Age-Related Brain Disease: 17 Key Risk Factors Revealed
Age-related brain disease is an emerging public health concern, as its prevalence continues to rise with the aging population. Researchers have identified 17 key risk factors for dementia, stroke, and late-life depression that can significantly impact brain health. Modifying these risk factors not only fosters better cognitive function but also aids in stroke risk prevention. By embracing lifestyle changes, such as improving diet and increasing physical activity, individuals can take proactive steps to ensure their cognitive longevity. Implementing brain health tips based on these findings offers a comprehensive approach to reducing the burden of age-related brain diseases.
The term age-related brain disease encompasses a variety of conditions that affect cognitive functions in older adults, notably dementia, stroke, and late-life depression. These disorders are interconnected and share common underlying risk factors, which can be altered through lifestyle modifications. Understanding the implications of these health challenges allows for better strategies in preventive care. Keywords such as modifiable risk factors and brain health define the scope of this critical area of research, emphasizing the importance of early intervention. By addressing these issues, we can enhance overall well-being and quality of life in the aging population.
Understanding Age-Related Brain Disease and Its Risk Factors
Age-related brain diseases encompass a range of neurological disorders that significantly impact cognitive health as one ages. Notably, conditions such as dementia and stroke, linked by common thread risk factors, pose a considerable burden on individuals and healthcare systems. Understanding these risk factors is vital in mitigating their impact. Recent studies highlight that we can modify several risk factors that lead to these diseases, thus empowering individuals to take proactive steps towards brain health.
In the quest to understand the nuances of age-related brain disease, research has illuminated numerous shared risk factors. Factors such as high blood pressure and diabetes not only threaten cognitive function but also amplify the risks associated with stroke and late-life depression. By addressing these modifiable risk factors, individuals can significantly lower their risk and improve their overall quality of life—making a strong case for preventive strategies in public health.
The Interconnection Between Stroke, Dementia, and Late-Life Depression
Stroke, dementia, and late-life depression are intricately linked, forming a triad of conditions where the presence of one often predicates the others. For instance, individuals who experience a stroke are at an increased risk of developing dementia, and untreated depression can exacerbate cognitive decline. The intricate web of these conditions can create a cycle that is challenging to break without intervention targeting their common risk factors.
Research indicates that the impact of these interconnected diseases can extend beyond individual health, affecting caregivers and families significantly. With shared risk factors, such as smoking and inadequate physical activity, the importance of comprehensive health strategies to address these issues becomes increasingly clear. By promoting healthy lifestyle changes focused on modifiable factors, we can curtail the prevalence of this trio of age-related brain diseases.
Exploring Modifiable Risk Factors for Better Brain Health
Modifiable risk factors are crucial in the fight against age-related brain diseases. Identifying what can be changed empowers individuals to make significant improvements in their brain health. With 17 identifiable risk factors connecting stroke, dementia, and late-life depression, researchers encourage everyone to take stock of their health choices. By focusing on areas such as diet, physical activity, and social engagement, individuals can make strides toward mitigating their risk for these diseases.
For example, maintaining a balanced diet rich in omega-3 fatty acids and antioxidants can positively affect brain health while reducing the risk of developing dementia. Coupling this with regular exercise not only aids in physical health but also enhances mental well-being. These modifiable factors offer pathways to improve overall health outcomes and quality of life, reinforcing the significance of preventive healthcare measures.
The Role of Physical Activity in Preventing Brain Disease
Physical activity is one of the most impactful modifiable risk factors in preventing age-related brain diseases. Engaging in regular exercise is strongly linked to enhanced cognitive function and reduced risk of dementia and stroke. Exercise boosts blood circulation to the brain, promotes neurogenesis—the growth of new neurons—and can improve mood, thereby addressing components that contribute to late-life depression.
Moreover, activities that combine physical and cognitive challenges, such as dancing or team sports, have been linked to better brain health outcomes. By encouraging individuals to lead active lifestyles and incorporate movement into their daily routines, we can not only mitigate the risks associated with age-related brain diseases but also enhance overall life satisfaction and engagement.
The Importance of Diet in Maintaining Brain Health
Diet plays a pivotal role in maintaining brain health and preventing age-related brain diseases. Research has consistently shown that diets high in saturated fats and sugars are detrimental to cognitive function, while nutritious diets rich in fruits, vegetables, whole grains, and healthy fats can yield protective benefits. The Mediterranean diet, characterized by ample olive oil, nuts, fish, and high vegetable consumption, has been particularly associated with lower rates of dementia and stroke.
Additionally, the impact of hydration cannot be overlooked. Water intake is crucial for maintaining optimal brain function, and dehydration can exacerbate cognitive decline. As such, promoting dietary interventions that focus on whole, unprocessed foods alongside adequate hydration can greatly empower individuals to take charge of their brain health, ultimately diminishing the long-term risk of age-related diseases.
The Significance of Social Engagement for Cognitive Wellness
Social engagement is a vital component of brain health, influencing both emotional well-being and cognitive vitality. Studies indicate that maintaining strong social connections can significantly lower the risk of depression and may also act as a buffer against cognitive decline, including the onset of dementia. Engaging in regular social activities stimulates cognitive functioning and provides emotional support, fostering a sense of community that is crucial for mental health in later life.
Moreover, declining social interactions are often a precursor to many brain-related illnesses, including late-life depression. Therefore, facilitating opportunities for social engagement through community programs, support groups, or even regular family interactions can enhance quality of life and promote resilience against mental health issues. The benefits of social engagement thus reverberate across both mental health and cognitive longevity.
Quality Sleep and Its Impact on Brain Health
Quality sleep is a cornerstone of brain health that is often overlooked in discussions about age-related brain disease. Inadequate sleep can impair cognitive performance and increases the risk of developing conditions such as dementia and depression. Sleep facilitates essential processes like memory consolidation and toxin removal from the brain, making sufficient rest crucial for maintaining cognitive integrity throughout aging.
To promote better sleep, individuals should consider establishing consistent sleep routines, creating a bedtime environment conducive to rest, and limiting screen time before bed. These changes can foster improved sleep quality, which may, in turn, protect against the cognitive decline associated with aging. Investing in sleep health can thus yield substantial benefits for brain health and overall life quality.
Managing Stress to Protect Cognitive Function
Chronic stress has profound negative implications not only for mental health but also for cognitive function, increasing the risk of conditions such as late-life depression and dementia. High levels of cortisol, the stress hormone, are known to damage neuronal connections and impair cognitive processes such as memory and decision-making. Consequently, managing stress effectively is crucial for safeguarding brain health.
Strategies such as mindfulness meditation, yoga, and relaxation techniques can significantly reduce stress levels and promote mental resilience. Moreover, engaging in hobbies or activities that induce joy can also serve as effective stress relievers. By integrating these practices into daily life, individuals can mitigate the cognitive risks associated with prolonged stress exposure and enhance their overall well-being.
The Future of Brain Health: Innovative Tools and Strategies
As research into age-related brain diseases advances, innovative tools like the Brain Care Score have been developed to help individuals assess and improve their brain health. This score encompasses various modifiable risk factors and provides personalized recommendations for lifestyle changes conducive to better cognitive function. The simplicity and accessibility of this tool emphasize the importance of proactivity in disease prevention.
Future strategies may involve integrating these innovative solutions into healthcare systems, ensuring that individuals receive tailored advice on maintaining their brain health. By focusing on collective awareness and preventive measures, we can aim for a future where age-related brain diseases are less prevalent, allowing for healthier aging experiences. The ongoing commitment to research in this field will undoubtedly foster further advancements in how we approach and maintain cognitive health.
Frequently Asked Questions
What are the key risk factors for dementia that can lead to age-related brain disease?
Research has identified 17 modifiable risk factors for dementia and other age-related brain diseases, including high blood pressure, diabetes, kidney disease, high cholesterol, and excessive alcohol consumption. By addressing these factors, individuals may significantly reduce their risk of developing dementia.
How can managing blood pressure lower the risk of age-related brain diseases?
High blood pressure is a major risk factor for age-related brain diseases like dementia and stroke. Effective management of blood pressure through lifestyle changes such as diet, exercise, and medication can significantly lower the risk of these conditions.
What role does physical activity play in preventing age-related brain disease?
Insufficient physical activity is linked to a higher risk of stroke, dementia, and late-life depression. Engaging in regular physical activity can enhance brain health and reduce the risk of developing these age-related conditions.
How does poor diet contribute to age-related brain diseases?
A poor diet can increase the risk of stroke, dementia, and late-life depression. Diets high in processed foods and low in nutrients can exacerbate risk factors like obesity and high cholesterol, thereby elevating the risk of age-related brain diseases.
Can late-life depression increase the risk of developing dementia?
Yes, late-life depression is interconnected with dementia and stroke. Untreated depression can heighten the risk for these conditions, indicating the importance of addressing mental health alongside physical health to prevent age-related brain diseases.
What are some effective brain health tips to reduce the risk of age-related diseases?
Effective brain health tips include maintaining a balanced diet, engaging in regular physical exercise, managing stress, ensuring quality sleep, staying socially active, and pursuing mental challenges. These habits can help lower the risk of stroke, dementia, and late-life depression.
Why is social engagement important in preventing age-related brain disease?
Social engagement can reduce the risk of depression, which is linked to increased rates of dementia and stroke. Maintaining strong social connections can thus play a critical role in protecting brain health as individuals age.
What is the Brain Care Score and how does it relate to age-related brain disease?
The Brain Care Score is a tool developed to measure and guide efforts for safeguarding brain health. It incorporates the latest scientific findings on modifiable risk factors to help individuals take actionable steps in reducing the risk of age-related brain diseases like dementia and stroke.
Are there lifestyle changes that can reduce the risk of late-life depression and dementia?
Yes, several lifestyle changes, such as improving diet, increasing physical activity, enhancing social engagement, and seeking mental health support can be effective in reducing the risk of late-life depression, which is often linked to dementia and other age-related brain diseases.
How does stress management affect the risk of age-related brain diseases?
Chronic stress can lead to a greater risk of depression and other age-related brain diseases. Implementing stress management techniques such as mindfulness, exercise, and relaxation can help mitigate this risk and improve overall brain health.
| Risk Factor | Associated Conditions | Impact on Health |
|---|---|---|
| Diabetes | Stroke, Dementia, Depression | Increases risk significantly |
| Blood Pressure | All three conditions | Major risk factor affecting all |
| Kidney Disease | Stroke, Dementia, Depression | Elevates risks substantially |
| Fasting Plasma Glucose | All three conditions | High levels increase risks |
| Total Cholesterol | Stroke, Dementia | Elevated levels are harmful |
| Alcohol Use | Stroke, Dementia, Depression | Excess intake increases risks |
| Diet | All three conditions | Poor diet worsens conditions |
| Hearing Loss | Dementia | Modifiable risk factor |
| Pain | Depression, Others | Chronic pain increases risks |
| Physical Activity | All three conditions | Healthy activity lowers risks |
| Purpose in Life | Depression, Others | Lack increases depression risk |
| Sleep | Depression, Others | Inadequate sleep raises risks |
| Smoking | All three conditions | Strongly increases risks |
| Social Engagement | Depression, Others | Low engagement linked to risks |
| Stress | Depression, Others | Chronic stress heightens risks |
| Obesity | Stroke, Dementia, Depression | Increases risk significantly |
Summary
Age-related brain disease encompasses various conditions such as stroke, dementia, and late-life depression, which share interconnected risk factors. Recent research highlights 17 modifiable factors that individuals can alter to reduce the risk of these debilitating diseases, emphasizing the importance of lifestyle changes such as managing blood pressure and engaging in physical activity. The findings underline the potential for targeted prevention strategies to lower the overall incidence of these age-related brain diseases, ultimately improving quality of life for older adults. By addressing these modifiable risks, we can significantly lessen the burden of age-related brain diseases on individuals and society.
