing patterns like waking frequently during the night or experiencing excessive daytime sleepiness can indicate that something isn’t right with your sleep cycle. Consulting a healthcare professional for insomnia solutions could lead to tailored interventions, including cognitive behavioral therapy, medication, or lifestyle adjustments. Early intervention can dramatically improve your quality of life, enhancing your energy levels during the day.
The Role of Sleep Hygiene in Quality Rest
Sleep hygiene refers to practices that promote consistent and quality sleep. This includes maintaining a comfortable sleep environment, establishing a regular bedtime routine, and recognizing the factors that may disrupt your sleep patterns, like irregular schedules or stress. Good sleep hygiene not only encourages the quantity of sleep but also improves its quality, which is crucial for cognitive and physiological health.
Additionally, avoiding food and drink that could upset your stomach before bed—such as heavy meals, spicy foods, and alcohol—can prevent disruptions in your sleep cycle. Similarly, developing calming habits, such as taking a warm bath or using a white noise machine, can help signal to your body that it is time to wind down. These practices can work wonders in creating a sleep-inducing atmosphere.
Understanding Sleep Stages and Their Impact
To appreciate how much sleep you need, it’s essential to understand sleep stages. Sleep is divided into two main types: REM (rapid eye movement) and non-REM sleep. Each of these stages plays a vital role in physical recovery and cognitive function. Non-REM sleep helps in physical repair, while REM sleep contributes to memory consolidation and learning processes.
Cycles of sleep stages occur throughout the night, and disruptions can lead to feeling unrefreshed and drowsy the next day. Understanding your sleep architecture can help you create conditions that promote deeper sleep stages. Using wearable devices or sleep apps can provide insights into how well you are progressing through these stages and help identify areas for improvement.
Navigating Sleep Supplements and Their Efficacy
Many people turn to sleep supplements like melatonin to promote relaxation and enhance sleep quality. However, it’s essential to approach sleep aids with caution. Not all supplements are created equal; for example, melatonin is unregulated, meaning the dosage and purity can significantly vary between products. It may be beneficial to consult with a healthcare provider to discuss your needs before trying any sleep aids.
While some individuals find success with over-the-counter sleep medications, long-term reliance on them is generally discouraged. Cognitive Behavioral Therapy for Insomnia (CBT-I) offers proven therapeutic solutions for individuals struggling with sleep issues, focusing on changing the thoughts and behaviors that contribute to sleep difficulties. This approach tends to yield more sustainable results for long-term sleep improvement.
The Benefits of Napping and its Timing
Napping can serve as a valuable tool for those who struggle to get enough sleep at night. Short naps, ideally between 10-30 minutes, can improve alertness and performance without leading to sleep inertia—feeling groggy after waking. However, timing is crucial; napping too late in the day can interfere with nighttime sleep schedules and contribute to difficulties falling asleep when it matters most.
For night shift workers or individuals with irregular schedules, strategic napping can be a beneficial practice to offset sleep deprivation. However, ensuring naps occur at well-timed intervals that don’t disrupt the sleep-wake cycle will help maintain overall sleep health. Incorporating brief, refreshing naps can enhance productivity and mood, making them a valuable addition to a balanced daily routine.
Frequently Asked Questions
How much sleep do you need to feel rested?
The amount of sleep you need varies by individual. A good starting point is to see how much sleep you naturally get without an alarm clock. This duration, typically measured over a few days, can indicate how much sleep you truly need to feel rested.
What is the importance of sleep for overall health?
The importance of sleep cannot be overstated. Adequate sleep supports cognitive function, emotional well-being, and physical health. Insufficient sleep can lead to various health issues, making it crucial to prioritize a proper sleep schedule.
How can sleep tips improve your sleep schedule?
Incorporating sleep tips such as establishing a consistent bedtime, limiting caffeine intake, and creating a calming pre-sleep routine can significantly improve your sleep schedule, helping you achieve the restorative sleep you need.
When should you see a sleep doctor about how much sleep you need?
If you consistently wake up feeling unrefreshed, even after several nights of what you believe is adequate sleep, consider consulting a sleep doctor. This may indicate underlying conditions such as insomnia or sleep apnea that require professional attention.
What are common insomnia solutions that can help with sleep?
Common insomnia solutions include cognitive behavioral therapy for insomnia, maintaining a consistent sleep environment, and practicing relaxation techniques. These strategies can help improve your ability to fall asleep and stay asleep, meeting your personal sleep needs.
How does changing your sleep schedule affect how much sleep you need?
Changing your sleep schedule can affect how much sleep you need since your body adapts to new routines over time. Gradually adjusting your bedtime can help recalibrate your sleep needs and promote better sleep patterns.
How much sleep do you need if you’re working a night shift?
If you’re working the night shift, you typically need about 7-9 hours of sleep during the day, though some individuals might require more. It’s important to establish a dark, quiet sleeping environment to optimize your rest.
Are there specific sleep tips to avoid insomnia?
Yes, to avoid insomnia, implement the following sleep tips: maintain a stable sleep schedule, create a relaxing pre-bed routine, limit screen time before bed, and avoid caffeine and heavy meals in the evening. These strategies can help enhance sleep quality.
| Aspect | Details |
|---|---|
| General Sleep Needs | Sleep needs vary by individual and are often determined by how much one sleeps without an alarm. |
| Indicators of Sleep Quality | Waking up feeling unrefreshed, despite achieving the recommended hours, may necessitate consulting a sleep doctor. |
| Advice for Better Sleep | To aid sleep, engage in calming activities before bed and avoid caffeine or stimulating media. |
| Melatonin | Melatonin is an unregulated supplement. It’s advised to seek pharmaceutical-grade options if considering its use. |
| Other Sleep Aids | Cognitive behavioral therapy is recommended for long-term insomnia solutions over pills, which should only be short-term. |
| Accessories for Sleep | Sleep podcasts, sound machines, eye masks, and earplugs can be beneficial, provided they don’t obstruct alarms or safety signals. |
Summary
How much sleep do you need? It varies for each individual, but understanding your sleep patterns and prioritizing quality rest is essential. Engaging in calming pre-sleep activities, recognizing sleep issues, and seeking professional advice when necessary can significantly improve sleep quality. Remember to consider factors like melatonin regulation and behavioral therapies for long-term solutions to sleep difficulties.

Heart Disease Prevention: Why You Should Take It Seriously
Heart disease prevention is becoming an increasingly crucial focus in today’s healthcare landscape as cardiovascular disease continues to be the leading cause of death in the United States. Despite significant medical advancements, many individuals remain indifferent to the dangers posed by heart disease, often dismissed as a lesser threat compared to more immediate concerns like cancer. Experts like Ami Bhatt from the American College of Cardiology emphasize the importance of proactive measures, such as cholesterol management and regular health screenings, to mitigate risks associated with cardiovascular health. Effective prevention strategies not only include lifestyle changes but also the thoughtful use of cholesterol-lowering medications and guidance from preventive cardiology specialists. By prioritizing heart health today, individuals can significantly reduce the likelihood of needing heart disease treatment in the future, fostering a culture of awareness and prompt action.
When discussing the topic of heart health, it’s vital to recognize the broader implications of cardiovascular wellness. This includes understanding preventive cardiology, which provides actionable insights into reducing risks associated with heart disease, often influenced by factors like cholesterol levels and overall lifestyle choices. Many healthcare providers advocate for early intervention through lifestyle adjustments and appropriate medical treatment, particularly addressing issues like high LDL cholesterol. Additionally, the approach to heart disease encompasses educational efforts surrounding the long-term benefits of maintaining cardiovascular health from a young age. By fostering awareness so that patients view cardiovascular disease as an urgent health concern, we can shift attitudes and inspire more proactive health management.
Understanding Heart Disease Prevention
Heart disease prevention is critical to steering clear of the leading cause of death in the nation. Many individuals underestimate the severity of cardiovascular disease, often postponing necessary lifestyle changes or medical interventions. Unlike the urgent reactions often associated with cancer diagnoses, heart disease does not incite the same level of alarm, which can lead to a dangerous complacency. This mindset perpetuates the cycle of neglecting preventative measures, putting millions at risk. Effective heart disease prevention includes early recognition of risk factors, such as high cholesterol and hypertension, which can silently accumulate over time.
To counter this complacency, healthcare professionals advocate for increased awareness regarding cardiovascular health, emphasizing regular screening and proactive management. Engaging patients in discussions about cholesterol management, lifestyle changes, and the importance of preventive cardiology can significantly alter their perception of risk. Patients must be encouraged to monitor their cholesterol levels, blood pressure, and overall health metrics to facilitate timely interventions, thus preventing the progression of heart disease before it manifests severely.
The Role of Cholesterol Management in Heart Health
Cholesterol management is a cornerstone of maintaining cardiovascular health. High levels of LDL cholesterol, or ‘bad’ cholesterol, can lead to plaque buildup in the arteries, increasing the risk of heart disease and stroke. Understanding one’s cholesterol profile is essential, as it can serve as a predictive indicator of heart health. For individuals with family histories of heart disease or those classified as at-risk, incorporating cholesterol-lowering medications at an early stage can lead to remarkable outcomes in reducing cardiovascular events. Statins, a common class of cholesterol-lowering drugs, are underutilized due to patient skepticism, despite mounting evidence of their benefits.
Furthermore, lifestyle modifications that promote optimal cholesterol levels should not be overlooked. Diet plays a significant role, with a focus on heart-healthy foods that can lower cholesterol naturally. Options like oats, fatty fish, nuts, and legumes can all contribute positively. Patients must be educated about these choices alongside medication options; integrating both can lead to better management of cholesterol levels and overall cardiovascular health, bridging the gap between treatment and prevention.
Advancements in Heart Disease Treatment
Advancements in heart disease treatment have been pivotal in improving patient outcomes. Innovations such as minimally invasive surgical techniques and the use of artificial intelligence in diagnosis and personalized patient care are changing the landscape of cardiovascular treatment. New strategies, such as preserving the beating heart during transplants and performing complex procedures through small incisions, have led to shorter recovery times and enhanced patient experiences. As these advancements continue to unfold, they present new avenues for addressing the chronic issues of cardiovascular disease effectively.
Moreover, the integration of wearable technology has empowered patients by providing real-time data on various health metrics. This accessibility encourages them to take charge of their health journey, fostering a proactive approach towards heart disease management. However, despite these remarkable developments, the challenge remains in encouraging patients to act on preventive measures and support for ongoing treatment adherence. A holistic approach requires not only cutting-edge technology but also robust patient education and engagement to maximize the effectiveness of new treatments.
Preventive Cardiology: A Shift in Focus
Preventive cardiology marks a transformative approach that emphasizes the significance of prevention over treatment. This paradigm shift focuses on the identification of risk factors at an early age, promoting the importance of regular check-ups and lifestyle management as the first line of defense against heart disease. Engaging patients in conversations about their health, metrics such as blood pressure and cholesterol, and the latent dangers of complacency can be life-saving. Cardiovascular specialists advocate for a proactive stance where treatment becomes less about reaction and more about prevention.
This preventive strategy must address the psychological barriers patients face when confronted with their risk factors. Many do not perceive themselves at risk until it is too late; hence, generating awareness through community outreach initiatives, educational programs, and one-on-one coaching may encourage individuals to prioritize their heart health. Through the implementation of navigators who assist patients in managing their health, we can significantly improve adherence to preventive measures and ensure timely follow-ups, creating a seamless continuum of care.
The Impact of Lifestyle Choices on Cardiovascular Health
Lifestyle choices hold significant sway over cardiovascular health outcomes. Factors such as diet, physical activity, smoking, and alcohol consumption contribute extensively to an individual’s risk for heart disease. Maintaining a balanced diet rich in vegetables, whole grains, and healthy fats while limiting processed foods and sugars can greatly affect cholesterol levels and overall heart health. Moreover, incorporating regular physical activity not only combats obesity but also enhances heart function and lowers blood pressure, making it a non-negotiable element of prevention.
However, altering long-standing habits can pose challenges for many. Educating patients about the direct correlation between their lifestyle choices and heart disease can inspire change. Programs designed to motivate individuals to increase their physical activity and adopt healthier eating habits yield positive results and can save lives. Therefore, addressing these lifestyle factors through both individual and community initiatives is essential for promoting lasting behavioral changes that enhance cardiovascular health.
The Importance of Regular Health Screenings
Regular health screenings serve as crucial checkpoints in the prevention of heart disease. Many individuals are unaware of their risk factors and the silent nature of conditions like high cholesterol and high blood pressure until significant damage has occurred. By scheduling consistent check-ups, patients gain insights into their cardiovascular health, allowing for early intervention and management. Screenings can detect anomalies in key indicators such as LDL cholesterol levels and blood pressure, facilitating timely treatment options that may include lifestyle changes or medications.
Furthermore, healthcare providers can also leverage these appointments as opportunities to educate patients on risk factors and the importance of maintaining healthy habits. Emphasizing the cumulative effect of long-term neglect versus immediate action can motivate individuals to take their health seriously. Significantly, these regular screenings should not be perceived as mere formalities but essential components of a proactive approach to heart disease prevention and management.
Emerging Technologies in Cardiovascular Care
Emerging technologies are reshaping cardiovascular care dynamics, introducing fresh possibilities in both treatment and prevention. Advances in artificial intelligence are allowing for more precise risk assessments, enabling physicians to tailor their approach to individual patients effectively. Moreover, wearable technology and mobile health applications are empowering patients by providing tools to monitor their cardiovascular metrics and receive timely feedback. These innovations are invaluable as they contribute to a significant shift towards personalized medicine, enhancing the patient experience and improving health outcomes.
However, as promising as these technologies are, it is important to balance their usage with traditional health assessments and personal interactions with healthcare professionals. The human element in medical care remains critical, and integrating technology into a compassionate healthcare framework can lead to the best outcomes. Ensuring that patients understand how to utilize these technologies and interpret their data correlates with improved adherence to treatment plans and lifestyle changes critical in heart disease prevention.
Community Outreach and Education for Heart Health
Community outreach and education programs play a vital role in enhancing public awareness of heart disease and its prevention. By facilitating workshops, screening events, and informational sessions, healthcare organizations can equip individuals with the knowledge necessary to make informed decisions about their heart health. Understanding risk factors, the importance of cholesterol management, and available treatment options fosters a culture of prevention that can, in turn, reduce the incidence of heart disease across populations.
Additionally, these outreach initiatives are crucial for addressing misconceptions surrounding heart health and barriers to accessing care. Empowering individuals through education encourages more proactive health behaviors, which is especially important in communities disproportionately affected by cardiovascular disease. Such comprehensive approaches ensure that everyone has access to essential information, leading to increased screenings, early detection, and treatment adherence, ultimately saving lives and improving community health outcomes.
Patient Engagement Strategies for Better Outcomes
Engaging patients in their own healthcare journey is essential for fostering adherence to treatment plans and improving cardiovascular health outcomes. Strategies to enhance patient engagement may include personalized follow-up communications, education on managing risk factors, and the introduction of support systems such as peer groups or health advocates. By creating an environment where patients feel supported and heard, healthcare providers can significantly improve compliance with medication regimens and lifestyle changes essential for heart disease prevention.
Moreover, acknowledging the unique challenges patients face—such as busy schedules or confusion over medical jargon—can help healthcare professionals tailor their communication for clearer understanding. Engaging patients effectively also involves leveraging technology, such as patient portals and mobile apps, to facilitate easier access to health information and encourage active participation in their care. Ultimately, empowered and informed patients are more likely to make decisions that lead to better heart health outcomes and enhance their own quality of life.
Frequently Asked Questions
What are effective strategies for heart disease prevention?
Effective heart disease prevention strategies include maintaining healthy cholesterol levels, adopting a balanced diet low in saturated fats and high in fruits and vegetables, engaging in regular physical activity, managing stress, and avoiding tobacco use. Regular screenings for cholesterol, blood pressure, and diabetes are also crucial in preventive cardiology to ensure early detection and treatment.
How can cholesterol management aid in heart disease prevention?
Cholesterol management is vital for heart disease prevention as high levels of LDL or ‘bad’ cholesterol can lead to plaque buildup in arteries, increasing the risk of heart attacks and strokes. Implementing lifestyle changes such as dietary modifications, regular exercise, and possibly cholesterol-lowering medications can significantly reduce cholesterol levels and enhance cardiovascular health.
What role do cholesterol-lowering medications play in heart disease prevention?
Cholesterol-lowering medications, such as statins, play a significant role in heart disease prevention by reducing LDL cholesterol levels and stabilizing plaque in the arteries, which helps prevent cardiovascular events. These medications are often prescribed after assessing individual risk factors, as they can have profound benefits, especially for individuals with elevated cholesterol levels or a family history of heart disease.
Why is awareness of cardiovascular health important for heart disease prevention?
Awareness of cardiovascular health is crucial for heart disease prevention because many people overlook the gradual risk factors associated with heart disease, such as high cholesterol and hypertension. By understanding their health metrics and engaging in preventive care, individuals can take proactive steps to mitigate their risk and improve their overall heart health.
How often should one get screened for heart disease risk factors?
Individuals should start getting screened for heart disease risk factors, including cholesterol levels and blood pressure, around age 20, and more frequently thereafter based on family history and health conditions. Regular check-ups are essential to monitor these metrics, as early intervention can make a significant difference in heart disease prevention.
What lifestyle changes can assist in preventive cardiology?
Lifestyle changes that assist in preventive cardiology include adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats, maintaining a healthy weight, exercising regularly, managing stress levels, and refraining from smoking. These modifications collectively enhance cardiovascular health and are foundational to heart disease prevention.
How does stress impact heart disease prevention efforts?
Stress negatively impacts heart disease prevention efforts by contributing to unhealthy behaviors such as poor diet, lack of exercise, and smoking, which can elevate cholesterol levels and blood pressure. Managing stress through relaxation techniques, physical activity, and a supportive social network is essential for protecting against heart disease.
What innovations are improving heart disease treatment and prevention?
Innovations improving heart disease treatment and prevention include advancements in minimally invasive surgical techniques, the use of artificial intelligence for personalized patient care, and the development of new cardiovascular drugs. These breakthroughs enhance patient outcomes and enable more effective management of heart disease risk factors, including cholesterol and blood pressure.
Is heart disease prevention more effective when started at a younger age?
Yes, heart disease prevention is generally more effective when started at a younger age. Early awareness and management of risk factors like cholesterol levels, blood pressure, and lifestyle habits can significantly reduce the likelihood of developing heart disease later in life and improve overall cardiovascular health.
What role does patient education play in heart disease prevention?
Patient education plays a critical role in heart disease prevention by empowering individuals to understand their health metrics, the importance of screenings, and the impact of lifestyle choices on cardiovascular health. Educated patients are more likely to adhere to treatment plans, make healthier decisions, and engage in proactive management of their heart health.
| Key Points About Heart Disease Prevention | Factors | Insights | |
|---|---|---|---|
| Lack of Urgency | Many patients do not treat heart disease with the seriousness it deserves, unlike cancer diagnoses. | ||
| Awareness of Metrics | Patients are advised to monitor LDL cholesterol, blood pressure, weight, and sleep quality from a young age. | ||
| Innovative Treatments | New heart transplant methods and minimally invasive surgeries are improving recovery times. | ||
| Enhanced Patient Care | Utilizing navigators can improve patient adherence to treatment plans and follow-up. | ||
| Role of Technology | Wearable fitness trackers and new medications can empower patients in managing their health. | ||
Summary
Heart disease prevention is critical as cardiovascular disease remains the leading cause of death in the United States. Experts emphasize the need for patients to take proactive steps towards their heart health, including awareness of risk factors and regular screenings. By prioritizing heart disease prevention, individuals can significantly reduce their risk of serious health complications.
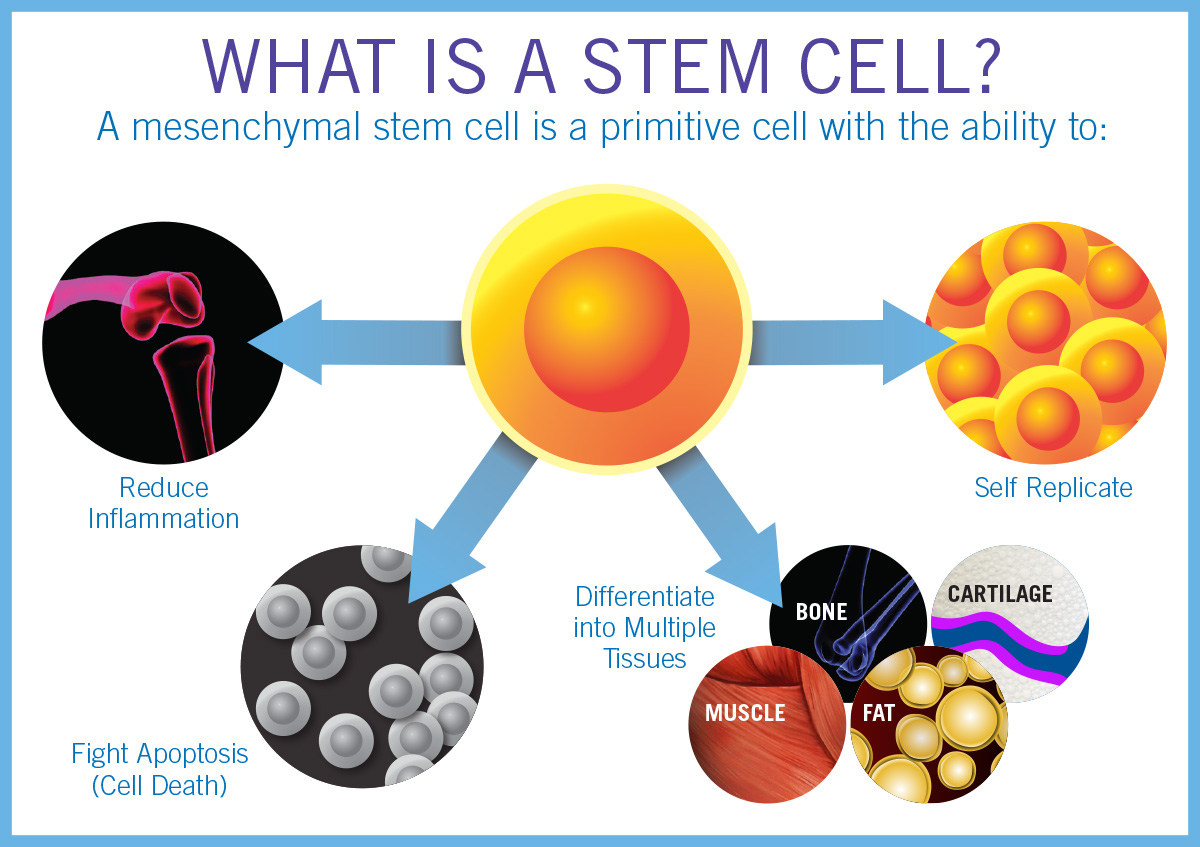
Stem Cell Therapy: A Breakthrough in Corneal Injury Treatment
Stem cell therapy is emerging as a revolutionary advancement in the medical field, particularly for the treatment of ocular conditions. Recently, clinical trials have demonstrated the efficacy of this innovative approach in restoring the cornea’s surface, offering hope to individuals suffering from corneal injuries once deemed untreatable. The procedure, known as cultivated autologous limbal epithelial cells (CALEC), involves the extraction of ocular stem cells from a healthy eye, which are then cultivated and transplanted into the damaged eye. This breakthrough treatment not only highlights the potential of ocular stem cells in eye damage recovery but also shows promise in redefining corneal injury treatment. With more than 90 percent success in restoring corneal surfaces observed in trial participants, the future of stem cell therapy in ophthalmology looks incredibly promising.
The topic of cellular regeneration within the eye, often referred to as ocular cell therapy, is gaining traction due to its potential to heal eye damage effectively. Techniques utilizing cultivated limbal epithelial cells are at the forefront of these advancements, specifically the CALEC procedure that draws from the body’s natural healing mechanisms. This innovative approach focuses on revitalizing the cornea after injury, tapping into the body’s own limbal epithelial cells to foster recovery. With a spotlight on new methods for repairing corneal damage, the landscape of eye care continues to evolve, providing new avenues for those facing vision loss. The continuous exploration of stem cell applications in this field may soon lead to more comprehensive treatments that can restore sight and alleviate suffering for patients globally.
Understanding Corneal Injury Treatment
Corneal injuries can result from various traumas, including chemical burns, infections, and physical trauma, leading to severe visual impairment. The cornea plays a crucial role in focusing light onto the retina, making its health vital for clear vision. Treatment for corneal injuries has traditionally focused on corneal transplants; however, this approach is not always possible due to limbal stem cell deficiencies that result from such injuries. Without a source of these cells, the corneal surface cannot regenerate, leading to chronic pain and visual difficulties for patients.
The traditional methods for treating corneal injuries have been limited, often leaving patients with few options besides corneal transplants that may not be viable due to the underlying limbal damage. Current advancements in corneal injury treatment, like the CALEC procedure, not only offer hope for restoration but also present a innovative approach to healing. By utilizing ocular stem cells harvested from a healthy eye, the CALEC procedure is paving the way towards more effective treatments that empower the regenerative potential of the eye.