Take Yourself Less Seriously: Embrace Humor for Health
In today’s fast-paced world, we often forget the importance of humor and how it can be a vital tool for our mental health. Learning to take yourself less seriously is not just a whimsy idea; it fosters self-awareness and enhances your ability to connect with those around you. Engaging in self-deprecating humor can create a safe space that enables genuine relationships while alleviating feelings of anxiety or depression. By embracing laughter, we open the door to exploring the benefits of humor in our everyday lives, helping us navigate life’s challenges with grace and perspective. Ultimately, humor is not just about making jokes; it’s a powerful way to remind ourselves that it’s okay to be flawed and human, reinforcing our bonds with others in the process.
We live in an era where taking life too seriously can often lead to burnout and disconnection from the world. Approaching ourselves with lightheartedness allows for a breath of fresh air amidst the chaos of daily responsibilities. Adopting a playful attitude can break down barriers, revealing the strength that lies in vulnerability. Through laughter, we can share our struggles and flaws, fostering deeper connections with others. So, let us explore the lighter side of life, recognizing the profound impact that humor and self-awareness can have on our well-being.
Understanding Self-Deprecating Humor
Self-deprecating humor is a unique form of comedy where individuals make light-hearted jokes at their own expense. While it might sound negative at first, it actually reflects a form of self-awareness and confidence. When someone indulges in self-deprecating humor, they often show their ability to acknowledge their flaws, imperfections, and even mistakes without feeling overly threatened or defensive. This can create a safe space for genuine connection with others, as it breaks down barriers of superiority and superiority complexes. It informs the listener that it’s okay to be imperfect, lending to a more approachable and relatable demeanor.
Moreover, the benefits of self-deprecating humor extend into mental health. It allows individuals to cope with stress and anxiety by transforming perceived weaknesses into humorous anecdotes. This shift not only alleviates the weight of self-criticism but also fosters a sense of community, making others feel at ease in similar situations. The reassurance that everyone has flaws creates empathy among peers, promoting social benefits that enhance relationships. Thus, self-deprecating humor acts as a bridge for communication and connection, fostering understanding and enhancing one’s mental well-being.
The Psychological Benefits of Humor
Humor, especially when self-directed, can significantly contribute to mental health. The act of laughing at oneself can diffuse tense situations, making them feel less daunting. When individuals engage in self-deprecating humor, they not only lighten their emotional load but also cultivate resilience. This is because humor encourages perspective-taking and emotional regulation, two vital skills in maintaining mental wellness. By learning to laugh at life’s challenges, individuals can approach difficult circumstances with curiosity and openness rather than fear and anxiety.
Additionally, humor works as a therapeutic tool in various scenarios. In clinical settings, therapists often use laughter to break down resistance from clients brimming with stress or pain. When a clinician models self-deprecating humor, it invites clients to drop their guard and relate on a human level, fostering a more authentic therapeutic alliance. Humor reminds us of our shared vulnerabilities and the human experience, which can be incredibly healing. By normalizing flaws through laughter, we empower ourselves to seek help and express our feelings, ultimately promoting better emotional health.
Creating Connections Through Laughter
Humor, particularly self-deprecating humor, plays a crucial role in creating meaningful connections among individuals. In a world where everyone is battling their own challenges, humor serves as a reminder that we are not alone in our struggles. When someone makes light of their imperfections, it often resonates with people around them, allowing for shared laughter and mutual understanding. This sense of connection is vital in today’s social climate, where many feel isolated and disconnected. By creating common ground through humor, we can foster relationships based on empathy and shared experiences.
Furthermore, humor acts as a social lubricant that facilitates discourse, even in disagreements. For instance, during contentious conversations, introducing a light-hearted comment can ease tension, encouraging open dialogue rather than defensiveness. It reminds us that while differing opinions exist, we can still relate on a human level. Utilizing humor in this way promotes a culture of respect and tolerance, underlining that taking ourselves less seriously can pave the way for deeper connections and more productive conversations. Ultimately, laughter can be a powerful tool in bridging gaps between individuals from diverse backgrounds.
Balancing Humor and Self-Criticism
While humor can be incredibly beneficial, it’s essential to strike a balance between light-hearted self-criticism and harsh self-judgment. Self-deprecating humor should enhance self-awareness without leading to feelings of inferiority or self-loathing. A healthy use of humor allows individuals to acknowledge their shortcomings while fostering a positive self-image. If someone finds themselves leaning towards self-flagellation rather than constructive humor, it might indicate deeper issues of self-worth that need addressing. Recognizing this boundary is vital to ensure that humor serves its intended purpose of uplifting rather than degrading.
In contrast, when humor is used excessively to seek sympathy or attention, it can backfire, causing others to feel uncomfortable. The key lies in intention: if the expression of self-deprecating humor is a genuine attempt to connect and not a plea for validation, it can be incredibly effective. Taking oneself less seriously is not about diminishing one’s worth but understanding our shared humanity. This approach encourages a healthier perspective on self-criticism, allowing us to see humor as an ally in our journey toward personal growth and mental health.
Cultural Perspectives on Humor
Cultural backgrounds significantly influence how humor is perceived and utilized. In many Western societies, self-deprecating humor is embraced as a means of building relatability. The emphasis on individualism encourages people to express their flaws openly, which can lead to greater social cohesion. By sharing our vulnerabilities, we create a culture of acceptance where laughter can be a powerful unifying factor. This approach not only strengthens personal connections but also helps individuals navigate the complexities of social interactions with grace and humor.
On the other hand, in collectivist cultures, humor often manifests as playful banter among peers rather than self-directed jokes. This style of humor promotes camaraderie and allows individuals to tease one another in a loving manner, reinforcing community ties. While self-deprecating humor can feel foreign in these contexts, finding humor in the collective struggle can similarly foster connection and acceptance. Both forms highlight the universal role humor plays in human interactions, serving as a reminder that regardless of cultural differences, humor remains a vital tool in connecting, healing, and bridging divides.
Navigating Vulnerability Through Humor
Vulnerability is a crucial aspect of human interaction, and humor can often help individuals navigate this sensitive terrain. Self-deprecating humor invites others to embrace their vulnerability by demonstrating that it’s okay to be imperfect. When someone jokes about their shortcomings, it not only lightens the mood but also cultivates an environment where others feel safe to share their own experiences. This openness plays a pivotal role in fostering deeper relationships, as it breaks down walls that often prevent genuine conversations.
Moreover, using humor as a tool for vulnerability can enhance self-awareness. By laughing at ourselves, we gain insights into our traits and behaviors that we might otherwise shy away from confronting. This acknowledgment is the first step toward personal growth and healing, allowing us to navigate our emotional landscape without fear. In doing so, we create opportunities for others to connect on a deeper level, embracing our humanity in a way that celebrates both flaws and strengths.
The Role of Humor in Emotional Regulation
Emotional regulation is a crucial skill for managing feelings of anxiety and depression, and humor can serve as an effective tool in this process. By introducing humor into our daily lives, we can cultivate a more resilient mindset. Laughter triggers the release of endorphins, which contribute to a positive mood and help reduce stress levels. Engaging in self-deprecating humor allows individuals to confront their issues with a lighter heart. This approach not only alleviates immediate feelings of distress but also fosters long-term emotional resilience.
Additionally, humor can act as a buffer against negative emotions during challenging situations. Rather than succumbing to despair, individuals who employ humor can often reframe their experiences, enabling them to cope more effectively. This reframing process encourages a more balanced perspective on life, helping individuals understand that everyone faces challenges, and it’s okay to struggle. Thus, humor becomes not just a mechanism for connection, but a vital element in maintaining mental health and emotional stability.
Applying Humor for Personal Growth
Integrating humor into one’s personal development journey can lead to significant insights and growth. By embracing the lighter side of life, individuals can learn to accept their imperfections, which is essential for personal evolution. Utilizing self-deprecating humor fosters a mindset focused on growth rather than criticism, allowing for an atmosphere of encouragement and self-compassion. This nurturing approach enables individuals to explore their potential and acknowledge areas for improvement without fear of failure or judgment.
Moreover, humor encourages a sense of playfulness, which is often essential for creative thinking and problem-solving. When we take ourselves less seriously, we open up to new ideas and perspectives that can catalyze change. This playful mindset can enhance our ability to connect with others, create deeper relationships, and foster collaborative environments. Ultimately, applying humor thoughtfully serves not only as a tool for social connection but also as a catalyst for greater personal development and emotional intelligence.
Humor as a Catalyst for Change
Humor possesses the unique ability to challenge societal norms and stimulate discussions around important issues. When individuals utilize self-deprecating humor to address personal struggles or societal expectations, they make powerful statements that resonate with many. This approach can bring light to serious topics, allowing for dialogue that may otherwise be too uncomfortable to engage in. By laughing at ourselves and our unique life experiences, we can foster greater understanding within our communities and promote empathy and compassion.
In addition, humor can drive behavioral change by making difficult conversations more approachable. When discussing mental health, for instance, incorporating humor can diffuse tension and encourage openness. This creates a safe space where people feel empowered to share their own stories without fear of judgment. By embracing this approach, we pave the way for broader acceptance and understanding of mental health issues and the importance of seeking help. Ultimately, humor serves as a bridge for change, enlightening us to the realities of ourselves and those around us.
Frequently Asked Questions
How can I take myself less seriously to improve my mental health?
Taking yourself less seriously can positively impact your mental health by reducing stress and increasing resilience. Engaging in self-deprecating humor allows you to view your flaws and challenges with a lighter perspective, fostering self-awareness and acceptance. This shift can lead to improved emotional regulation and a stronger ability to connect with others.
What are the benefits of humor when learning to take yourself less seriously?
The benefits of humor, particularly self-deprecating humor, include fostering connections and creating a sense of safety in social interactions. It promotes relatability, helps diffuse tension, and enhances emotional clarity. By not taking yourself too seriously, you open the door for deeper relationships and greater acceptance of your imperfections.
Can self-awareness help me take myself less seriously?
Absolutely! Developing self-awareness allows you to recognize your strengths and weaknesses without harsh judgment. This understanding can lead to a healthy form of self-deprecating humor, where you acknowledge your flaws without negativity. Embracing this mindset helps cultivate both self-acceptance and likability.
What role does self-deprecating humor play in human connection?
Self-deprecating humor plays a pivotal role in human connection by indicating humility and vulnerability, signaling that it’s okay to be imperfect. It fosters an atmosphere of trust where individuals feel comfortable sharing their own flaws, thus strengthening social bonds and making interactions more enjoyable.
How can I balance humor with self-criticism when trying to take myself less seriously?
Balancing humor with self-criticism involves recognizing the intent behind your humor. Aim for lightheartedness that encourages joy and relatability rather than harsh self-judgment. Monitor the emotional responses your humor elicits—if it fosters connection and comfort, you’re on the right track.
What are the differences between individualistic and collectivist cultures in terms of humor and taking oneself seriously?
In individualistic cultures, self-deprecating humor is prevalent, promoting relatability and connection through personal flaws. Conversely, collectivist cultures often use humor that emphasizes community and camaraderie, poking fun at one another in a good-natured way. Understanding these differences can enhance your ability to connect through humor in diverse settings.