The Importance of Limbal Epithelial Cells
Limbal epithelial cells are essential for maintaining the integrity of the cornea, responsible for the smooth surface that is critical for proper vision. Found at the border of the cornea and the sclera, these cells facilitate healing and regeneration when the cornea is injured. A deficiency in limbal epithelial cells can lead to a state where the cornea cannot regenerate, resulting in a myriad of complications, including chronic pain and severe vision impairments. Understanding their function is vital for developing successful treatments for corneal injuries.
The preservation and restoration of limbal epithelial cells through stem cell therapy can transform the landscape of ocular treatments. Cultivated autologous limbal epithelial cells (CALEC) involve harvesting these crucial cells from a healthy eye, which allows for the potential regeneration of the cornea in the affected eye. This innovative procedure not only circumvents the issues associated with traditional transplant surgeries but also aligns new hope for patients who have been previously deemed untreatable.
Exploring the role of limbal epithelial cells is paramount in advancing ocular treatments. As researchers build on the foundation laid by stem cell therapy, future studies aim to enhance the efficacy and availability of these treatments. By leveraging the natural regenerative capacity of the eye, practitioners can help restore vision and alleviate the suffering of many patients worldwide.
Exploring the CALEC Procedure
The Cultivated Autologous Limbal Epithelial Cells (CALEC) procedure exemplifies cutting-edge advancements in eye damage recovery. This innovative approach involves harvesting limbal epithelial cells from a healthy eye, expanding them in a lab setting, and eventually transplanting them into the injured eye. During a clinical trial, participants demonstrated significant improvement in corneal surface restoration, indicating the potential for CALEC to redefine treatment options for individuals with severe corneal injuries.
The success of the CALEC procedure hinges on its meticulous approach to cell harvesting and transplantation. By providing a tailored solution for each patient, this procedure offers a path to healing that emphasizes safety and efficacy. As the trial results reveal improved outcomes and a high safety profile, the CALEC procedure stands out as a revolutionary advancement that could set a new standard in treating corneal injuries and restoring vision.
Stem Cell Therapy: A Game Changer in Ophthalmology
Stem cell therapy represents a profound shift in the way we approach eye care and treatment for corneal injuries. By harnessing the regenerative capabilities of stem cells, particularly those derived from limbal epithelial cells, surgeons can offer a solution that promotes healing at a cellular level. The groundbreaking CALEC procedure exemplifies this advancement, providing hope where traditional methods fall short.
As clinical trials continue to showcase the safety and effectiveness of stem cell therapies, including the CALEC procedure, the landscape of ophthalmology is changing. Researchers are increasingly focused on developing comprehensive treatment plans that integrate these therapies, ensuring patients receive the best possible care. With potential applications beyond corneal injuries, stem cell therapy may very well define the future of eye health and recovery.
Advancements in Eye Damage Recovery
The journey of recovery from eye injuries has witnessed significant advancements in recent years, particularly through innovative treatments like the CALEC procedure. By utilizing stem cells, researchers have made remarkable progress in restoring the cornea’s surface, which was once deemed irreparable. This progress in eye damage recovery signifies a paradigm shift, offering patients renewed hope and improved quality of life.
Continued advances in eye damage recovery are fueled by rigorous clinical trials and a better understanding of ocular biology. Studies revealing high success rates in corneal restoration affirm the potential of stem cell applications in ophthalmology. As the scientific community furthers research on eye damage treatment and the CALEC procedure, the pathway towards broader applications in various ocular conditions becomes increasingly tangible.
The Role of Ocular Stem Cells in Healing
Ocular stem cells, particularly those found in the limbal region of the cornea, play a crucial role in the eye’s healing process. These cells primarily maintain the regenerative capacity of the corneal surface, enabling it to recover from injuries. When damage occurs, the depletion of limbal epithelial cells can lead to severe complications, but stem cell therapy offers a solution by replenishing these vital cells.
Research focusing on ocular stem cells enhances understanding of their unique qualities and potential therapeutic applications. Innovations such as the CALEC procedure leverage these cells’ natural regenerative properties, improving outcomes for patients with corneal injuries. By integrating stem cells into treatment protocols, the ophthalmic field looks forward to a future where healing is more effective and accessible.
Impact of the CALEC Procedure on Vision
The CALEC procedure has demonstrated a significant impact on vision restoration for patients suffering from corneal injuries. With high success rates in restoring the corneal surface, many participants reported improvements in visual acuity following treatment. This outcome underscores the procedure’s potential as a viable option for people facing challenges in vision recovery due to ocular damage.
Evaluating the visual outcomes from the CALEC procedure has revealed promising results, leading to higher expectations for future applications of stem cell therapy in ophthalmology. By understanding the mechanism behind these improvements, researchers aim to refine the procedure further, enhancing its effectiveness and accessibility. The hope is to transform the landscape of vision recovery for individuals who have long struggled with impairments due to corneal injuries.
Future Directions for Corneal Treatments
As the field of corneal treatments evolves, a clear trajectory toward more personalized and effective strategies is emerging. With ongoing research into stem cell therapies, such as the CALEC procedure, the potential for creating tailored treatment plans based on individual patient needs is more promising than ever. This approach aims to address the complexities of corneal injuries while promoting healing in novel ways.
Future trials are expected to explore broader applications of the CALEC procedure, potentially making it a standard treatment option for various ocular conditions. By refining techniques and expanding research, the goal is to enable access to these innovative therapies for all patients, regardless of the severity of their corneal injuries. This proactive approach holds the promise of significantly improving visual health outcomes on a larger scale.
Conclusion: The Future of Stem Cell Innovations in Eye Care
The future of eye care is set to be revolutionized by stem cell innovations, primarily through therapies like CALEC that demonstrate clear success in treating corneal damage. As research evolves and demonstrates the impact of ocular stem cells, healthcare providers are moving closer to offering effective solutions for eye injuries that were once viewed as permanent.
Looking ahead, the ongoing commitment to advancing research and clinical trials will be crucial in bringing these groundbreaking treatments to a wider audience. By focusing on developing robust protocols and understanding patient needs, the medical community can ensure that stem cell therapies play a significant role in enhancing vision recovery and improving the overall quality of life for countless individuals.
Frequently Asked Questions
What is stem cell therapy for corneal injury treatment?
Stem cell therapy for corneal injury treatment involves harvesting limbal epithelial cells from a healthy eye, expanding them into a graft, and transplanting this graft into the damaged eye. This innovative approach, known as the CALEC procedure, has shown more than 90% effectiveness in restoring the corneal surface in clinical trials.
How does the CALEC procedure restore damaged corneas?
The CALEC procedure restores damaged corneas by taking stem cells from a healthy eye, cultivating them into a graft, and then transplanting that graft into a cornea damaged by injury or disease. This process helps regenerate the limbal epithelial cells that are crucial for maintaining a smooth corneal surface.
What role do ocular stem cells play in eye damage recovery?
Ocular stem cells, particularly limbal epithelial cells, are vital in eye damage recovery as they repair and regenerate the cornea. The CALEC procedure utilizes these stem cells to restore the cornea’s surface after injuries that lead to limbal stem cell deficiency.
Who can benefit from stem cell therapy in treating eye damage?
Individuals suffering from corneal injuries that deplete limbal epithelial cells, resulting in visual impairment and chronic pain, can benefit from stem cell therapy. Specifically, this therapy is suitable for patients with damage to one eye, allowing a biopsy to obtain healthy stem cells for treatment.
What are the success rates of the CALEC procedure in clinical trials?
Clinical trials of the CALEC procedure have demonstrated high success rates, with 50% of participants achieving complete corneal restoration at three months. This rate increased to 79% at 12 months and 77% at 18 months, evidencing the procedure’s efficacy in serious eye damage recovery.
Is the CALEC procedure available for patients right now?
Currently, the CALEC procedure is still experimental and not widely available, including at Mass Eye and Ear. Further studies and federal approval efforts are necessary before it becomes accessible to patients with corneal damage.
What are the main challenges associated with the CALEC procedure?
One significant challenge of the CALEC procedure is that it requires the patient to have only one healthy eye for obtaining limbal stem cells. There is ongoing research to develop an allogeneic process using donor stem cells to expand the treatment’s applicability.
Who led the clinical trial for the CALEC procedure?
The clinical trial for the CALEC procedure was led by Ula Jurkunas, an associate director of the Cornea Service at Mass Eye and Ear, alongside researchers from the National Eye Institute and collaborators from various hospitals.
What future research is planned for stem cell therapy in ocular treatments?
Future research on stem cell therapy for ocular treatments aims to include larger patient cohorts, longer follow-ups, and randomized controlled designs. These studies are crucial for seeking FDA approval and ensuring broader access to the treatment.
What should patients know about the safety of stem cell therapy for eye treatments?
Clinical trials of stem cell therapy, specifically the CALEC procedure, reported a high safety profile with no significant complications. While some minor adverse events occurred, they were quickly resolved, showcasing the therapy’s overall safety for eye damage recovery.
| Key Point | Details |
|---|---|
| Purpose of Study | To test the safety and effectiveness of stem cell therapy (CALEC) in restoring corneal surfaces in patients with cornea damage. |
| Methodology | Stem cells were harvested from a healthy eye and used to create a graft for transplantation to a damaged eye. |
| Results | The treatment achieved over 90% effectiveness in restoring corneal surfaces after 18 months. |
| Trial Participants | 14 patients participated, showing varying degrees of improvement in vision and cornea restoration. |
| Future Directions | Plans to develop an allogeneic manufacturing process to treat patients with damage to both eyes. |
| Safety | High safety profile with no major complications; one minor adverse event related to contact lens use. |
Summary
Stem Cell Therapy represents a groundbreaking approach to treating eye damage that was once deemed untreatable. This innovative treatment, particularly the cultivated autologous limbal epithelial cells (CALEC) method, has shown promising results, safely restoring corneal surfaces in a significant number of patients. The initial clinical trials led by Ula Jurkunas at Mass Eye and Ear exemplify the potential for this therapy to become a standard care practice for individuals suffering from severe corneal injuries. As research progresses, the goal is to refine these methods further, ensuring wider access to effective treatments that could alleviate visual impairments for thousands.

Plant-Based Oils: A Simple Swap to Boost Longevity
Plant-based oils are gaining recognition not only for their culinary versatility but also for their significant health benefits. Current research indicates that substituting butter with these oils can lead to a remarkable 17 percent reduction in the risk of premature death. This dietary swap has been linked to lower mortality rates from major health issues, including cancer and cardiovascular diseases. The findings from a comprehensive study conducted by renowned institutions emphasize how incorporating oils like soybean, canola, and olive into our diets can promote healthier living. By embracing plant-based oils, individuals can harness a simple yet effective strategy for enhancing their overall well-being and longevity.
Vegetable oils, often referred to as plant-derived fats, are becoming increasingly popular as individuals seek healthier dietary options. These oils serve as effective alternatives to traditional dairy fats, such as butter, allowing for significant dietary swaps that cater to health-conscious consumers. Emerging studies have highlighted the connection between regular consumption of these oils and lower mortality rates, particularly in relation to serious conditions like cancer. The advantage of these oils lies in their unsaturated fatty acid content, which is believed to contribute to their cancer prevention and heart health properties. As awareness grows around their myriad health benefits, plant-based oils are set to redefine how we approach our eating habits.
The Health Benefits of Plant-Based Oils
Incorporating plant-based oils into your daily diet can yield numerous health benefits, particularly in reducing the risk of chronic diseases. Studies indicate that consuming oils derived from sources such as soybeans, olives, and canola can significantly improve heart health due to their high levels of unsaturated fatty acids. Unlike butter, which is high in saturated fats that can raise bad cholesterol levels, plant-based oils contribute to better cardiovascular health, helping to lower the overall risk of heart disease.
Furthermore, these healthful oils are loaded with antioxidants and essential fatty acids that promote overall well-being. According to recent research, higher consumption of plant-based oils is also linked to lower mortality rates from various causes, including cancer. With their anti-inflammatory properties, these oils may play a role in preventing the development of certain cancers, reinforcing the idea that small dietary swaps can have a significant positive influence on health.
Substituting Butter for Plant-Based Oils
Substituting butter with plant-based oils is a straightforward dietary change that can have profound implications for long-term health. The recent study suggests that this simple swap can reduce premature death risk by 17 percent, making it a viable option for those looking to improve their nutrition. By replacing butter, which is rich in saturated fats, with plant-based oils such as olive or canola oil, individuals can significantly lower their intake of unhealthy fats while increasing beneficial nutrients that support heart health.
Additionally, as more people become aware of the health implications of their dietary choices, the importance of substituting butter becomes increasingly clear. In culinary practices, plant-based oils can be used for a variety of cooking methods including frying, sautéing, and baking. This not only helps in health-conscious meal preparation, but also enhances flavors and textures in foods, making it an appealing transition for those who enjoy cooking.
Understanding Dietary Swaps
Dietary swaps, such as replacing butter with plant-based oils, can be an effective strategy for improving health outcomes. By making these substitutions, individuals can enjoy foods they love while simultaneously reaping health benefits. The research highlights that these simple changes in dietary habits can lead to a longer, healthier life, especially given the alarming statistics surrounding chronic diseases linked to poor dietary choices.
Moreover, understanding how to implement these dietary swaps can empower individuals to make better food choices. For example, incorporating oils like olive oil in salads, or using canola oil for frying, are effective ways to enhance meals without compromising health. The convenience of finding plant-based oils in supermarkets makes it easier for anyone to adopt these beneficial changes.
The Link Between Diet and Lower Mortality Rates
The relationship between diet and longevity is increasingly recognized in the scientific community. By analyzing extensive data from health studies, researchers have found that individuals who adhere to a diet rich in plant-based oils tend to experience lower mortality rates. This correlation underscores the significant impact dietary patterns can have not just on individual health, but also on public health at large, demonstrating that choosing healthier fats can contribute to longer lives.
Additionally, establishing a direct connection between dietary fats and overall mortality provides a compelling reason for dietary change. For instance, the reduction of butter intake in favor of plant-based oils is not just a personal choice; it is a public health message that can potentially save lives. As people become more conscientious about the dietary fats they consume, it could lead to a collective improvement in health outcomes across communities.
Cancer Prevention Through Dietary Changes
Cancer prevention is a crucial aspect of health, and recent studies have highlighted the role of dietary fats in this domain. Research suggests that substituting butter with plant-based oils can be part of a proactive strategy to lower cancer risk. The unsaturated fatty acids found in these oils can help mitigate inflammation and oxidative stress, both of which are linked to cancer development.
Incorporating more plant-based oils into one’s diet may not only reduce cancer risks but also support overall health in multiple ways. By making intentional dietary swaps, individuals can create a more healthful diet that aims to prevent cancer while also enhancing longevity and quality of life. As evidence mounts, it becomes increasingly clear that dietary choices play a pivotal role in cancer prevention and overall wellness.
Long-Term Health Benefits of Plant-Based Eating
Adopting a plant-based eating pattern that includes a wide variety of oils can offer extensive long-term health benefits. Research findings indicate that higher consumption of plant oils is associated with decreased risks of chronic diseases, including heart disease and certain cancers. Over time, these dietary choices can result in better health outcomes, enhancing both quality and longevity of life.
Moreover, a plant-based diet that emphasizes natural foods like fruits, vegetables, legumes, and oils not only supports physical health but can also have positive effects on mental well-being. The nutrients found in these foods—along with the healthy fats from plant-based oils—contribute to improved brain function and emotional resilience, further illustrating the profound impact of diet on holistically maintaining health.
The Importance of Healthy Fats in Your Diet
Healthy fats play an essential role in a well-rounded diet, and incorporating plant-based oils is a fantastic way to prioritize these nutrients. Unlike saturated fats found in butter and other animal products, healthy fats such as those derived from nuts, seeds, and oils can provide vital energy and support bodily functions. They also offer essential fatty acids that are crucial for brain health and hormone production.
As awareness grows regarding the benefits of healthy fats, replacing saturated fats with sources of unsaturated fats—from plant-based oils—should become a standard in dietary practices. By understanding and choosing healthier fat options, individuals can make significant strides toward enhancing their health and reducing disease risk.
Public Health Implications of Dietary Changes
The findings of recent studies on substituting butter for plant-based oils extend beyond individual health; they also have significant public health implications. If more people adopted these simple dietary changes, it could lead to dramatic reductions in chronic disease rates across populations. Such changes could alleviate the burden on healthcare systems dealing with the fallout from poor dietary practices, making it crucial for public health campaigns to promote these findings.
Incorporating educational programs that highlight the benefits of substituting unhealthy fats with healthier options can empower communities to make informed decisions about their diets. As public awareness increases, the potential for improving health outcomes through dietary education offers an optimistic view for the future health of populations.
Strategies for Incorporating Plant-Based Oils into Your Diet
Incorporating plant-based oils into your daily routine doesn’t have to be complicated. Simple strategies, such as replacing butter in recipes with oils like olive or avocado oil, can make a big difference. Whether used in salad dressings, sautés, or as a bread dip, these oils can enhance flavors while contributing to better health outcomes.
Moreover, learning how to use plant-based oils effectively in meal preparation allows for versatility in cooking. For example, using canola oil for frying or baking can provide a healthier alternative without compromising taste. By getting creative with the use of plant oils, individuals can enjoy delicious meals while making positive changes towards a healthier lifestyle.
Frequently Asked Questions
What are the health benefits of substituting butter with plant-based oils?
Substituting butter with plant-based oils like olive, soybean, and canola can offer significant health benefits, including a 17% reduction in premature death risk. This dietary swap lowers mortality rates associated with cancer and cardiovascular diseases, making plant-based oils a healthier alternative to butter.
How does incorporating plant-based oils contribute to cancer prevention?
Incorporating plant-based oils into your diet can contribute to cancer prevention by replacing saturated fats found in butter with healthier unsaturated fats. Studies suggest that higher consumption of plant-based oils is linked to lower cancer mortality rates, emphasizing the protective role these oils may play against various cancers.
What dietary swaps can enhance longevity and lower mortality rates?
A key dietary swap for enhancing longevity is replacing butter with plant-based oils. Research indicates that making this simple change can lead to a 17% lower risk of premature death, highlighting the importance of dietary choices in promoting long-term health and reducing mortality.
Which plant-based oils are most effective in reducing health risks?
Plant-based oils such as olive oil, canola oil, and soybean oil have been found particularly effective in reducing health risks. Regular consumption of these oils, as a substitute for butter, can lower mortality rates and promote better cardiovascular health.
Can small reductions in butter intake lead to significant health improvements?
Yes, even small reductions in butter intake, combined with a greater incorporation of plant-based oils, can lead to significant health improvements. Studies suggest that slight dietary changes can yield considerable long-term benefits, helping to reduce risks associated with chronic diseases.
How should individuals start transitioning from butter to plant-based oils?
Individuals can begin transitioning from butter to plant-based oils by gradually substituting oils like olive or canola for butter in cooking, baking, and dressings. They can start with using oils in salad dressings or for sautéing to ease into this healthier dietary choice.
| Key Points |
|---|
| A study found that replacing butter with plant-based oils can lower the risk of premature death by 17%. |
| Key oils studied include soybean, canola, and olive oil. |
| Higher plant-based oil consumption is linked to lower mortality rates from various causes, including cancer and cardiovascular disease. |
| Butter is high in saturated fats, while plant-based oils are richer in unsaturated fats, which are generally healthier. |
| The study analyzed data from 221,054 participants over more than 30 years, tracking diet and health outcomes. |
| Even modest reductions in butter intake can yield significant health benefits. |
| The findings indicate that dietary changes can prevent deaths from chronic diseases. |
Summary
Plant-based oils are a healthier alternative to butter; studies show that making this simple switch can significantly lower the risk of premature death. By substituting butter with oils like soybean, canola, and olive, individuals can enhance their overall health and reduce mortality rates associated with chronic diseases. Embracing plant-based oils not only benefits personal health but could also serve as a preventive measure against severe health conditions in the population.

Medical Gaslighting: Understanding Its Impact on Patients
Medical gaslighting is an increasingly recognized issue in healthcare, where patients often find themselves dismissed or invalidated by their providers. This phenomenon can leave individuals feeling frustrated and unheard, particularly those battling chronic conditions with unclear diagnoses, such as long COVID or irritable bowel syndrome. The doctor-patient relationship is paramount, yet pressures on doctors can lead to misunderstandings, contributing to feelings of medical invalidation. With the rising prevalence of gaslighting in healthcare discussions on social media, it’s crucial to explore its implications for patient experience and outcomes. Understanding these dynamics can foster better communication and compassion within the healthcare system, addressing the burnout in physicians that often exacerbates the issue.
In the realm of healthcare, the phenomenon often termed as medical gaslighting encompasses various experiences where patients feel their concerns are unjustly minimized or overlooked by medical professionals. This form of medical invalidation can feel particularly acute in a landscape where conditions lack tangible proof, leading to a breakdown in the essential doctor-patient bond. The dialogue surrounding doctor-patient dynamics must evolve to include terms like emotional displacement and communicative dissonance, which highlight how systemic pressures on physicians can compromise patient trust and care. Such discussions acknowledge the human aspects of medicine, allowing for greater empathy and understanding of the pressures faced by providers that might inadvertently impact their interactions. By redefining these terms and embracing a compassionate approach, we can create a more supportive environment for both patients and healthcare providers.
Understanding Medical Gaslighting
Medical gaslighting refers to the phenomenon where healthcare providers dismiss or downplay the experiences of their patients, often making them feel as though their symptoms are not valid. This aptly named term has gained significant traction in contemporary healthcare discussions due to the rising instances where patients feel their concerns are inadequately addressed. far too often, patients are left navigating their ailments alone, struggling against the tide of disbelief that can arise from a doctor’s inability to pinpoint a diagnosis based solely on medical testing.
In many cases, especially in conditions like long COVID or irritable bowel syndrome, patients report feeling unheard or invalidated. The emotional impact of such dismissals can be profound, reinforcing feelings of isolation and confusion. As the discussion on medical gaslighting evolves, it sheds light on a critical need for healthcare providers to foster a more empathetic approach to patient interactions.
The Consequences of Medical Invalidation
Medical invalidation occurs when a healthcare provider fails to acknowledge or understand a patient’s experiences, leading to feelings of rejection or doubt in the patient’s mind about their conditions. This form of dismissal can significantly damage the doctor-patient relationship, as trust is essential for effective care. Patients who feel invalidated may avoid seeking further medical help, fearing that their concerns will be treated with the same lack of seriousness as before.
Furthermore, the consequences of medical invalidation extend beyond individual patients. When large numbers of patients face this issue within a healthcare system, it can lead to widespread disillusionment with medical professionals. Patient experiences become marred by trauma, and the ripple effect can influence public perception of healthcare, ultimately impacting the overall quality of care.
The Role of the Doctor-Patient Relationship
A strong doctor-patient relationship is foundational for effective healthcare delivery. When patients feel heard and validated, they engage more actively in their care processes and are more likely to adhere to treatment plans. However, high-pressure environments can compromise this dynamic, leading providers to inadvertently rush through consultations, thus failing to connect with their patients. This lack of personal connection can cause further feelings of isolation in patients.
To cultivate a trusting doctor-patient relationship, healthcare providers must prioritize empathetic communication. Allowing time for patients to share their stories and concerns not only fosters trust but also enhances the efficacy of the diagnosis and treatment. Trust is built when patients feel that their experiences are valued, which could prevent situations of medical invalidation and the psychological toll that accompanies it.
Addressing Gaslighting in Healthcare
Addressing gaslighting in healthcare requires both awareness and action from medical professionals. While the term ‘gaslighting’ can carry heavy implications, it is essential to differentiate between intentional deception and the systemic issues that lead to medical invalidation. By establishing a culture of compassion and understanding, healthcare providers can mitigate the risk of patients feeling neglected or dismissed.
Training programs that focus on communication skills, empathy, and patient-centered care can help reduce instances of gaslighting. When healthcare systems place an emphasis on understanding patient experiences as integral to care, both patient satisfaction and health outcomes improve.
Recognizing Burnout Among Physicians
Physician burnout is an increasingly recognized issue that can have significant implications for patient care. When healthcare providers experience high levels of stress and emotional exhaustion, their capacity to engage empathetically with patients diminishes. Burnout can lead to a defensive posture where physicians may unintentionally invalidate their patients’ experiences due to overwhelming workload pressures.
Addressing physician burnout requires systemic changes in healthcare management, including reducing documentation loads and increasing support staff. By alleviating some of the structural pressures on physicians, healthcare systems can improve the overall patient experience as well as the mental well-being of their providers.
Creating a Compassionate Healthcare Environment
A compassionate healthcare environment is crucial for preventing medical gaslighting and invalidation. This starts with fostering a culture in which healthcare professionals are encouraged to view patients as partners in their care. For patients, being part of the healthcare conversation can facilitate a cooperative approach to diagnosis and treatment that can enhance satisfaction and outcomes.
Moreover, systems that prioritize compassion in care can also reduce the stressors contributing to physician burnout. Ensuring that healthcare providers have manageable workloads, proper mental health resources, and supportive policies can create an environment in which both patients and physicians thrive. In turn, this can lead to more open communication, reducing the likelihood of misunderstandings that contribute to gaslighting incidents.