How can taking yourself less seriously lead to better social interactions?
Taking yourself less seriously contributes to better social interactions by reducing defensiveness and enhancing approachability. When you can laugh at yourself, it invites others to do the same, creating an environment of joy, acceptance, and mutual understanding. This openness can break down social barriers and foster deeper connections.
Is self-deprecating humor always healthy, or can it be a sign of low self-esteem?
While self-deprecating humor can facilitate connection and demonstrate humility, it can sometimes mask underlying issues of low self-esteem. It’s important to distinguish between playful self-reflection and negative self-talk. Healthy humor should uplift rather than diminish self-worth, so be mindful of your tone and context.
How does humor act as a tool for emotional regulation?
Humor acts as a tool for emotional regulation by diffusing tension and providing perspective. When you engage in self-deprecating humor, it helps to lighten burdens and invites a sense of clarity. This can lead to improved coping strategies in challenging situations and enhances your ability to manage emotional responses constructively.
Why is it important to learn how to take myself less seriously?
Learning to take yourself less seriously is important because it contributes to a healthier mindset and social life. By embracing imperfections and practicing self-deprecating humor, you foster resilience, improve mental health, and create authentic connections, thus enhancing your overall quality of life.
| Key Point | Explanation |
|---|---|
| Self-deprecating Humor | A category of humor that allows individuals to make light of their own flaws without negative self-judgment. |
| Benefits in Therapy | Used by therapists to help patients with anxiety and depression by fostering connection and safety. |
| Self-awareness and Acceptance | Individuals who use self-deprecating humor are often humble, self-aware, and confident in acknowledging their flaws. |
| Cultural Differences | Self-deprecating humor is prevalent in individualistic cultures, while collectivist cultures often tease others rather than themselves. |
| Avoiding Extremes | Extreme self-criticism can lead to negative feelings; moderation in taking oneself seriously is encouraged. |
| Building Connections | Humor can bridge disagreements and enhance connections, emphasizing that everyone has struggles. |
Summary
Taking yourself less seriously is essential for personal well-being and social connection. By embracing self-deprecating humor, you open the door to vulnerability and relatability, which enhances your interactions with others. Rather than dwelling on flaws, this approach allows people to recognize their humanity and foster connections through shared experiences. Ultimately, practicing self-deprecating humor can lighten life’s burdens and promote a more balanced, joyful existence.
Black Infant Mortality Rates: A Growing Concern in America
Black infant mortality remains a pressing issue in the United States, highlighting significant racial health disparities within the healthcare system. Recent studies reveal that, despite improvements in overall life expectancy and mortality rates for both Black and white Americans, Black infants are now dying at alarming rates—almost twice that of their white counterparts. This concerning trend underscores the healthcare inequality that persists across racial lines, revealing how systemic discrepancies adversely impact Black Americans’ health outcomes. Medical conditions during pregnancy are often cited as contributing factors to this elevated mortality rate among Black infants, emphasizing the need for equitable access to quality healthcare. With Black infant mortality rates demonstrating concerning growth since the 1950s, it’s crucial that policymakers prioritize addressing these disparities to ensure all infants have the opportunity for a healthy start in life.
The issue of infant mortality among Black populations presents a significant public health challenge, reflecting broader themes of healthcare inequality and racial inequity in the United States. Disparities in infant survival rates not only illuminate the pressing healthcare challenges faced by Black families but also highlight the urgent need for systemic change within healthcare delivery. Research into healthcare outcomes reveals that, while general life expectancy is on the rise for many Americans, Black infants suffer disproportionately high mortality rates, reinforcing the critical need for targeted interventions. Inequitable access to healthcare resources is a key factor driving these stark disparities, raising questions about the fairness of healthcare systems in addressing the needs of diverse populations. As we delve deeper into the factors contributing to these life expectancy disparities, it becomes imperative for researchers and authorities to adopt inclusive measures to safeguard the health of all infants, irrespective of their racial background.
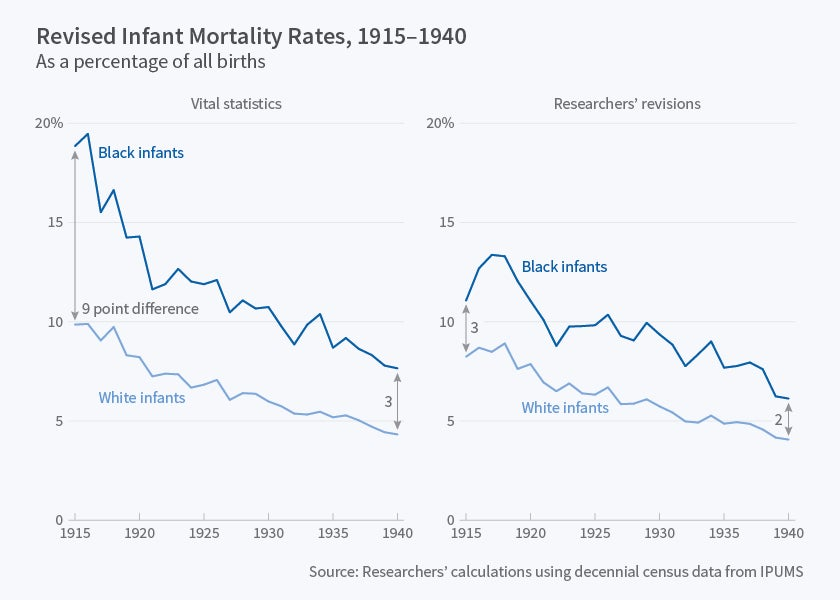
The Widening Disparity in Black Infant Mortality Rates
Research indicates that Black infant mortality rates have shown a disturbing trend, worsening from a 92% disparity compared to white infants in the 1950s to a staggering 115% today. This rise highlights a crucial public health crisis despite advances in healthcare that have generally improved life expectancy for other demographics. The data reflects that, while racial health disparities have narrowed for adult populations, the situation for Black infants is critically worrying, emphasizing a significant area that requires immediate attention from healthcare policymakers.
The factors contributing to these rising mortality rates among Black infants are complex and multifaceted. The leading causes of these deaths primarily involve medical issues associated with pregnancy and infancy, which stem from systemic healthcare inequality faced by many Black Americans. Access to quality prenatal and postnatal care is severely limited for many families, pointing to the urgent need for interventions to tackle these inequities. Without systemic changes in healthcare access and quality, these rates are unlikely to improve.
Addressing Racial Health Disparities in Infant Mortality
To combat the staggering differences in infant mortality rates, it is essential for public health officials and researchers to focus on the underlying factors that lead to these disparities. This includes analyzing healthcare inequality in terms of both access and quality of care for expecting mothers. Enhanced programs supporting Black Americans in healthcare, along with community-based initiatives, could potentially bridge this gap and lead to better outcomes for infants.
Moreover, policymakers must prioritize comprehensive interventions aimed at reducing life expectancy disparities linked to race. This calls for increasing funding for maternal health programs targeted at underserved populations, ensuring equitable distribution of healthcare resources, and implementing educational initiatives that raise awareness about these critical health issues. By addressing the root causes of infant mortality rates in the Black community, steps can be taken to prevent the loss of countless young lives, thereby improving overall public health.
Healthcare Inequality: A Barrier to Better Outcomes for Black Infants
Healthcare inequality remains a substantial barrier to improving health outcomes for Black infants, with disparities rooted deeply in societal and systemic issues. For too long, the focus has largely been on broader health metrics without addressing the specific challenges faced by marginalized communities, particularly relating to infant health. The lack of access to quality medical care and the pervasive mistrust in healthcare systems mean that many Black families do not receive adequate support during pregnancy and childbirth.
There is an urgent need to dismantle these barriers through targeted policies that promote health equity. Initiatives that emphasize inclusive healthcare practices and address social determinants of health can help shift the narrative around Black infant mortality. Creating programs that specifically cater to the needs of Black mothers and infants can provide the necessary support and education to improve healthcare experiences, thereby potentially reducing the infant mortality rates that have been persistently high.
The Importance of Longitudinal Studies on Infant Mortality
The examination of long-term data on infant mortality rates across different racial groups reveals significant insights that shorter-term studies might overlook. Understanding the changes over a 70-year period allows researchers to contextualize health improvements and disparities within broader societal trends. This comprehensive view underscores the importance of sustained focus on healthcare outcomes for vulnerable populations, particularly Black infants who continue to face disproportionately high mortality rates.
Historically, the narrative around healthcare has often highlighted improvements in life expectancy, yet without addressing the fundamental racial disparities that persist, we risk ignoring large segments of the population. Longitudinal research should continue to be a priority to ensure healthcare reforms are informed by data that accurately reflects the realities faced by Black infants and their families. By shedding light on these long-term trends, stakeholders can better advocate for policies that aim to rectify historical injustices within healthcare systems.
Policy Recommendations to Reduce Black Infant Mortality
To reverse the alarming trend of rising Black infant mortality rates, concrete policy recommendations must be established. This includes increasing funding for prenatal care programs specifically designed for at-risk populations. Efforts should focus on expanding healthcare access through community clinics, mobile health units, and telehealth services that can reach isolated areas. Additionally, there should be incentives for healthcare providers to prioritize care for Black mothers and infants.
Moreover, there is a need for public awareness campaigns that educate expectant families about available resources and support systems. Initiatives that foster partnerships between community organizations, healthcare providers, and local governments can lead to more sustainable changes in healthcare delivery for Black families. The goal should be to create a healthcare environment where every infant, regardless of race, has an equitable opportunity for a healthy start in life.
Community Health Initiatives and Their Impact on Infant Mortality
Community health initiatives have emerged as critical components in addressing infant mortality disparities among Black infants. By implementing localized programs that provide education, resources, and support, these initiatives can significantly influence health outcomes. Programs that engage with community leaders and empower families with knowledge about prenatal and infant care have shown promise in improving healthcare access and reducing mortality rates.
Additionally, community-based approaches often foster a sense of trust and collaboration between healthcare providers and families. Such partnerships can enhance the effectiveness of health interventions, transforming how care is delivered to marginalized populations. As stakeholders continue to investigate innovative healthcare solutions, the importance of grassroots movements in tackling infant mortality cannot be overstated, particularly for vulnerable communities.
The Role of Education in Reducing Healthcare Disparities
Education plays a crucial role in mitigating healthcare disparities and improving outcomes for Black infants. Parents with greater knowledge about maternal health, infant care, and available healthcare resources are better equipped to make informed decisions. Educational initiatives tailored to underserved communities can help bridge the gap and empower families to seek the necessary care and support for their infants.
Moreover, educational programs that incorporate cultural competence can enhance the effectiveness of health communication. By recognizing and valuing the unique experiences of Black families, healthcare providers can foster a more inclusive environment that encourages families to engage actively with their healthcare. Prioritizing education in the fight against infant mortality not only raises awareness but also helps cultivate a generation that advocates for its health and well-being.
Innovations in Healthcare Delivery for Black Infants
Innovations in healthcare delivery have the potential to revolutionize the approach to reducing Black infant mortality rates. The integration of technology, such as telemedicine and remote monitoring, can provide vital support to families who may face geographic or logistical challenges in accessing care. These technologies can offer timely advice and treatment options, bridging gaps where traditional healthcare systems fall short.
Furthermore, community health workers can play an essential role in these innovations, acting as liaisons between families and healthcare providers. By delivering personalized care and support directly within communities, these individuals can help ensure that Black infants receive the critical resources and assistance needed during the first years of life. As we explore new delivery models, the focus must remain on enhancing equity and accessibility within healthcare systems.
Future Directions in Research on Black Infant Mortality
Future research on Black infant mortality must be comprehensive and multifaceted, addressing the complexity of the issues at hand. Longitudinal studies are crucial in uncovering trends over time, while qualitative research can provide insights into the experiences of families navigating the healthcare system. These efforts should aim to identify specific barriers that contribute to high mortality rates, informing targeted interventions.
The inclusion of diverse voices in research is equally important to capture a full spectrum of experiences. Collaborations between academic institutions, community organizations, and policymakers can enhance the relevance and impact of research findings. Moving forward, a collective approach towards understanding and addressing the factors leading to Black infant mortality will be essential in paving the way for effective solutions and improved health outcomes.
Frequently Asked Questions
What is the current status of Black infant mortality rates compared to other racial groups?
Black infant mortality rates remain significantly higher than those of white infants, with Black infants dying at nearly twice the rate of white infants. Research data shows that while overall life expectancy has improved for both Black and white Americans, the racial disparity in infant mortality has tragically widened since the 1950s.
How do racial health disparities affect Black infant mortality?
Racial health disparities play a critical role in Black infant mortality. Despite advancements in healthcare, Black infants face higher mortality rates largely due to systemic factors such as access to quality care, prenatal healthcare conditions, and socioeconomic challenges, all of which contribute to healthcare inequality.
What are the main causes of Black infant mortality in the United States?
The leading causes of Black infant mortality are medical conditions during pregnancy and complications linked to maternal health. Many of these issues stem from healthcare inequality, where Black mothers often have less access to quality prenatal care, resulting in higher rates of infant death.
Why has the disparity in infant mortality rates between Black and white infants persisted for decades?
The persistence of this disparity is attributed to ingrained systemic issues, including inequalities in healthcare access, differences in the quality of care, and socio-economic factors affecting Black Americans. Despite improvements in overall healthcare metrics, targeted efforts to address these specific disparities have been insufficient.
What measures can be taken to reduce Black infant mortality rates?
Reducing Black infant mortality rates requires comprehensive public health policies focused on improving access to healthcare for Black mothers and infants. Initiatives should prioritize equitable healthcare resources, better prenatal care access, and targeted community health programs to address underlying socio-economic factors.
How can we inform policies to address Black infant mortality effectively?
To address Black infant mortality effectively, policymakers need to focus on data-driven approaches that highlight systemic inequalities in healthcare. Research studies, like the one conducted over 70 years, can provide crucial insights to inform strong public health policies designed to equalize healthcare access and improve maternal and infant health outcomes.
What impact could closing the gap in Black infant mortality rates have on overall public health?
Closing the gap in Black infant mortality rates could significantly improve overall public health by saving an estimated 5 million Black American lives over the past 70 years. It would also lead to healthier generations, increased life expectancy, and economic benefits through reduced healthcare costs associated with infant mortality.
What role does maternal healthcare play in Black infant mortality rates?
Maternal healthcare is a major factor influencing Black infant mortality rates. Adequate prenatal and postnatal care can prevent complications during pregnancy and childbirth. Improving maternal healthcare for Black Americans can thus directly impact and reduce infant mortality rates in this population.
| Key Points |
|---|
| Black infant mortality rates are twice that of white infants as of 2019. |
| The gap in overall mortality rates between Black and white Americans has narrowed since the 1950s, yet the situation for infants has worsened. |
| Life expectancy has increased for both Black (60.5 to 76 years) and white Americans (69 to 79.3 years) from the 1950s to the 2010s. |
| The disparity in infant mortality has grown from a 92% higher rate for Black infants vs white infants in the 1950s to a 115% difference today. |
| Leading causes of infant mortality include medical conditions during pregnancy, healthcare inequality, and lack of access to quality care. |
| Research indicates that if Black Americans had equal healthcare to white Americans, approximately 5 million Black lives could have been saved over the past 70 years. |
Summary
Black infant mortality remains a significant public health crisis, with recent studies revealing that Black infants die at twice the rate of white infants. Despite improvements in overall life expectancy for both races, the disparity in infant mortality has widened over the past 70 years. Medical conditions during pregnancy and systemic healthcare inequalities are major contributing factors to these tragic statistics. It is crucial for public health officials and policymakers to prioritize addressing these disparities to ensure equitable healthcare access and ultimately improve outcomes for Black infants.

Exercise and Colon Cancer Survival: A Game Changer for Patients
Exercise and colon cancer survival have become pivotal topics in cancer research, particularly as new studies unveil the benefits of physical activity during recovery. Recent findings from the Dana-Farber Cancer Institute suggest that engaging in regular exercise after stage 3 colon cancer treatment may significantly improve survival rates for patients, bridging the gap between cancer survivors and the general population. The study highlights how physical activity not only enhances overall well-being but could also contribute to better long-term outcomes, reducing risk factors associated with recurring cancer. As patients navigate their recovery, incorporating exercise into their routine emerges as a crucial element of colon cancer treatment. This aligns with the growing understanding that cancer recovery exercise can play an essential role in enhancing life expectancy and quality for survivors.
The relationship between physical fitness and longevity in cancer survivors extends beyond just basic health; it encapsulates a more comprehensive approach to cancer recovery. Terms like physical activity benefits and wellness activities for colon cancer patients are gaining prominence as research emphasizes their critical role in enhancing not just survival rates but overall quality of life post-diagnosis. By focusing on cancer recovery strategies, particularly in the context of advanced stages such as stage 3 colon cancer, we can appreciate how exercise fundamentally changes patient outcomes. Understanding this nexus lays the groundwork for tailored cancer treatment plans that include structured physical activity as a fundamental aspect of care. Thus, exploring the implications of maintaining an active lifestyle post-treatment could unlock a new chapter in improving survival rates for those affected by colon cancer.
Understanding the Role of Exercise in Colon Cancer Survival
Research has shown that engaging in regular physical activity significantly contributes to improved survival rates for patients recovering from colon cancer. In the context of stage 3 colon cancer, studies have found that individuals who maintain higher activity levels post-treatment tend to reflect survival rates that are quite close to those of the general population. This robust connection between exercise and survival outcomes highlights the critical role that physical activity plays in the recovery process, allowing patients to regain a sense of normalcy and hope after a challenging diagnosis.
Moreover, a closer examination of the data reveals that patients who reported engaging in 18 or more MET-hours of exercise each week experienced minimal differences in survival rates compared to their healthier counterparts. The implications of these findings are profound, suggesting that not only does physical activity assist in physical recovery, but it also mitigates the psychological burden that often accompanies a cancer diagnosis. Regular exercise serves as a vital component of post-treatment care that can pave the way for better health outcomes.
Frequently Asked Questions
How does exercise impact colon cancer survival rates?
Regular physical activity significantly improves survival rates for individuals diagnosed with colon cancer, particularly those who have undergone treatment for stage 3 colon cancer. According to studies from Dana-Farber Cancer Institute, higher levels of physical activity (18 or more MET-hours per week) correlate with survival rates closer to those of the general population, reducing disparities in outcomes for cancer survivors.
What are the benefits of physical activity during colon cancer treatment?
Engaging in physical activity during colon cancer treatment offers several benefits, including enhanced recovery, improved overall health, and increased survival rates. Patients who report higher levels of activity post-treatment, particularly after surgery and chemotherapy for stage 3 colon cancer, show significantly better long-term survival rates compared to those with lower activity levels.
Can exercise help reduce disparities in colon cancer survival?
Yes, exercise can help reduce disparities in survival rates for colon cancer patients. Research shows that those who are physically active after treatment have survival rates that closely align with the general population, indicating that regular exercise plays a crucial role in improving outcomes for cancer survivors.
What types of exercise are recommended for colon cancer survivors?
Colon cancer survivors are encouraged to incorporate a variety of physical activities into their routines, such as walking, cycling, or swimming. Even short bouts of activity, like 10 to 20 minutes of exercise, have been shown to contribute to improved survival rates after stage 3 colon cancer treatment.
How much physical activity is necessary to improve survival rates in colon cancer patients?
To improve survival rates, colon cancer patients should aim for at least 18 MET-hours of physical activity per week. This level of activity has been associated with better overall survival rates, particularly among those who have been treated for stage 3 colon cancer.
Is it too late to start exercising after colon cancer treatment?
No, it is never too late to start exercising after colon cancer treatment. Engaging in physical activity, even at low levels, can still provide benefits and contribute to better health outcomes and improved survival rates for colon cancer survivors.
Do age and diagnosis impact the effects of exercise on colon cancer survival?
While age at the time of diagnosis may vary among colon cancer patients, the benefits of exercise on survival rates remain significant across different age groups. Research indicates that increased physical activity positively affects survival regardless of a patient’s age.
What is the relationship between exercise and cancer recurrence in colon cancer patients?
Exercise has been shown to lessen the likelihood of cancer recurrence among colon cancer patients. Those with higher activity levels exhibit better overall survival rates, even in cases where the cancer recurred within three years of treatment.
| Key Point | Details |
|---|---|
| Importance of Exercise | Regular physical activity can significantly improve long-term survival rates for stage 3 colon cancer patients. |
| Survival Disparities | Exercise narrows the gap in survival rates between colon cancer patients and the general population. |
| Activity Levels and Survival Rates | Patients active with 18+ MET-hours per week showed survival rates closer to the general population. |
| Low Activity Impact | Low activity leads to a 50.5% lower survival rate for recurrent cancer patients compared to the general population. |
| Risk Factors | Survival benefits from exercise are observed regardless of patient age at diagnosis. |
| Duration of Study | Study followed patients for an average of 5.9 to 6 years after treatment. |
Summary
Exercise and colon cancer survival are closely linked, with studies showing that regular physical activity after treatment can drastically improve survival rates for patients. This research demonstrates the significant impact exercise has in narrowing survival discrepancies between colon cancer patients and the general population, indicating that encouraging exercise post-treatment may enhance overall outcomes and quality of life for survivors.
Cancer Risk: Trustworthy Insights and Facts from Harvard
Cancer risk is an ever-present concern in today’s health discussions, often intertwined with prevalent myths about cancer and misconceptions surrounding it. As individuals strive for wellness, understanding cancer prevention tips and making healthy lifestyle choices becomes vital in minimizing these risks. Amidst a constant stream of information, discerning trustworthy sources can be challenging, which is where the Harvard cancer research initiatives come into play. They empower individuals with tools like the Cancer FactFinder, helping to clarify what really influences cancer risk. By leveraging research and evidence-based insights, we can take actionable steps towards reducing our chances of developing this formidable disease.
When discussing the threat of various malignancies, it is essential to understand the factors that elevate susceptibility to such diseases. Terms like cancer susceptibility and malignancy risk convey the same urgent message to those seeking to maintain their health. As people navigate the labyrinth of information available, discerning fact from fiction in their quest for a healthier lifestyle is crucial. Engaging with reliable resources can illuminate pathways to cancer prevention, enabling individuals to combat this pervasive health challenge effectively. By anchoring our decisions in scientific research, particularly initiatives from esteemed institutions like Harvard, we can confidently tackle the complexities of cancer risk.