Improving Patient Experiences through Active Listening
One of the most effective ways to combat medical gaslighting is through the practice of active listening on the part of healthcare providers. By truly hearing what patients have to say, physicians can validate their experiences and foster a more inclusive environment. Active listening involves not only hearing the words but also acknowledging emotions and experiences, which can provide a sense of validation for the patient.
By implementing strategies for active listening, healthcare professionals can demonstrate their commitment to understanding diverse patient needs. This can help to bridge the gap that often exists in the doctor-patient relationship and significantly improve overall patient experience. Ultimately, making space for the patient’s voice transforms medical interactions from mere clinical assessments into meaningful conversations.
Impact of Technology on Healthcare Communication
In the digital age, technology has both exacerbated and alleviated issues surrounding medical gaslighting. While telemedicine provides convenient access to care, it can also lead to more impersonal interactions if not managed correctly. Patients may feel less connected to their providers when communicating through screens, furthering misunderstandings and feelings of invalidation.
To mitigate the risks associated with technology in healthcare, it’s essential for providers to employ tools that enhance communication. Investing in user-friendly platforms that encourage virtual face-to-face interactions can help maintain the personal connection so vital in the healthcare process, ensuring that patients feel heard and validated even at a distance.
Transforming Healthcare Systems for Better Outcomes
Transforming healthcare systems to prioritize patient experience can have profound effects on reducing medical gaslighting. When healthcare institutions focus on holistic approaches that encompass both patient care and provider support, they can cultivate environments that nurture both parties. Systemic changes that facilitate better doctor-patient communication can also enhance overall trust and satisfaction.
Such transformations require collaboration among healthcare leaders, policy makers, and professionals to implement changes that address the root causes of medical invalidation. With the right strategies in place, healthcare systems can significantly improve physician engagement and patient outcomes, ultimately leading to a more effective and compassionate healthcare experience.
Frequently Asked Questions
What is medical gaslighting and how does it impact the patient experience?
Medical gaslighting refers to the phenomenon where patients feel their concerns, experiences, or symptoms are dismissed or invalidated by healthcare providers. This often results in patients questioning their own reality and leads to feelings of frustration, despair, and decreased trust in the healthcare system. It is crucial to address this issue to improve the patient experience and foster a better doctor-patient relationship.
How can medical invalidation occur in doctor-patient relationships?
Medical invalidation can occur when a doctor dismisses a patient’s reported symptoms as being imaginary or all in their head, especially in cases of hard-to-diagnose conditions. This behavior undermines the patient’s lived experience and can severely harm the doctor-patient relationship, leading to mistrust and inadequate patient care.
What are the signs of gaslighting in healthcare settings?
Signs of gaslighting in healthcare include a doctor questioning the validity of a patient’s symptoms, suggesting that the issue is psychological without investigating further, or failing to listen actively to the patient’s concerns. Recognizing these signs is critical for patients to advocate for their own health and seek validation in their experiences.
How does burnout in physicians contribute to medical gaslighting?
Burnout in physicians, often due to high caseloads and overwhelming documentation demands, can result in hurried patient interactions. This pressure may lead to medical gaslighting, as physicians may not have the time to fully engage with patients, leading to unintentional dismissals of important health concerns.
What are effective strategies to prevent medical gaslighting in healthcare?
To prevent medical gaslighting, healthcare systems should prioritize effective communication training for physicians, allow ample time for patient consultations, and promote a culture of empathy. Encouraging patients to share their experiences thoroughly and validating their concerns can help rebuild trust and improve the overall healthcare environment.
Why is compassionate care important in the context of medical gaslighting?
Compassionate care is crucial in preventing medical gaslighting as it fosters a supportive doctor-patient relationship. When physicians express understanding and validate patient experiences, it combats feelings of invalidation and helps ensure that patients feel heard, respected, and properly cared for.
How can patients advocate for themselves against medical gaslighting?
Patients can advocate for themselves by clearly communicating their symptoms, asking questions about any dismissive remarks, and seeking second opinions when they feel invalidated. Keeping detailed records of their symptoms and experiences can also empower them in conversations with healthcare providers.
What is the difference between medical gaslighting and medical invalidation?
Medical gaslighting typically implies intent to deceive, where a provider consciously undermines a patient’s experience. In contrast, medical invalidation may occur without malicious intent, as providers may simply lack the time or resources to adequately validate a patient’s concerns, which still leads to negative impacts on patient care.
| Key Points |
|---|
| Medical gaslighting refers to patients feeling dismissed by healthcare providers, especially when hard-to-detect conditions like long COVID or irritable bowel syndrome are involved. |
| The term ‘gaslighting’ might not be appropriate as it implies intent to deceive, which is often absent in medical settings. |
| Medical invalidation is a more suitable term that reflects the behavior of providers who may unintentionally dismiss patient experiences due to workload pressures. |
| Healthcare professionals face significant pressure to diagnose correctly and manage high patient loads, contributing to interactions where patient concerns are not adequately addressed. |
| Improving healthcare systems and reducing pressures on doctors may help to prevent incidents of medical invalidation. |
Summary
Medical gaslighting is an ongoing issue in the healthcare field, where patients, particularly those with vague or hard-to-diagnose conditions, feel their concerns are dismissed by providers. This phenomenon is exacerbated by systemic pressures within the medical environment, which can lead to hurried consultations and inadequate patient-provider communication. Recognizing the nuances of medical gaslighting, particularly distinguishing it from unintentional medical invalidation, is crucial in fostering compassionate healthcare practices that prioritize patient understanding and support.
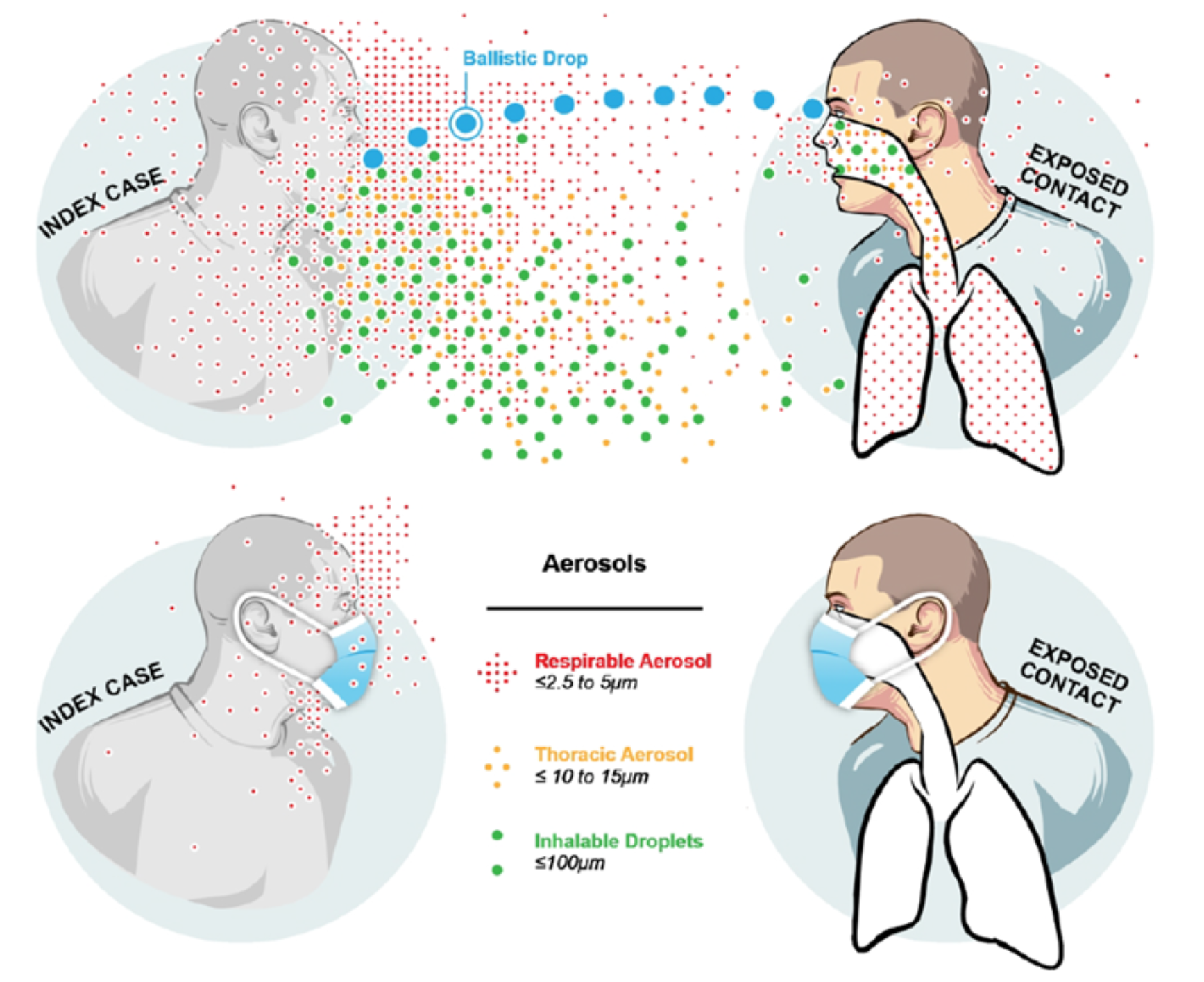
Airborne Disease Control: The Impact of Social Dynamics
Airborne disease control is a critical field of public health aimed at preventing the spread of illnesses that can easily transmit through the air. As highlighted by renowned science communicator Carl Zimmer, understanding how airborne diseases operate has evolved dramatically from ancient theories of “bad air” to concrete scientific findings. William Firth Wells played a pivotal role in this journey by demonstrating that pathogens could be carried by human exhalations, thereby emphasizing the crucial need for effective airborne disease control measures. Innovations such as UV light treatment have been suggested to neutralize these airborne pathogens, underscoring the intersection of technology and public health strategy. With ongoing challenges in managing airborne diseases, the insights from pioneers like Wells remain relevant and essential for future advancements in disease prevention.
Controlling diseases transmitted through the air, often referred to as airborne infection management, encompasses strategies designed to mitigate the spread of pathogens contained in respiratory droplets. Carl Zimmer’s exploration of this topic sheds light on historical figures such as William Firth Wells, whose groundbreaking work revealed the significance of air quality in public health. By employing methods to trap and analyze the air around us, scientists have gradually shifted our understanding from abstract concepts to actionable insights. The role of ultraviolet light in eradicating these potentially harmful pathogens demonstrates the integration of innovative solutions into disease prevention. As we navigate the complexities of airborne illnesses, the continued study and application of these strategies are vital to safeguarding public health.
The Role of Personality in Scientific Progress
Scientific advancements often hinge on the personalities of the researchers behind them. In the case of airborne disease control, Carl Zimmer argues that the social skills of William Firth Wells may have played a pivotal role in the acceptance—or lack thereof—of his groundbreaking findings. Despite his significant contributions, including the demonstration that pathogens can be transmitted through the air, Wells struggled to communicate his ideas effectively due to a perceived inability to connect with his audience. This disconnect may have led to skepticism within the scientific community, ultimately slowing the progress necessary for widespread adoption of airborne disease prevention measures.
This phenomenon is not unique to Wells; many innovative scientists face similar challenges. The reluctance of the public and fellow researchers to embrace controversial ideas, such as those formulated by Wells on airborne infections, emphasizes the importance of effective communication in science. Good interpersonal skills can often help researchers gain credibility and garner support for their work. The case of Wells illustrates the concept that sometimes, the discovery of a revolutionary idea is not enough; how that idea is presented to the world can make all the difference.
Unveiling the Science of Airborne Diseases
The understanding of airborne diseases has evolved significantly over the centuries, moving from ancient concepts of miasmas to the acknowledgment of microorganisms as the true culprits. Carl Zimmer highlights this shift in perception, attributing substantial credit to researchers like William Firth Wells, who demonstrated that pathogens can indeed linger in the air. By the early 20th century, the scientific community began to recognize the reality of airborne infection, fueled by experiments that showcased how diseases such as tuberculosis spread through the air we breathe.
Wells’ pioneering experiments in cultivating airborne pathogens signified a turning point in public health. His research on the efficacy of ultraviolet (UV) light in eliminating these pathogens opened new avenues for airborne disease control. As disease outbreaks began to plague populations, especially during WWII, the need for effective control measures became increasingly urgent. Wells’ infection chambers exemplified innovative approaches to managing airborne risks, laying the groundwork for future public health strategies that emphasize the significance of indoor air quality and pathogen transmission.
The quest to understand how pathogens travel and contaminate public spaces continues to inform contemporary approaches to disease prevention. The implications of Wells’ work are evident today, especially in light of recent global health crises that underscore the necessity of addressing airborne transmission. Current technologies aim to minimize exposure to airborne pathogens in various environments, demonstrating how Wells’ foundational research remains crucial in contemporary public health advancements.