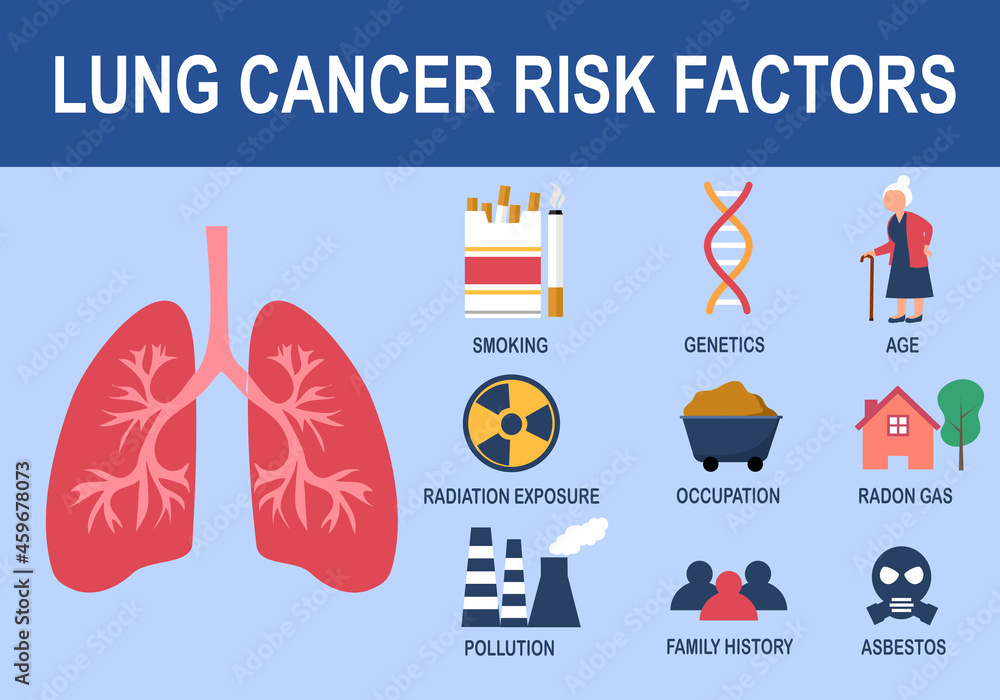
Understanding Cancer Risk Factors
Cancer risk factors can vary widely, influenced by lifestyle choices, genetics, and environmental exposures. Researchers emphasize that certain behaviors, such as smoking, excessive alcohol consumption, and poor dietary habits, significantly increase the risk of developing various forms of cancer. For instance, consistent studies link high alcohol consumption as a leading preventable cause of cancer, underscoring the importance of moderation and awareness in personal habits.
Additionally, not all cancer risks are easily identifiable; some may stem from mundane daily activities. For example, the consumption of processed meats and charred foods has been flagged by the International Agency for Research on Cancer as potentially carcinogenic. Recognizing these risks and understanding their implications allows individuals to make more informed decisions that could aid in cancer prevention.
Healthy Lifestyle Choices for Cancer Prevention
Adopting a healthy lifestyle is pivotal in reducing cancer risk. Incorporating balanced nutrition, regular physical activity, and maintaining a healthy weight can lower the chances of developing cancer. Diets rich in fruits, vegetables, and whole grains are frequently recommended, as they are believed to bolster the body’s defenses against various diseases, including cancer. Moreover, regular exercise has been shown to help manage weight and alleviate stress, both of which are significant contributors to cancer risk.
In addition to diet and exercise, adequate sleep is often overlooked but plays a crucial role in overall health and cancer prevention. Disruptions in sleep patterns can hinder the body’s ability to repair itself and maintain a healthy immune system. By prioritizing sleep and forming consistent routines, individuals can enhance their overall well-being and reduce the likelihood of cancer development.
Debunking Myths About Cancer
Misinformation surrounding cancer has led to numerous myths that can misguide the public and diminish awareness of genuine preventive measures. One prevalent myth is that certain lifestyle factors have no bearing on cancer risk, such as the often-cited belief that only certain demographics, like older adults or smokers, need to worry about cancer. In fact, research shows that low physical activity, obesity, and chronic stress are all significant risk factors regardless of one’s age or personal habits.
Using tools like the Cancer FactFinder can help dispel these myths, offering research-backed insights into the real risks associated with lifestyle choices. This resource not only educates the public but also encourages individuals to actively engage in behaviors that align with cancer prevention, debunking false claims and promoting healthier living.
The Role of Nutrition in Cancer Prevention
Dietary choices have been closely linked to cancer risk, and certain foods are recognized for their potential cancer-fighting properties. For example, turmeric, a spice renowned for its anti-inflammatory qualities, has been suggested to have cancer-preventive effects. However, ongoing research is essential to substantiate these claims and inform the public about effective dietary strategies for cancer prevention.
In contrast, processed and charred meats have been linked to increased cancer risk, prompting health experts to encourage individuals to limit their intake of these foods. Understanding the nutritional elements that contribute to cancer risk and prevention can empower people to make healthier choices, fostering lifelong habits that could significantly influence their overall health.
Examining the Myths Around Alcohol and Cancer
Alcohol consumption remains a contentious topic in discussions about cancer risk. Evidence from the U.S. Surgeon General paints a clear picture, highlighting excessive alcohol as a leading preventable cause of various cancers. Despite this, many continue to dismiss the connection, fueled by myths suggesting that moderate drinking poses no risk. This illustrates the necessity for education on the true risks associated with alcohol intake.
Furthermore, it’s essential to understand how even moderate drinking can contribute to increased cancer risk over time. By examining the facts and figures provided by research institutions, individuals can make informed decisions about their alcohol consumption, aligning their habits with cancer prevention efforts and fostering a culture of awareness around health.
The Impact of Sleep on Cancer Risk
Quality sleep is vital for maintaining overall health and well-being, playing a lesser-known but crucial role in cancer prevention. Medical studies have shown that disrupted sleep patterns can affect the body’s immune system, directly influencing its ability to fend off diseases, including cancer. Those who overlook the importance of sleep may unwittingly increase their cancer risk, emphasizing the need for awareness and prioritization of healthy sleep habits.
Furthermore, creating a consistent sleep schedule and ensuring a restful environment can significantly enhance sleep quality. By recognizing the connection between sleep and health, individuals can take proactive steps toward preventing cancer and promoting longevity through better sleep hygiene practices.
Facts and Fiction: The Cancer Fact Checker
With the endless stream of information available about cancer, it often becomes difficult to distinguish between facts and fiction. Harvard’s Cancer FactFinder tool seeks to illuminate the truth by allowing users to explore common claims related to cancer risk and prevention. This resource not only helps debunk myths but also guides individuals toward healthier lifestyles by providing research-based answers.
Emphasizing accurate information is crucial, particularly in an age where misinformation can spread rapidly through social media. By utilizing tools like the Cancer FactChecker, individuals can arm themselves with the critical knowledge needed to make informed health decisions, ultimately contributing to the broader public understanding of cancer prevention.
The Link Between Stress and Cancer Risk
Stress is often overlooked in conversations about cancer risk, yet research suggests that it plays a significant role in the overall health of individuals. Chronic stress may weaken the immune system, making it less effective at combatting the early stages of cancer development. Therefore, managing stress through various techniques like mindfulness, therapy, or regular physical activity becomes paramount in the quest for cancer prevention.
By incorporating stress-reduction practices into daily life, individuals can not only improve their mental health but also bolster their physical health significantly. Recognizing the intertwined relationship between stress and cancer risk can empower individuals to take control of their overall well-being, aligning their lifestyles with cancer prevention strategies.
Cancer Awareness: Recognizing High-Risk Groups
Cancer does not discriminate. However, certain demographic groups are identified as being at a higher risk for specific cancers, such as Black men for prostate cancer. Recognizing these high-risk groups is essential for early detection and preventive measures. By raising awareness and ensuring that individuals understand their specific risks, healthcare providers can encourage routine screenings and proactive health behaviors that may prevent cancer onset.
Moreover, education plays a crucial role in awareness efforts. By providing targeted information about the risks faced by high-risk groups, healthcare initiatives can better serve these communities, ensuring they have access to necessary resources for cancer prevention. Emphasizing the importance of regular check-ups and screenings can ultimately lead to improved health outcomes for these populations.
Engaging with Ongoing Research on Cancer Prevention
Continuous research is pivotal in advancing our understanding of cancer prevention. Institutions like Harvard T.H. Chan School of Public Health are at the forefront of this endeavor, conducting studies that examine the effectiveness of various lifestyle factors in reducing cancer risks. Engaging with the latest findings equips individuals with the knowledge to adjust their habits and enhance their lifestyles accordingly.
Staying informed about new cancer research findings not only educates the public but also encourages a collaborative approach to health and wellness. By relying on reputable sources and supporting ongoing studies, individuals can contribute to the collective effort to fight cancer and promote healthy living in their communities.
Frequently Asked Questions
What are some cancer prevention tips related to lifestyle choices?
To lower cancer risk, consider adopting these cancer prevention tips: maintain a healthy weight, engage in regular physical activity, limit alcohol consumption, and eat a balanced diet rich in fruits and vegetables. Making these healthy lifestyle choices can significantly impact your overall cancer risk.
Are there common myths about cancer risk that I should be aware of?
Yes, there are several myths about cancer risk that can mislead individuals. For example, many believe that stress alone can cause cancer, which is not supported by research. It’s important to use a reliable cancer fact checker, like the Harvard Cancer FactFinder, to debunk such myths and understand actual risk factors.
How does a healthy lifestyle influence cancer risk?
A healthy lifestyle greatly influences cancer risk. By maintaining a balanced diet, exercising regularly, avoiding smoking, and limiting alcohol intake, you can reduce your chances of developing certain types of cancer. Consistently making healthy lifestyle choices works together to lower overall cancer risk.
What’s the role of Harvard cancer research in understanding cancer risk?
Harvard cancer research plays a crucial role in understanding cancer risk by providing evidence-based insights into lifestyle factors and environmental exposures. The findings support initiatives like the Cancer FactFinder, which helps individuals make informed decisions about their health and risk for cancer.
Can coffee consumption really affect cancer risk?
Research indicates that coffee consumption may actually decrease cancer risk for certain types of cancer. It’s important to review studies and consult reliable sources, such as Harvard’s cancer research, to get accurate information about how various dietary factors relate to cancer risk.
Why should I consider using a cancer fact checker?
Using a cancer fact checker, such as the one developed by Harvard, helps you verify claims about cancer risk. It separates fact from fiction regarding lifestyle choices, diet, and environmental factors, enabling you to make informed health decisions and reduce your cancer risk.
| Key Point | Details |
|---|---|
| Cancer Risk Awareness | There’s a plethora of information about cancer risk available that can often be misleading. Identifying trustworthy sources is important. |
| Cancer FactFinder Tool | Developed by Harvard T.H. Chan School of Public Health, this tool helps users validate claims about cancer risk based on research evidence. |
| Alcohol Consumption | The U.S. Surgeon General identifies alcohol as a leading preventable cause of cancer. |
| Coffee and Cancer Risk | Current research suggests coffee consumption may decrease cancer risk. |
| Carcinogenic Foods | Charred, processed, and red meat are flagged as possibly carcinogenic by the International Agency for Research on Cancer. |
| Scented Candles | Burning certain scented candles indoors may lead to exposure to cancer-causing chemicals. |
| Occupational Risks | Pilots and flight attendants face a higher risk for some types of cancer. |
| Turmeric and Cancer Prevention | The effectiveness of turmeric in preventing cancer needs more research. |
| Tampons and Cancer Risk | It’s a myth that using tampons raises cancer risk. |
| Lifestyle Factors | Factors such as low physical activity, obesity, and stress contribute to increased cancer risk. |
| Sleep Disruptions | Disrupted sleep patterns can hinder the body’s ability to fight cancer. |
| Skin Cancer and Sunscreen | Misconceptions about sunscreen use relate to skin cancer risk, especially among people with darker skin. |
| Prostate Cancer in Black Men | Research indicates that Black men are at a higher risk for prostate cancer. |
Summary
Cancer risk is an important topic that requires careful consideration of information sources. With numerous claims in the media, it’s essential to distinguish between verified facts and myths surrounding cancer. Tools like the Cancer FactFinder help individuals navigate these claims, allowing for informed health choices. Understanding the implications of various lifestyle factors is crucial in managing and potentially lowering one’s cancer risk.
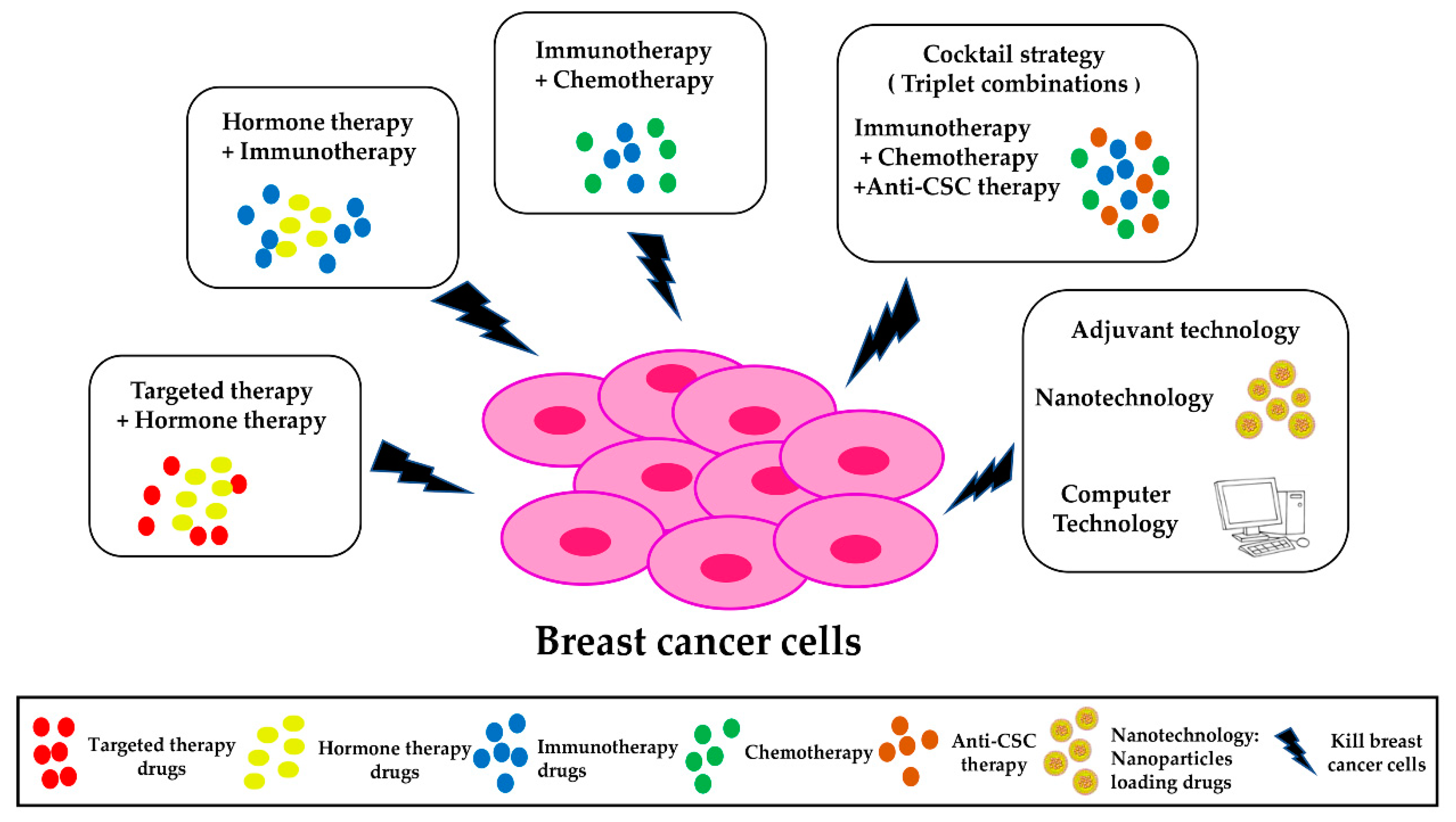
Molecular Therapies for Cancer: A Breakthrough Discovery
Advancements in molecular therapies for cancer are setting the stage for a groundbreaking transformation in how we approach and treat this pervasive disease. Recent research efforts, particularly in the realm of cancer biology, have highlighted the potential of small molecules known as molecular glues, which can cleverly manipulate critical protein interactions within cancer cells. These innovative therapies aim to exploit genetic mutations that underlie various cancers, paving the way for targeted treatment strategies that go beyond traditional methods. With an increased understanding of protein interactions and their role in tumorigenesis, drug discovery is entering a new era, fostering hope for more effective therapies. As scientists delve deeper into cancer research, these molecular approaches may redefine our capabilities in combating cancer’s devastating effects.
Molecular therapies targeting cancer have emerged as a revolutionary frontier in oncology, promising tailored treatments that address the complexities of tumor biology. These targeted strategies utilize small molecules, often termed molecular glues, to enhance or inhibit protein interactions essential for cancer cell survival. By focusing on specific genetic alterations present within tumors, researchers are uncovering novel pathways that could lead to the development of highly effective therapeutic agents. This meticulous approach not only allows for personalized medicine but also opens new avenues in drug discovery by identifying previously overlooked molecular targets. Thus, the intersection of genetic mutation insights and protein interaction dynamics stands to transform the landscape of cancer treatment.
Advancements in Molecular Therapies for Cancer
The recent breakthroughs in molecular therapies for cancer mark a significant leap forward in the fight against this pervasive disease. Researchers at Harvard’s Department of Chemistry and Chemical Biology (CCB) have published compelling studies that delve into the mechanisms of both genetic mutations and small molecules that control cancer cell behavior. By focusing on molecular glues, which facilitate protein interactions that lead to the degradation of oncogenic proteins, these studies pave the way for targeted treatments that could potentially revolutionize cancer therapy.
Understanding and manipulating the complex interactions between proteins within cancer cells are crucial for developing effective therapies. With the advent of molecular glues, scientists now have the tools to create innovative treatments that target previously undruggable proteins. This research not only highlights the potential of molecular therapies for cancer but also underlines the importance of collaboration among various institutions and expertise in advancing drug discovery.
The Role of Molecular Glues in Cancer Treatment
Molecular glues are exciting compounds that can induce interactions between proteins that typically do not bind, effectively transforming how we approach cancer treatment. One notable example is the molecule UM171, which has demonstrated the ability to disrupt the CoREST complex, a key player in gene regulation within cancer cells. This disruption could lead to the selective degradation of oncogenic proteins, thereby halting the uncontrolled proliferation of cancer.
The identification and design of new molecular glues are critical components in the broader scope of cancer research. By understanding the protein interactions facilitated by molecular glues, researchers can devise targeted therapies that are not only effective but also tailored to the specific genetic mutations present in different cancers. This innovative strategy underscores the potential for these compounds to transform the landscape of cancer treatment and contribute significantly to future drug discovery.
Understanding Genetic Mutations and Their Impact
Genetic mutations play a pivotal role in the development and progression of cancer, often altering protein interactions and functions that lead to tumor growth. Recent studies have identified specific mutations in the KBTBD4 protein that contribute to medulloblastoma, a type of pediatric brain cancer. By visualizing these mutations through advanced techniques like cryo-electron microscopy, researchers can gain insights into how these changes affect the protein structure and its interaction with other molecular components.
The convergence of genetic mutations and molecular glues, where they mimic each other’s functional outcomes, is a groundbreaking finding in cancer research. This paradigm shift not only enhances our understanding of disease mechanisms but also opens avenues for the development of targeted therapies that can effectively address the unique molecular profiles of individual cancers.
The Intersection of Drug Discovery and Genetic Insights
The combination of molecular therapies and insights into genetic mutations is reshaping drug discovery processes. By leveraging genetic information to identify potential molecular glues, researchers can create innovative treatments that are tailored to the specific genetic landscape of various cancers. This intersection of molecular therapies and genetic insights signifies a profound advancement in personalized medicine, allowing for more effective and targeted cancer treatments.
Furthermore, understanding how genetic mutations drive cancer progression can inform the design of molecular glues that selectively target these aberrant proteins. This integrated approach not only streamlines drug discovery efforts but also significantly enhances the likelihood of developing successful therapies that improve patient outcomes.
Future Directions in Cancer Research
As research into molecular therapies for cancer continues to evolve, the implications of these studies extend beyond oncology. The methodologies developed in understanding protein interactions and genetic mutations may also be applicable to other diseases, signaling a new direction in biomedical research. For instance, similar approaches could be used to tackle neurodegenerative diseases where protein misfolding plays a crucial role.
Looking ahead, researchers are excited about the potential to discover new molecular glues and identify more genetic mutations that could provide therapeutic targets. By fostering a multidisciplinary approach that combines chemistry, biology, and genomics, the future of cancer research holds promising opportunities for breakthrough therapies that could fundamentally change how we approach numerous diseases.
Collaborative Efforts in Cancer Therapeutics
The pursuit of effective molecular therapies for cancer heavily relies on collaborative efforts among researchers, institutions, and funding bodies. The studies conducted at Harvard, supported by various educational and research institutions, exemplify how shared knowledge and resources can accelerate scientific discovery. Collaboration allows for the pooling of expertise, which is crucial in tackling the multifaceted challenges posed by cancer.
These interdisciplinary partnerships not only enhance the quality of research but also facilitate the translation of findings into clinical practice. By combining insights from different fields, such as chemistry, genetics, and structural biology, researchers can create a more comprehensive understanding of cancer and develop innovative therapeutics that may lead to significant advancements in patient care.
Molecular Strategies for Targeting Undruggable Proteins
One of the most daunting challenges in oncology has been the identification and targeting of so-called ‘undruggable’ proteins. Molecular glues have emerged as a novel strategy to address this issue, as they can enable the degradation of these proteins by inducing favorable interactions with other cellular components. The recent findings surrounding the CoREST complex underscore the potential of molecular glues in targeting proteins that were previously deemed too complex or unstable for therapeutic intervention.
This innovative approach not only broadens the range of potential therapeutic targets but also propels research in drug discovery into new territories. By focusing on the underlying mechanisms of protein interactions facilitated by molecular glues, scientists can design drugs with a higher likelihood of effectiveness, ultimately driving advancements in cancer treatment and improving patient outcomes.
Harnessing Structural Biology for Drug Development
Structural biology plays a crucial role in understanding the molecular underpinnings of diseases, including cancer. By utilizing technologies such as cryo-electron microscopy, researchers can visualize how genetic mutations and molecular glues affect protein structures and interactions. This level of detail is paramount for developing targeted therapies that are informed by precise structural information.
Implementing structural insights into the drug development process allows scientists to create molecules that can effectively modulate protein interactions associated with cancer. By harnessing the information gleaned from structural studies, researchers are better equipped to tackle the complexities of drug discovery and design innovative treatments that can lead to more effective cancer therapies.