UV Light: A Tool for Airborne Disease Control
The discovery of UV light’s ability to neutralize airborne pathogens was a significant milestone in the field of public health. Wells’ innovative use of UV light as a disinfection tool showcased how preventative measures could be applied in settings prone to airborne diseases. This technique became invaluable during outbreaks, offering a practical solution to minimize the risk of infection in heavily populated areas, such as schools and hospitals. The synergy between Wells’ theories and the practical applications of UV technology represents a critical advancement in the fight against airborne diseases.
Today, the integration of UV light systems in ventilation and air filtration systems serves to underscore the continuing relevance of Wells’ research. Modern iterations of Wells’ infection chambers have evolved into sophisticated devices designed to purify air and eradicate harmful microorganisms, effectively mitigating the spread of illnesses such as influenza and COVID-19. The ongoing implementation of air purification technologies in public spaces exemplifies the intersection of scientific discovery and technological advancement that defines modern public health practice, highlighting the vital role played by early researchers like Wells.
Historical Context of Airborne Disease Understanding
The historical perspectives on airborne disease transmission reflect a gradual evolution from ancient beliefs to modern scientific understanding. Carl Zimmer discusses how early ideas such as Hippocrates’ miasma theory laid the groundwork for questions about how diseases spread. For centuries, the notion that air could harbor harmful microorganisms was overlooked, leading to widespread misunderstandings that impeded public health responses during outbreaks, such as cholera in the 1830s.
The journey towards recognizing airborne transmission was slow, with pivotal contributions from figures like William Firth Wells shaping modern consciousness around this issue. By rejecting outdated beliefs and embracing empirical evidence, scientists started to unveil the complex interactions between pathogens and the air we breathe. Zimmer’s account allows us to appreciate the monumental shifts that have taken place, ultimately culminating in an acknowledgment of the airborne spread of diseases as a legitimate threat that requires comprehensive control methods.
Implications for Modern Public Health Policies
Understanding airborne diseases and their transmission is critical for informing effective public health policies. In light of historical lessons learned, contemporary strategies now emphasize the need for proactive approaches in disease prevention and control, particularly in response to respiratory pathogens. With experts like Wells paving the way, health officials advocate for improved ventilation standards in buildings, the use of air purification technologies, and public awareness campaigns aimed at educating citizens about the importance of airborne disease management.
The COVID-19 pandemic serves as a stark reminder of how easily airborne pathogens can spread, highlighting the necessity of adapting public health policies to urgent realities. Insights drawn from Wells’ research reveal a pressing need to factor airborne transmission into policy discussions, shaping response mechanisms to protect populations. As we continue navigating evolving disease landscapes, the lessons learned from historical figures in the field underscore the importance of vigilance and adaptability in public health frameworks.
Scientific Collaboration: Bridging Gaps in Research
Carl Zimmer’s commentary on the challenges faced by William Firth Wells in communicating his findings also touches on the broader theme of collaboration within the scientific community. The progression of research on airborne diseases showcases the need for multidisciplinary approaches, combining insights from microbiology, public health, and engineering. Scientific collaboration often enhances the potential for innovation, yielding comprehensive solutions, especially in the complex realm of infectious disease control.
By fostering stronger communication and teamwork among researchers, the scientific community can build on Wells’ legacy, addressing the gaps that historically limited progress in understanding airborne pathogens. Collaboration facilitates the exchange of ideas, encourages diverse perspectives, and ultimately leads to scientifically sound interventions that safeguard public health. As the landscapes of infectious diseases continue to evolve, reinforcing collaborative networks will be vital in harnessing the full potential of scientific inquiry.
The Future of Airborne Disease Research
Looking ahead, the field of airborne disease research holds immense promise, particularly as technological advancements foster new methodologies in virus detection and air purification. The history of contributions from insightful researchers like Wells serves as a foundation on which modern scientists can build their investigations. The increased focus on airborne pathogens since the onset of the COVID-19 pandemic indicates a potential renaissance in studies related to ventilation, air quality, and their direct links to health outcomes.
Future prospects include integrating new technologies such as artificial intelligence and advanced modeling techniques to predict how airborne diseases spread and can be controlled in various environments. This comprehensive approach not only honors the legacy of foundational research but will also equip modern public health systems with the necessary tools to respond effectively to emerging health threats.
Public Awareness and Education on Airborne Diseases
As the body of research around airborne diseases continues to expand, public awareness and education become increasingly vital. Understanding the modes of transmission—including the role of airborne pathogens in illnesses—can empower communities to take proactive measures in disease prevention. Initiatives that promote awareness of how airborne diseases spread can contribute to more informed public behaviors and foster a culture of health responsibility.
Educational campaigns that highlight the significance of Wells’ findings and promote practices such as proper ventilation and air quality monitoring will play an essential role in shaping future public health responses. The more individuals understand the importance of air safety and the risks associated with airborne pathogens, the better prepared they will be to protect themselves and others from infection.
The Intersection of Science and Society
The relationship between scientific inquiry and societal acceptance often plays a crucial role in the trajectory of public health measures. Drawing from the experiences of William Firth Wells as discussed by Carl Zimmer, the importance of contextualizing scientific findings within the broader societal framework cannot be overstated. When scientists successfully convey their discoveries to the public, such as the risks posed by airborne diseases, the resulting knowledge can drive effective health policies and individual behaviors.
However, when researchers like Wells encounter barriers to communication, such as social awkwardness or unpopular personalities, their contributions may be overshadowed, hindering societal understanding. This intersection of science and society demands an ongoing commitment to improving communication strategies in public health messaging. Ensuring that scientific advancements reach diverse audiences is essential in fostering public trust and engagement, ultimately leading to a healthier society.
Frequently Asked Questions
What are airborne diseases and how do they relate to public health?
Airborne diseases are illnesses caused by pathogens that spread through the air, primarily via respiratory droplets or aerosols. Understanding airborne disease control is crucial for public health as it helps prevent outbreaks and protects community health through effective infection prevention strategies.
How did William Firth Wells contribute to airborne disease control?
William Firth Wells made significant contributions to airborne disease control by pioneering research that demonstrated how pathogens could be transmitted through the air. His innovative experiments using a centrifuge and his theory that ultraviolet light could eliminate airborne pathogens were foundational in establishing the importance of air quality in controlling infections.
What role does UV light play in controlling airborne diseases?
UV light has been shown to effectively disinfect air by killing airborne pathogens, making it a valuable tool in airborne disease control. Research by scientists like William Firth Wells highlighted the potential of UV light in sanitizing environments, thereby reducing the risk of airborne transmission of infectious diseases.
How does the history of researching airborne diseases affect current public health policies?
The history of researching airborne diseases, particularly the struggles faced by early scientists like Wells, informs current public health policies by emphasizing the importance of recognizing airborne transmission. This historical context supports ongoing advocacy for enhanced air quality measures, better ventilation systems, and the implementation of infection control protocols.
What challenges have historians noted about the acceptance of airborne disease theories?
Historians, including Carl Zimmer, have noted that the acceptance of airborne disease theories often faced challenges due to societal biases, personalities of key researchers like William Firth Wells, and prevailing misconceptions about disease transmission. These challenges illustrate the need for clear communication and education about airborne disease control.
Why is research on airborne disease control still relevant today?
Research on airborne disease control remains highly relevant due to the persistence of infectious diseases and emerging pathogens that can spread through the air. Understanding past challenges and advancements, such as those made by Wells, informs modern strategies to mitigate risks in various environments, including healthcare and public spaces.
| Key Points |
|---|
| Carl Zimmer’s talk explores the impact of personality on airborne disease control research. |
| William Firth Wells, a key figure in airborne disease research, faced challenges due to his personality. |
| Despite significant contributions, Wells’ work was often disregarded due to poor communication skills. |
| Airborne pathogens were historically underestimated in disease transmission. |
| Zimmer highlights the historical shift in understanding disease transmission, linking it to personal dynamics. |
Summary
Airborne disease control has often been affected by the personalities of researchers involved. As described by Carl Zimmer, William Firth Wells’ groundbreaking work on airborne pathogens suffered due to his social awkwardness and communication difficulties. This illustrates the critical role that both scientific discovery and personal dynamics play in the acceptance and application of airborne disease research. Understanding these challenges is vital for advancing airborne disease control and ensuring effective public health measures.
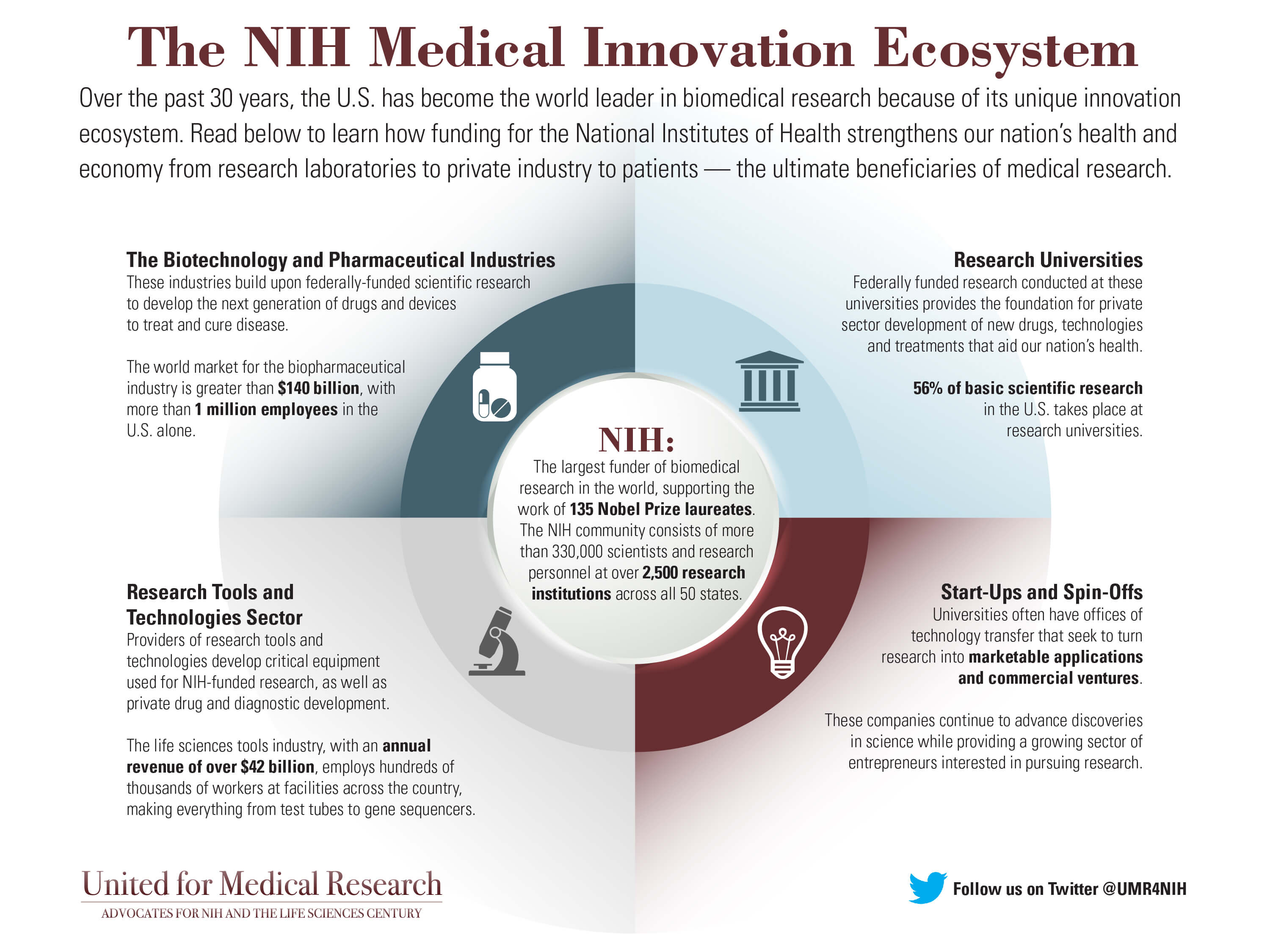
U.S. Health Innovation Ecosystem: A Historical Overview
The U.S. health innovation ecosystem stands as a global benchmark, showcasing the successful collaboration between public and private sectors in advancing biomedical research and technology. This dynamic landscape emerged significantly during World War II, with pivotal government-supported initiatives like the mass production of penicillin, which revolutionized medical treatment and set the stage for subsequent healthcare breakthroughs. Insights gained from federal funding for biomedical research have fueled innovative partnerships, leading to discoveries that benefit both military and civilian populations. The historical context highlights how the foundations laid during wartime efforts continue to drive contemporary advancements in medicine through strategic public-private partnerships. As we navigate the complexities of modern healthcare, understanding this intricate ecosystem is essential to promoting sustainable innovation and ensuring continued progress in the field.
The landscape of U.S. healthcare innovation embodies a rich tapestry of ideas and collaborations that have shaped modern biomedicine. Often referred to as the biomedical ecosystem, this intricate web consists of partnerships between educational institutions, government agencies, and private enterprises, each playing a crucial role in fostering scientific discovery. Since the 1940s, federal investment in research has harmoniously blended with entrepreneurial spirit, enabling remarkable technological advancements that have transformed patient care. This synergy not only reflects the storied history of American biomedical research but also highlights a broader paradigm where strategic alliances cultivate a flourishing environment for innovative medical solutions. By embracing a legacy rooted in public investment and cooperative research, the U.S. continues to lead the way in health innovation.
The Origins of the U.S. Health Innovation Ecosystem
The U.S. health innovation ecosystem is built on a rich history that dates back to World War II, when the urgent demands of wartime propelled significant advancements in biomedical science. Initially, the federal government recognized the necessity of harnessing civilian scientists to pioneer technological breakthroughs. This collaboration between government and academia catalyzed a shift towards a more structured research environment, laying the foundation for modern biomedical innovation. Today, this ecosystem stands as a global leader in scientific advancement, owing much to its historical roots.
The pivotal time of World War II illustrated the critical need for effective medical treatments, particularly as infectious diseases posed serious risks to military personnel. The establishment of entities like the Office of Scientific Research and Development (OSRD) enabled a coordinated effort to channel resources and expertise into developing life-saving solutions. This set the stage for the future growth of the National Institutes of Health (NIH) and other research institutions that form the backbone of the U.S. health innovation system today.
Frequently Asked Questions
What is the role of public-private partnerships in the U.S. health innovation ecosystem?
Public-private partnerships have been a cornerstone of the U.S. health innovation ecosystem, facilitating collaboration between government entities, academic institutions, and private industry. This collaborative dynamic has enabled significant advancements in biomedical innovation, ensuring that research initiatives are well-funded and effectively translated into practical medical solutions.
How has federal funding impacted the U.S. health innovation ecosystem?
Federal funding has been instrumental in shaping the U.S. health innovation ecosystem, particularly in biomedical research. It provides essential financial resources that support academic institutions and industry collaborations, facilitating the discovery of new treatments and technologies essential for public health.
What was the significance of USDA penicillin production during World War II for the U.S. health innovation ecosystem?
The USDA’s mass production of penicillin during World War II marked a pivotal moment in the U.S. health innovation ecosystem. It demonstrated the effectiveness of federal support for biomedical innovation, resulting in the rapid development and distribution of antibiotics that saved countless lives and laid the groundwork for modern pharmaceuticals.
What is the historical context of biomedical innovation in the U.S.?
The history of biomedical innovation in the U.S. traces back to World War II, when urgent health needs prompted government-university partnerships that significantly advanced medical research. This collaboration set the stage for the modern U.S. health innovation ecosystem, characterized by robust funding, research advancements, and effective public-private partnerships.
How did World War II influence the development of the U.S. health innovation ecosystem?
World War II catalyzed the development of the U.S. health innovation ecosystem by highlighting the need for rapid biomedical advancements. Initiatives such as the Office of Scientific Research and Development established collaborative frameworks between the government and research institutions, leading to notable innovations like penicillin and a lasting legacy in biomedical research.
What are the challenges currently facing the U.S. health innovation ecosystem?
Currently, the U.S. health innovation ecosystem faces challenges including proposed cuts to federal funding for biomedical research, which could threaten public-private partnerships that drive innovation. These challenges underscore the importance of sustaining investments in health research to maintain the efficacy and growth of this vital ecosystem.
Why is the U.S. health innovation ecosystem considered a global benchmark?
The U.S. health innovation ecosystem is regarded as a global benchmark due to its successful integration of federal funding, academic research, and private industry. This model has inspired similar systems worldwide, showcasing its effectiveness in generating groundbreaking biomedical innovations and responding to complex health challenges.
| Key Points | Details |
|---|---|
| Historical Origin | The U.S. health innovation ecosystem began during World War II with government-supported research initiatives. |
| Public-Private Partnership | This partnership fostered collaboration between the federal government, academic institutions, and private industries, leading to significant advancements in biomedicine. |
| Impact of WWII | The war highlighted the urgent need for innovations in health technologies, spurring the development of critical medical advancements like penicillin. |
| Role of the NIH | The National Institutes of Health played a crucial role in funding and developing research institutions post-war. |
| Challenges and Funding | Federal funding has come under scrutiny, with potential cuts threatening the ongoing success of the health innovation ecosystem. |
| Legacy and Future | The foundational efforts during the war led to a global benchmark for biomedicine, which must be preserved to sustain further innovation. |
Summary
The U.S. health innovation ecosystem stands as a global exemplar, having evolved from critical wartime collaborations into a cornerstone of modern medical advancements. The partnership between federal institutions, academia, and private industry has fostered significant breakthroughs in biomedicine, particularly evident during World War II with the mass production of penicillin. However, current challenges regarding federal funding highlight the need for ongoing support to maintain this successful model. Preserving the synergies developed over decades is essential for future health innovations and maintaining the progressive momentum of the U.S. health innovation ecosystem.
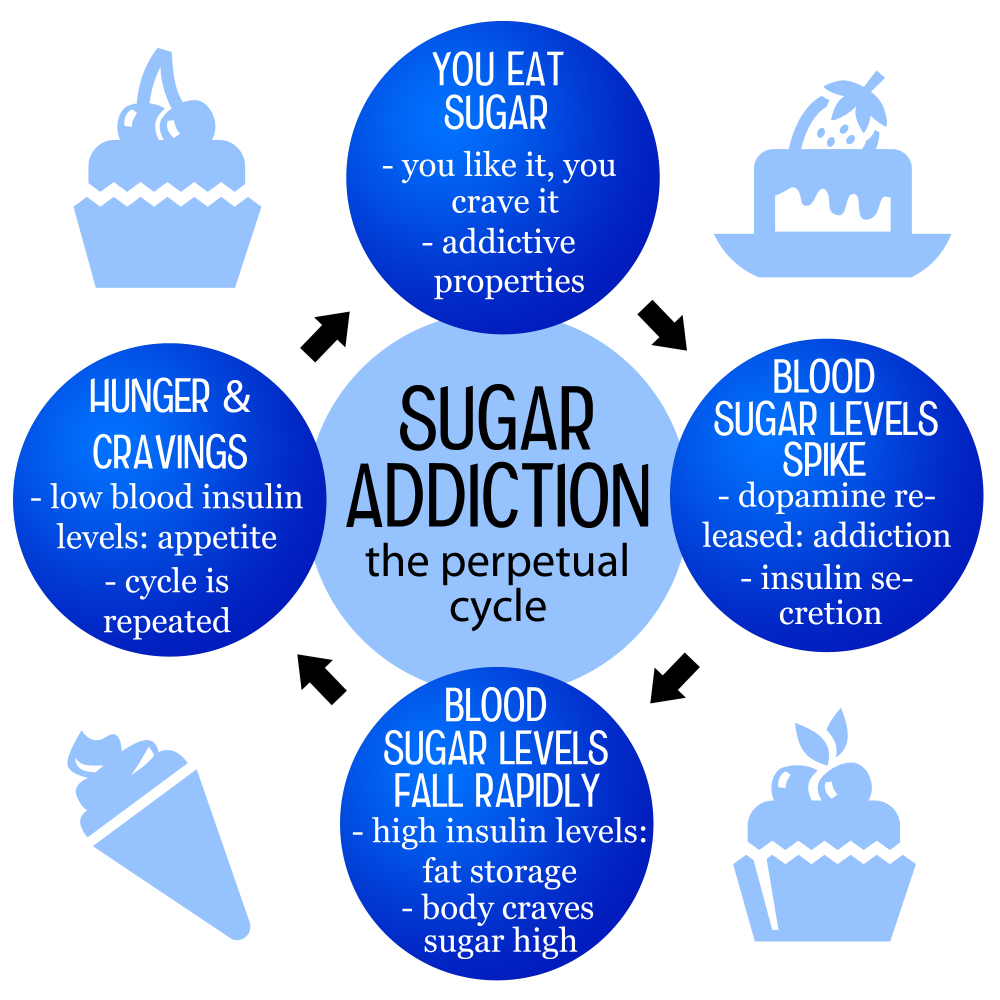
Is Sugar Addictive? Understanding the Cravings and Effects
Is sugar addictive? This question has sparked significant debate among nutrition researchers and health professionals alike. While substances like alcohol and nicotine fall squarely within the realm of addiction, sugar elicits strong cravings and compulsive behaviors that mimic addiction without meeting clinical definitions. The rise of processed foods, laden with added sugars, has made it easier for people to consume excessive amounts, leading to noteworthy health effects of sugar consumption. According to the American Heart Association sugar recommendations, excessive sugar intake can result in serious health complications, underscoring the need for awareness about our dietary choices and sugar cravings.
Exploring the potential addictive nature of sugar unveils a complex web of issues revolving around dietary habits and cravings. Terms like sweet dependency and sweet tooth often arise in discussions regarding our attraction to sugary foods, especially those found in highly processed items. These sugary substances, designed for maximum palatability, can trigger an intensely satisfying response, making it difficult to resist them. As individuals face escalating challenges with consumption, understanding the psychological and physiological implications of sugar addiction becomes crucial. By studying these relationships, we can garner insights into how to manage our intake and promote healthier eating behaviors.
Is Sugar Addictive? Understanding the Debate
The question of whether sugar is addictive has sparked considerable debate within the scientific community. While substances like alcohol and nicotine are classified as addictive substances due to their severe psychological and physiological effects, sugar does not fit neatly into this category. However, many individuals experience strong cravings for sugary foods, indicating that sugar does possess qualities that can lead to compulsive eating behaviors. Research has shown that sugar can activate the brain’s reward system, similar to other addictive substances, which complicates the conversation surrounding sugar addiction.
It is crucial to distinguish between physiological dependence and psychological cravings. Although some people may feel withdrawal-like symptoms when they reduce sugar intake, these effects tend to be milder than those associated with true addiction to drugs or alcohol. It’s the accessibility and appeal of sugar-laden, ultra-processed foods that make managing cravings challenging, leading to habitual consumption that can affect one’s health.
The contrasting viewpoints are important to consider when discussing the health effects of sugar. On one hand, moderate consumption is generally recognized as part of a balanced diet, but the overconsumption of added sugars can lead to negative health consequences such as obesity, diabetes, and cardiovascular disease. The American Heart Association recommends strict limits on added sugars—no more than 9 teaspoons for men and 6 teaspoons for women—to promote better health outcomes. Understanding that sugar is present in many nutrient-dense foods allows for a balanced view that supports moderation rather than total elimination.
The Impact of Sugar Cravings on Eating Habits
Sugar cravings can significantly influence an individual’s eating habits, often leading to the consumption of highly processed foods that are rich in added sugars. This change in dietary behavior can create a cycle of dependence, where the body craves more sugar to satisfy the initial desires, thus perpetuating the intake of unhealthy foods. These cravings can be particularly pronounced in times of stress, fatigue, or emotional distress, highlighting the psychological components tied to sugar consumption.
Research suggests that people who regularly consume high amounts of sugar are more likely to experience intense cravings, which can push them towards choosing sugary snacks over healthier options. This pattern is problematic, as it may lead to a cycle of unhealthy eating that is hard to break. Nutritional education, awareness, and mindful eating practices can help individuals recognize their cravings and make healthier choices without feeling deprived.
Furthermore, understanding the mechanism behind sugar cravings can empower individuals to make informed choices. Timing meals to include a balance of fiber, protein, and healthy fats can stabilize blood sugar levels and diminish the likelihood of sudden cravings. As lifestyle changes prove difficult, gradual reduction of added sugars in meals and snacks can help mitigate cravings without leading to overwhelming withdrawal-like symptoms. The goal should be to cultivate a health-focused environment that encourages mindful consumption and education about hidden sugars in processed foods.
Health Effects of Excess Sugar Consumption
The health effects of consuming excessive amounts of sugar are well-documented and extend beyond just weight gain. High sugar intake has been linked to various chronic diseases, including heart disease, diabetes, and fatty liver disease. Processed foods laden with sugars often lack essential nutrients, leading individuals to ingest empty calories that contribute to metabolic syndrome and obesity. This situation is compounded by the fact that many processed foods contain added sugars that go unrecognized by consumers, highlighting the necessity of reading food labels.
Moreover, the American Heart Association’s guidelines emphasize the long-term health risks associated with high sugar consumption. Limiting intake to recommended levels is key to reducing the risk factors associated with diet-related diseases. Understanding how much sugar is incorporated into daily foods allows for better dietary choices and supports public health initiatives aimed at reducing sugar consumption in the population.