The Importance of Personalized Medicine in Cancer Treatment
Personalized medicine represents the future of cancer treatment, focusing on tailoring therapeutic strategies to match the unique genetic profile of each patient’s tumor. The recent advancements in identifying molecular glues and understanding the impact of genetic mutations enhance the ability to create personalized therapies that improve treatment efficacy and minimize side effects. This approach not only holds the promise for better patient outcomes but also addresses the one-size-fits-all dilemma in oncology.
By integrating genetic insights with molecular therapies, clinicians can select the most appropriate treatments based on a patient’s specific cancer characteristics. This tailored strategy is supported by ongoing research efforts aimed at further elucidating the mechanisms of action of molecular glues and their potential applications in various cancer types.
Innovations in Functional Genomics for Cancer Research
Functional genomics is a rapidly advancing field that offers valuable insights into the genetic basis of cancer. By studying how specific genes and their mutations influence cellular behavior, researchers can uncover the underlying mechanisms that drive oncogenesis. The incorporation of functional genomics in cancer research has become particularly important in identifying novel targets for molecular therapies.
The intersection of functional genomics and molecular therapies for cancer opens new avenues for discovery. Researchers can now explore how molecular glues interact with genetic alterations to disrupt cancerous processes, paving the way for innovative treatment strategies that could significantly alter the landscape of cancer therapeutics.
Frequently Asked Questions
What are molecular therapies for cancer and how do molecular glues fit in?
Molecular therapies for cancer involve targeted approaches to treat the disease at a molecular level. Molecular glues are a type of small molecule that facilitate interactions between proteins, promoting the degradation of disease-causing proteins. These glues are crucial in cancer research, as they can be designed to target otherwise undruggable proteins, thereby combating cancer effectively.
How do genetic mutations influence molecular therapies for cancer?
Genetic mutations can significantly affect the efficacy of molecular therapies for cancer by altering protein interactions within cancer cells. For example, mutations in proteins like KBTBD4 can lead to aberrant functions that drive cancer progression. Understanding these mutations helps in tailoring molecular therapies that specifically target altered protein interactions associated with cancer.
What role do protein interactions play in the development of molecular therapies for cancer?
Protein interactions are central to molecular therapies for cancer, as these interactions can dictate the behavior of cancer cells. By deciphering how molecular glues influence these interactions, researchers can develop therapeutic strategies that disrupt unhealthy protein networks, offering pathways to innovate drug discovery aimed at targeted cancer treatments.
What are some of the recent advancements in molecular therapies for cancer research?
Recent advancements in molecular therapies for cancer include the discovery of novel molecular glues and insights into genetic mutations that affect protein interactions. Research led by Harvard scientists has unveiled how small molecules can mimic the effects of genetic mutations to target protein complexes like CoREST, leading to potential new drug development strategies.
How does the concept of ‘chemical genetic convergence’ apply to molecular therapies for cancer?
Chemical genetic convergence refers to the phenomenon where a small molecule, such as a molecular glue, and genetic mutations achieve similar effects on protein interactions and functions. This concept is vital in molecular therapies for cancer, as it suggests that insights gained from studying genetic mutations can inform the design of small molecules for effective cancer treatment.
What are the implications of using molecular glues in drug discovery for cancer treatment?
The implications of using molecular glues in cancer drug discovery are profound. By enabling the targeting of previously undruggable proteins and altering protein interactions, molecular glues provide new avenues for developing effective therapies. This may lead to breakthroughs in treating various types of cancer and advancing the overall landscape of cancer treatment options.
What future directions are researchers pursuing in molecular therapies for cancer?
Researchers are focusing on identifying more instances of genetic mutations that induce beneficial protein interactions to enhance chemical design for molecular therapies. The ongoing study of molecular glues and their interaction with genetic mutations aims to refine targeted treatments and expand the potential applications of molecular therapies beyond cancer.
| Key Points | Details |
|---|---|
| Significant Advancement | The studies represent a leap in understanding and targeting cancer growth at its origin. |
| Molecular Glues | Molecular glues help connect proteins that normally would not interact, enabling cancer-targeting strategies. |
| Specific Research Focus | Research centered on mutations in medulloblastoma and their effects on protein interactions. |
| Collaboration | Research involved contributions from several institutions, enhancing the findings’ credibility. |
| New Insights | Findings provide fresh strategies for drug design by targeting previously ‘undruggable’ proteins. |
| Future Directions | Plans to explore further genetic mutations and their implications for drug discovery. |
Summary
Molecular therapies for cancer are reshaping the landscape of cancer treatment through innovative research that uncovers how to manipulate protein interactions at the molecular level. The advancements made by researchers, especially in understanding the role of molecular glues and genetic mutations, signify a promising future for targeted therapies that can effectively combat aggressive cancers. As studies continue to reveal complex interactions within cancer cells, we move closer to developing more effective and precise cancer therapies.
ACO PC Flex: Revolutionizing Primary Care Payments
ACO PC Flex is an innovative initiative designed to transform the landscape of primary care funding in the United States. As many healthcare experts lament the financial struggles plaguing U.S. primary care, ACO PC Flex emerges as a beacon of hope by introducing a new payment model aimed at enhancing reimbursement rates for physicians. This program leverages the concept of accountable care organizations to incentivize doctors to prioritize preventative measures and holistic patient engagement, ultimately reducing the incidence of costly hospital visits. By adopting a prospective payment approach, ACO PC Flex provides upfront financial support to primary care providers, enabling them to focus on delivering high-quality healthcare rather than merely increasing patient volume. With this strategic shift, specialists and policymakers alike are optimistic that ACO PC Flex will catalyze essential reforms in healthcare reimbursement and contribute to a more sustainable primary care system.
The term ACO PC Flex encapsulates a groundbreaking approach to primary care reimbursement, focusing on a proactive funding model that prioritizes preventative health. Often referred to as the accountable care framework, this initiative redefines how healthcare systems compensate physicians, advocating for a shift from traditional fee-for-service methods to an innovative prospective payment structure. In this evolving landscape, the initiative holds significant promise for improving primary care funding, ultimately seeking to bolster healthcare accessibility and quality. By fostering an environment where primary care providers can spend more time engaging with patients, ACO PC Flex represents a vital step toward addressing the urgent challenges facing the U.S. healthcare system. Supporters believe that this model can serve as a catalyst for broader reforms in healthcare reimbursement, setting the stage for a healthier future.
Understanding the Current Crisis in U.S. Primary Care
The U.S. primary care sector is currently facing a significant crisis, primarily driven by several systemic issues. One major concern is the overwhelming demand for appointments which is not matched by the availability of primary care physicians. Many clinicians are burdened with heavy patient loads and often work under the constraints imposed by larger corporate healthcare entities. These organizations prioritize volume, pushing doctors to rush through appointments to accommodate as many patients as possible, ultimately compromising the quality of care.
Moreover, the financial structures in place seem to favor specialized care significantly over primary care. Physicians in specialties such as cardiology or orthopedics typically have higher reimbursement rates compared to primary care providers. This skewed compensation model leads to a lack of resources for primary care, making it difficult for practitioners to focus on preventive measures that could save costs and improve patient outcomes in the long run. Consequently, if this trend continues, the quality of primary care services may continue to deteriorate, further exacerbating the existing healthcare crisis.
Frequently Asked Questions
What is ACO PC Flex and how does it enhance primary care funding?
ACO PC Flex is a new model within accountable care organizations designed to increase primary care funding significantly. It utilizes a prospective payment system, providing upfront payments to primary care providers before any services are rendered. This innovative approach aims to relieve financial pressures on physicians, foster better patient health management, and encourage investments in primary care infrastructure to prevent serious illnesses and reduce hospital visits.
How does the prospective payment model in ACO PC Flex differ from traditional healthcare reimbursement?
In ACO PC Flex, the prospective payment model allows primary care providers to receive payments in advance based on average costs in their region, in contrast to the traditional fee-for-service model where payments are made after services are delivered. This change is crucial as it enables doctors to focus more on preventative care and patient engagement, rather than just volume-driven care.
What challenges does ACO PC Flex address in the U.S. primary care system?
ACO PC Flex addresses several critical challenges in the U.S. primary care system, including the low reimbursement rates for general practitioners compared to specialists and the overwhelming demand for services. By increasing funding through prospective payments, it aims to create a more sustainable financial environment where primary care practitioners can provide thorough care without excessive pressure to see high patient volumes.
Can ACO PC Flex impact healthcare outcomes for Medicare beneficiaries?
Yes, ACO PC Flex is specifically designed for Medicare recipients and aims to improve healthcare outcomes by providing primary care physicians with the resources they need to prevent hospitalizations. The model encourages investments in comprehensive care, which can lead to better management of chronic conditions and overall patient health.
What is the long-term potential of ACO PC Flex in reshaping primary care reimbursement models?
If successful, ACO PC Flex has the potential to significantly influence primary care reimbursement models across the healthcare system. Its emphasis on prospective payment and preventive care may prompt both Medicare and private insurers to adopt similar frameworks, ultimately leading to better funding for primary care and better health outcomes for patients.
How could ACO PC Flex affect the future of accountable care organizations?
ACO PC Flex could pave the way for a new era in accountable care organizations by proving that prospective payments lead to effective healthcare delivery. If it demonstrates cost savings and improved patient care, other ACO models may adopt similar structures, reshaping the landscape of primary care payment models to better support healthcare providers.
What strategies might ACO PC Flex encourage for improving patient health?
ACO PC Flex encourages strategies focused on preventative care, patient counseling, and the management of chronic illnesses. With stable funding, primary care physicians can dedicate more time to nurturing patient relationships and engaging in non-traditional care activities aimed at promoting long-term health, rather than solely focusing on treatment during office visits.
How does ACO PC Flex relate to the Affordable Care Act’s healthcare reforms?
ACO PC Flex is a direct result of the Affordable Care Act’s push for innovative financing in healthcare. It seeks to increase primary care funding and support the transition towards value-based care, ensuring that primary care practitioners are incentivized to prioritize patient health outcomes over the volume of services provided.
| Key Aspects | Details |
|---|---|
| Current Issues in U.S. Primary Care | Rising demand for appointments, declining number of doctors, and low reimbursement rates for primary care compared to specialists. |
| Prospective Payment Experiment: ACO PC Flex | A new model increasing primary care funding and promoting preventative care, initiated by the Affordable Care Act. |
| Payment Structure Changes | Payments in ACO PC Flex are made upfront (before services), unlike traditional models. This encourages investment in preventative care. |
| Incentives for Improved Care | Doctors encouraged to spend more time on patient counseling and preventative measures rather than just clinic visits. |
| Potential Impact | If successful on Medicare, it could influence funding for Medicaid and private insurers, aiming to improve care accessibility. |
Summary
ACO PC Flex represents a significant innovation in addressing the funding issues plaguing primary care in the United States. Through prospective payment models, this initiative seeks to increase financial support for primary care providers and emphasizes the importance of preventative care. By shifting the payment structure to facilitate upfront funding, ACO PC Flex encourages doctors to engage more deeply with patients’ health needs, aiming to alleviate burdens on the healthcare system. If successful, it has the potential to reshape the landscape of primary care, extending benefits to both Medicare and potentially influencing broader insurance frameworks.
Citrus Depression: How Oranges Lower Your Risk by 20%
Citrus depression is an emerging area of research that highlights the intriguing connection between diet and mental health. Recent studies suggest that consuming citrus fruits may significantly lower the risk of depression, providing a natural method for depression prevention. The gut-brain connection plays a pivotal role in this phenomenon, as citrus fruits enhance the growth of beneficial gut bacteria, which in turn affects the production of mood-elevating neurotransmitters. Incorporating citrus into your diet not only offers delicious health benefits but may also serve as a proactive approach to improving mental well-being. As we delve into the mechanics behind this relationship, it becomes clearer how what we eat impacts our mood and overall mental health.