In addition to physical health impacts, excessive sugar consumption can also affect mental well-being. Elevated blood sugar levels can lead to mood swings, fatigue, and an increased risk of depression. This relationship emphasizes the importance of considering both the psychological and physiological aspects of sugar intake and its cravings. By becoming more aware of sugar consumption and replacing unhealthy sugars with whole foods, individuals can enhance their overall health status and quality of life.
Navigating Sugar in a Processed Food World
In a world saturated with processed foods, navigating sugar consumption becomes a challenge for many individuals. Ultra-processed foods often contain high levels of added sugars, unhealthy fats, and sodium, making them exceptionally appealing and more likely to lead to overconsumption. This trend raises concerns over dietary habits and the public’s health as these foods contribute significantly to the average sugar intake, which currently exceeds the American Heart Association’s recommendations for added sugars.
To counteract this issue, consumers must develop skills in identifying sugar content in labels and making informed food choices. Engaging with whole foods and cooking meals from scratch can help mitigate the tendency towards grabbing sugary snacks, which are often designed for convenience rather than nutrition. Balancing the diet with fiber and nutrients while consciously reducing added sugars can lead to better health outcomes for individuals and families.
Furthermore, food manufacturers have a responsibility to reformulate their products and reduce added sugars to promote healthier options in the market. This shift requires collaboration between public health organizations and food producers to create a food environment that encourages healthy dietary patterns. By improving the accessibility of wholesome foods and enhancing nutrition education, we can support healthier eating habits and combat the rising prevalence of sugar-related health issues.
Combatting Sugar Addiction with Healthy Lifestyle Changes
Combatting sugar cravings and potential addiction necessitates a multifaceted lifestyle approach. One of the cornerstone strategies to reduce sugar intake effectively is through mindful eating practices. Individuals are encouraged to pay close attention to the types of foods consumed, focusing on natural sweeteners and whole foods that provide nourishment without the excessive sugar burden found in many snacks. These changes can lead to a more balanced consumption experience and reduce the overwhelming urge for sugary treats.
Incorporating regular physical activities can also help diminish sugar cravings. Exercise not only boosts mood and energy levels but also plays a significant role in regulating hormone levels that influence cravings. Engaging in moving activities encourages a healthier lifestyle overall and assists in offsetting the potential negative effects of occasional sugar indulgence.
Additionally, seeking support from professionals such as dietitians or nutritionists can provide tailored advice and strategies to help individuals manage their sugar cravings. These experts can assist in developing a personalized plan that aligns with one’s health goals, making the journey towards healthy eating both manageable and enjoyable. By fostering a supportive environment and building awareness around sugar consumption, individuals can cultivate a healthier relationship with food as they work towards reducing sugar’s presence in their diet.
Understanding the Role of Sweeteners in Our Diet
Understanding the role of sweeteners—both natural and artificial—in our diets is vital when discussing sugar addiction. While many seek to reduce their sugar intake, the market is flooded with alternatives, including stevia, agave nectar, and sugar alcohols. These sweeteners can satisfy cravings without the same caloric load or blood sugar impact, making them appealing for those looking to decrease their sugar consumption. However, it’s important to discern the health effects of these alternatives, as some may have their side effects or complicate the taste preferences that drive sugar consumption.
Moreover, the psychological impact of using substitutes can perpetuate sugar cravings rather than eliminate them. If individuals remain reliant on sweet tastes, they may struggle to achieve a balanced palate, leading to continued reliance on sweet foods and beverages. Comprehensively educating oneself about the profiles of various sweeteners and forming a preference for less sweetness can aid in reducing overall sugar dependency.
Ultimately, the goal should shift from merely avoiding sugar to fostering a holistic understanding of how different sweeteners play a role in overall health. This approach encourages consumers to experiment with various flavors and recognize that too much sweetness—regardless of the source—can lead to negative health consequences. By promoting awareness and reducing dependency on sweet flavors, individuals can foster a healthier relationship with food within the context of their dietary choices.
Tips for Gradually Reducing Sugar Intake
Making the decision to reduce sugar intake can feel overwhelming, but by taking gradual steps, this process can become much more manageable. One effective tip is keeping a food diary to track sugar consumption, which helps in identifying sources of added sugars in the diet. From sugary drinks to snacks, recognizing hidden sugars can empower individuals to make informed changes. This awareness can also help in setting realistic goals for reducing sugar without experiencing extreme cravings or discomfort.
Another strategy involves substituting sugary options with healthier alternatives. Rather than reaching for a candy bar, consider snacking on fruit or nuts, which can satisfy sweet cravings without the drawbacks of added sugars. Over time, these small changes can lead to a significant reduction in overall sugar intake, enhancing both health and well-being.
Finally, finding healthy ways to enjoy sweetness can also provide comfort while reducing dependence on high-sugar options. Integrating spices like cinnamon or vanilla extract can add a sweet flavor profile to dishes without the need for added sugars. This not only nurtures the satisfaction of taste but can also establish a new relationship with flavor in food—a relationship that emphasizes variety, balance, and health.
Frequently Asked Questions
Is sugar addictive like alcohol or nicotine?
While sugar can increase cravings and compulsive eating behaviors, it is not officially classified as an addictive substance like alcohol or nicotine. Current research suggests that though sugar has some addictive qualities, especially in the context of ultra-processed foods, it lacks the severe withdrawal symptoms associated with true addictive substances.
What causes sugar cravings and are they a sign of sugar addiction?
Sugar cravings can occur due to the palatable nature of sugary foods, often linked to habitual consumption. These cravings are intensified by processed foods high in sugar, unhealthy fats, and sodium. While these cravings can mimic signs of sugar addiction, they do not meet clinical criteria for addiction compared to substances like alcohol or nicotine.
What are the health effects of sugar consumption and should I be concerned?
Excessive sugar consumption can lead to a range of health issues, including obesity, diabetes, and heart disease. The American Heart Association recommends limiting added sugar to 9 teaspoons for men and 6 for women. Being mindful of sugar intake is crucial for maintaining overall health.
How can I reduce my sugar intake if I think I have a sugar addiction?
If you feel dependent on sugar, it’s advisable to gradually reduce your intake rather than going cold turkey, which can lead to withdrawal-like symptoms. Start by reading food labels, particularly on processed foods, and opt for healthier snacks with lower sugar content. This can help diminish sugar cravings over time.
What do the American Heart Association sugar recommendations suggest?
The American Heart Association recommends that men should limit their intake to no more than 9 teaspoons of added sugar per day, while women should consume no more than 6 teaspoons. Children should have even lower amounts, emphasizing the need to be aware of sugar consumption from processed foods and beverages.
Can sugar be part of a healthy diet without leading to addiction?
Yes, sugar can enhance flavor and texture in foods. It’s essential to distinguish between the natural sugars found in fruits and dairy versus added sugars in processed foods. Moderation is key; consuming low to moderate amounts of added sugar is usually safe and will not lead to significant health consequences.
Why are processed foods high in sugar so appealing and dangerous?
Processed foods are engineered to be highly palatable, containing added sugars that enhance flavor. This can lead to habitual eating patterns and heightened sugar cravings. The accessibility of these foods makes it challenging to limit intake, thus increasing potential health risks associated with overconsumption.
| Key Point | Details |
|---|---|
| Is Sugar Addictive? | Sugar is not classified as an addictive substance like alcohol or nicotine, according to current clinical criteria. |
| Physical and Psychological Effects | Sugar can increase cravings and compulsive eating, leading to withdrawal-like symptoms when stopped suddenly. |
| Ultra-Processed Foods | Foods high in added sugar, unhealthy fats, and sodium can exacerbate cravings due to their palatability. |
| Average Sugar Consumption | The average American consumes nearly 20 teaspoons of added sugar daily, far exceeding recommended limits. |
| Health Recommendations | American Heart Association recommends no more than 9 teaspoons for men, and 6 teaspoons for women. |
| Moderation is Key | Consuming sugar in moderation can enhance flavor and enjoyment, making it unnecessary to eliminate completely. |
Summary
Is sugar addictive? This question generates significant debate among nutritionists and researchers. While it shows addictive-like qualities in increasing cravings, sugar is not classified as an addictive substance like alcohol or nicotine based on strict clinical criteria. Unlike these substances, sugar is an essential part of our diet found in fruits and grains, suggesting we need a balanced approach to its intake. Therefore, understanding the impact of excessive sugar consumption and moderating its use can help avoid potential negative psychological effects while still enjoying its benefits.

Indoor Air Quality: How It Affects Your Health Now
Indoor air quality is a critical aspect that significantly impacts our health and overall well-being. In fact, the health effects of indoor air quality can range from mild symptoms like fatigue and concentration issues to more severe respiratory problems. Understanding the importance of ventilation is vital, as proper airflow can help to reduce indoor air pollutants that accumulate in our living and working spaces. Studies suggest that improving indoor air quality can lead not just to healthier buildings, but also to enhanced cognitive function and productivity. As we explore this topic further, the link between our environments and our physical health becomes increasingly evident.
When discussing the quality of air within buildings, we often underscore the effects it has on our physical health and daily functionality. The environments we inhabit—be it at home, in offices, or in educational settings—play a crucial role in determining how we feel and perform. Ensuring proper ventilation helps mitigate harmful airborne contaminants that can adversely affect our well-being. Additionally, a focus on establishing healthy indoor spaces can lead to substantial improvements in life quality and productivity. As we delve deeper into this subject, we will uncover various strategies for enhancing the air we breathe indoors.
Understanding Indoor Air Quality and Its Health Effects
Indoor air quality (IAQ) is a critical aspect of health that often goes unnoticed until it leads to tangible effects. Poor IAQ can have serious implications on physical health, contributing to conditions such as respiratory diseases, allergies, and even cardiovascular issues. The presence of common indoor air pollutants like mold, carbon dioxide, volatile organic compounds (VOCs), and particulate matter can compromise the environment in which we live and work, highlighting the urgent need to assess and improve indoor environments.
Moreover, the health effects of indoor air quality extend beyond physical ailments. Psychological impacts due to ongoing discomfort from poor air quality can lead to decreased productivity and increased stress levels. Studies have shown that individuals working in well-ventilated spaces with high IAQ report better cognitive function and mood, reinforcing the link between indoor conditions and overall well-being. Understanding this relationship empowers us to take necessary actions to enhance our indoor spaces and mitigate health risks.
Frequently Asked Questions
What are the health effects of indoor air quality?
Indoor air quality significantly impacts health. Poor air quality can lead to respiratory issues, headaches, fatigue, and can exacerbate allergies and asthma. Long-term exposure to indoor air pollutants may result in chronic health conditions.
Why is the importance of ventilation in maintaining indoor air quality?
Ventilation is crucial because it helps dilute indoor air pollutants and bring in fresh air. Proper ventilation reduces the concentration of harmful substances, improves overall air quality, and supports a healthier living environment.
How do healthy buildings impact indoor air quality?
Healthy buildings are designed with features that enhance indoor air quality, such as effective ventilation systems, use of non-toxic materials, and air filtration. These features can reduce pollutants and allergens, promoting better health and productivity.
What are some common indoor air pollutants that affect air quality?
Common indoor air pollutants include mold, dust mites, pet dander, volatile organic compounds (VOCs), and carbon monoxide. These pollutants can affect health and are often found in various household products and materials.
What are effective ways to improve indoor air quality?
Improving indoor air quality can be achieved by increasing ventilation, using high-efficiency air filters, reducing the use of VOCs and toxic chemicals, regularly cleaning and maintaining HVAC systems, and incorporating plants that help purify the air.
| Key Area | Details |
|---|---|
| Indoor Air Quality | Indoor air quality significantly impacts health, including cognitive functions and overall well-being. |
| Average Time Indoors | Americans spend about 80% of their lives indoors. |
| Effect of Ventilation | Increasing building air ventilation has been shown to improve cognitive function. |
| Source of Air Pollution | Indoor spaces can be a source of outdoor air pollution. |
| Impact of Neighboring Units | In an apartment, up to 30% of indoor air can come from neighboring units. |
| Infectious Disease Prevention | To reduce indoor spread of diseases, increase outdoor air, use better filters, and deploy HEPA filters. |
| Dust Composition | Dust can be hormonally active. |
| Chemical Regulations | Only about 200 out of 80,000+ chemicals have been banned by the EPA since 1976. |
Summary
Indoor air quality plays a crucial role in our health and well-being, influencing both cognitive function and overall wellness. As our lives are predominantly spent indoors, attention must be directed toward how buildings are designed and maintained to ensure adequate ventilation and minimize exposure to harmful pollutants. By improving indoor air quality through better ventilation, filtration, and awareness of pollutants, we can significantly enhance our work and living environments.