Exploring the concept of citrus depression reveals a fascinating aspect of how our dietary choices influence emotional wellness. Known as the citrus impact on mood enhancement, this topic encompasses the physiological relationship between our food intake and mental health outcomes. The phenomenon is tied to the gut-brain nexus, wherein the consumption of citrus fruits contributes to the betterment of gut health, thereby fostering a more robust mental state. With an emphasis on the advantages of citrus in combatting feelings of sadness or anxiety, this discussion opens doors to further understanding of how diet and mood intertwine. Such insights underline the importance of nutrition in maintaining a balanced emotional state and preventing depressive symptoms.
The Connection Between Citrus Intake and Mental Health
Recent research emphasizes the vital link between diet and mental health, particularly highlighting how citrus fruits can improve mood and potentially lower depression risk. Studies have shown that consuming just one medium orange a day can result in a significant 20% reduction in the likelihood of developing depression. This intriguing finding stems from an extensive analysis of data collected from the Nurses’ Health Study II, which involved over 100,000 female participants. The study points to the unique potential of citrus fruits, setting them apart from other fruits and vegetables, which do not exhibit the same relationship with mental health.
The health benefits of citrus fruits can be credited to their ability to promote the growth of beneficial gut bacteria, such as Faecalibacterium prausnitzii (F. prausnitzii). This specific strain has been associated with improved mental health outcomes, as it contributes to the production of neurotransmitters like serotonin and dopamine. These neurotransmitters, known for their roles in mood regulation, are impacted by gut health, reinforcing the gut-brain connection. Consumers are being encouraged to incorporate more citrus fruits into their diets as a simple yet effective strategy for enhancing mental well-being and decreasing the risk of depression.
Understanding the Gut-Brain Connection Through Diet
The gut-brain connection has gained considerable attention in recent years, as researchers uncover the significant role gut microbiota play in influencing mood and mental health. The consumption of citrus fruits not only supports the growth of beneficial bacteria but also affects the neurochemical environment within the body. This correlation is essential, as the balance of neurotransmitters is crucial for emotional stability and overall mental wellness. By establishing a healthy gut microbiome through a citrus-rich diet, individuals may reinforce their defenses against depression.
Specifically, Faecalibacterium prausnitzii is believed to act through metabolic pathways that regulate serotonin and dopamine levels. This relationship illustrates a two-way street: while a healthy diet can improve gut bacteria, a healthy gut can, in turn, enhance mood and cognitive function. Such understanding may pave the way for innovative dietary interventions aimed at preventing depression, shifting the focus from traditional medication to natural food-based strategies that support mental health.
Unlocking the secrets of the gut-brain connection provides valuable insights into how lifestyle choices impact mental health. By being conscious of the foods we consume, particularly citrus fruits, we can make strides in depression prevention and overall emotional well-being. Individuals are encouraged to explore the beneficial properties of various dietary options, embracing a holistic approach to mental health that extends beyond conventional treatments.
The Role of Citrus Fruits in Depression Prevention
Citrus fruits are emerging as essential partners in the quest for effective depression prevention strategies. As ongoing research sheds light on their benefits, the notion that dietary choices can significantly influence mood gains traction. The inclusion of citrus in one’s daily meals may not only contribute to a healthier diet but could also reduce the risk of depressive symptoms. This potential for prevention underscores the importance of considering food as a frontline defense in mental health care.
Engaging in preventive measures through diet could alleviate the burden on healthcare systems and provide individuals with more autonomy over their mental health. Eating citrus regularly—an easy addition to most diets—could empower people to take proactive steps toward enhancing their psychological resilience. As we delve deeper into understanding how certain foods interact with our biology, citrus fruits could stand out as a remarkable tool in maintaining mental wellness.
Exploring Citrus Fruits’ Neurochemical Benefits
The neurochemical benefits of citrus consumption are becoming increasingly apparent in research focusing on food and mood. The consumption of citrus fruits has been linked to the production of vital neurotransmitters that play a crucial role in regulating our emotions. By influencing serotonin and dopamine synthesis, citrus not only promotes happiness but may also serve as a natural adjunct to more conventional mental health treatments. This burgeoning interest in dietary neuroscience reveals new depths to the age-old adage of ‘you are what you eat,’ emphasizing the profound effect of nutrition on emotional health.
This research highlights the possibility of leveraging the gut-brain connection for therapeutic purposes. By understanding the pathways through which citrus influences mental states, healthcare providers can refine approaches to intervention in depression management. Ultimately, as we grapple with the complexities of mental health, harnessing the neurochemical benefits of citrus fruits may provide a straightforward, effective adjunct to existing treatment modalities for depression, underscoring the important role of diet in mental well-being.
Future Directions in Citrus Research
Going forward, the exploration of citrus fruits as a viable means of depression prevention is a promising direction in nutritional psychiatry. Much more needs to be uncovered about the specific mechanisms through which citrus affects mood. Future studies aim to investigate how various forms of citrus and their components interact with different gut bacteria, including F. prausnitzii, to further elucidate the relationship between diet and mental health outcomes. This landscape of research is vital, particularly in the context of the rising prevalence of depression and the search for non-pharmaceutical interventions that are effective and have minimal side effects.
As researchers forge ahead, there is hope that clinical trials will validate the findings linking citrus consumption with improved mental health. The goal would be to enhance existing mental health strategies with dietary interventions that reinforce long-term resilience against mood disorders. By integrating dietary approaches with established mental health practices, a comprehensive strategy may emerge that could revolutionize how we view and treat depression.
Integrating Citrus into a Holistic Mental Health Approach
Adopting a holistic approach to mental health encompasses not just medication but also lifestyle changes that prioritize nutrition. The seamless integration of citrus fruits into daily diets can serve as a transformative step towards achieving balanced mental wellness. This way of thinking encourages individuals to treat their bodies as systems where dietary choices significantly influence emotional states. The bright, natural sugars and high vitamin C content in citrus can elevate spirits while optimizing gut health, reinforcing the mind-body connection.
Encouraging adequate consumption of citrus fruits can empower individuals to take charge of their mental health. As part of a broader strategy that may also include physical activity, mindfulness practices, and social connections, citrus emerges as an accessible tool for enhancing well-being. Promoting awareness about the mental health benefits of diet incorporates multiple perspectives on health, potentially leading to improved outcomes for many who struggle with mental health issues.
The Impact of Comfort Foods on Mental Wellness
Comfort foods have long been associated with emotional relief, yet the phenomenon requires deeper exploration, particularly as it pertains to mental wellness. Citrus fruits can easily fall into the comfort food category while also providing biochemical benefits that positively impact mood. Unlike traditional comfort foods that may be high in sugar or unhealthy fats, citrus offers a healthier option that nourishes the body while elevating the spirit. The notion that comfort foods can influence emotional well-being signifies an evolving understanding of how diet intersects with mental health.
When individuals reach for their favorite snacks in moments of stress, having a healthy choice available may facilitate better mental health outcomes. Thus, introducing citrus as a staple in comfort foods could act as a bridge to healthier eating habits. As society becomes increasingly aware of how nutritional choices can fortify mental health, citrus fruits can play a pivotal role in redefining what comfort foods mean in the context of wellness.
Citrus Fruits: A Potential Game-Changer for Emotional Health
The exciting prospects surrounding citrus fruits as a game-changer in emotional health reflect an evolving dialogue about the relationship between our diets and well-being. As outlined in research findings, the capacity of citrus fruits to reduce the risk of depression has implications that extend to all areas of mental health. By positioning citrus as a mainstay of dietary recommendations for emotional well-being, we may empower individuals with straightforward actions they can take to enhance their mental health.
This pivotal role of citrus in emotional health reinforces the importance of focusing on prevention rather than merely treating existing conditions. Cultivating a mindset that values food choices as integral to maintaining mental wellness could revolutionize our approach to mental health care. As more studies unveil the depths of the benefits associated with citrus consumption, we can anticipate a future in which these vibrant fruits are widely recognized not just for their nutritional value, but also for their profound impact on emotional health and resilience.
Frequently Asked Questions
What is the link between citrus depression and mental health?
Citrus depression refers to the potential impact of citrus fruits on reducing the risk of depression. Recent studies suggest that consuming citrus fruits, such as oranges, may lower depression risk by approximately 20%. This is believed to be due to the stimulation of beneficial gut bacteria, which influence mood-related neurotransmitters such as serotonin and dopamine, thus linking citrus intake with improved mental health.
How do citrus fruits benefits contribute to depression prevention?
Citrus fruits offer multiple benefits that may contribute to depression prevention. They are rich in vitamins, antioxidants, and fibers, which can enhance gut health. A healthy gut microbiome, influenced by citrus consumption, promotes the growth of beneficial bacteria like Faecalibacterium prausnitzii. This bacterium is linked to the production of mood-regulating neurotransmitters, suggesting that including citrus in your diet may help mitigate depressive symptoms.
What role does the gut-brain connection play in citrus depression?
The gut-brain connection is a crucial factor in understanding citrus depression. Research indicates that citrus fruits can positively impact gut health by fostering beneficial bacteria. These bacteria, particularly Faecalibacterium prausnitzii, are linked to the production of neurotransmitters such as serotonin and dopamine in the gut, which can travel to the brain and influence mood, potentially lowering the risk of depression.
Can diet and mood be influenced by citrus intake?
Yes, diet and mood can be influenced by citrus intake. Incorporating citrus fruits like oranges into your daily diet may support mental health by enhancing gut microbiota and increasing levels of neurotransmitters that elevate mood. This dietary approach could serve as a complementary strategy in depression prevention, highlighting the importance of nutritional choices on mental well-being.
Is eating citrus as effective as traditional antidepressants in treating depression?
While eating citrus can contribute to depression prevention, it is not directly comparable to traditional antidepressants, which are used to treat existing depression. Current studies suggest that citrus can lower the risk of developing depression; however, further research is needed to evaluate its effectiveness in alleviating depression when used alongside conventional therapies. Diet can play a supportive role in mental health management.
What are the potential side effects of eating citrus for mental health benefits?
Eating citrus fruits is generally considered safe with minimal side effects. Unlike pharmaceutical treatments for depression, which can have significant side effects, citrus consumption poses no major health risks. However, individuals should consume them in moderation as part of a balanced diet to fully reap their mental health benefits while avoiding any dietary excesses.
| Key Point | Details |
|---|---|
| Study Finding | Eating one medium orange a day may reduce depression risk by 20%. |
| Research Background | The study was conducted by Raaj Mehta using data from the Nurses’ Health Study II involving over 100,000 women. |
| Specific Effects | The benefits appear specific to citrus, as other fruits do not show the same relationship with depression. |
| Gut-Bacteria Link | Citrus may stimulate the growth of F. prausnitzii which influences serotonin and dopamine production. |
| Future Research | More studies, including clinical trials, are needed to explore the impact of citrus on depression treatment. |
Summary
Citrus depression is a topic of growing interest in the field of mental health, as recent studies suggest that consuming citrus fruits, particularly oranges, may significantly lower the risk of depression. The findings indicate a 20% reduction in depression risk associated with daily orange consumption, primarily due to its impact on gut bacteria like F. prausnitzii, which helps produce mood-enhancing neurotransmitters. As research continues to unveil the connections between diet and mental well-being, incorporating citrus into one’s daily routine could serve as a simple yet effective strategy for improving mental health.
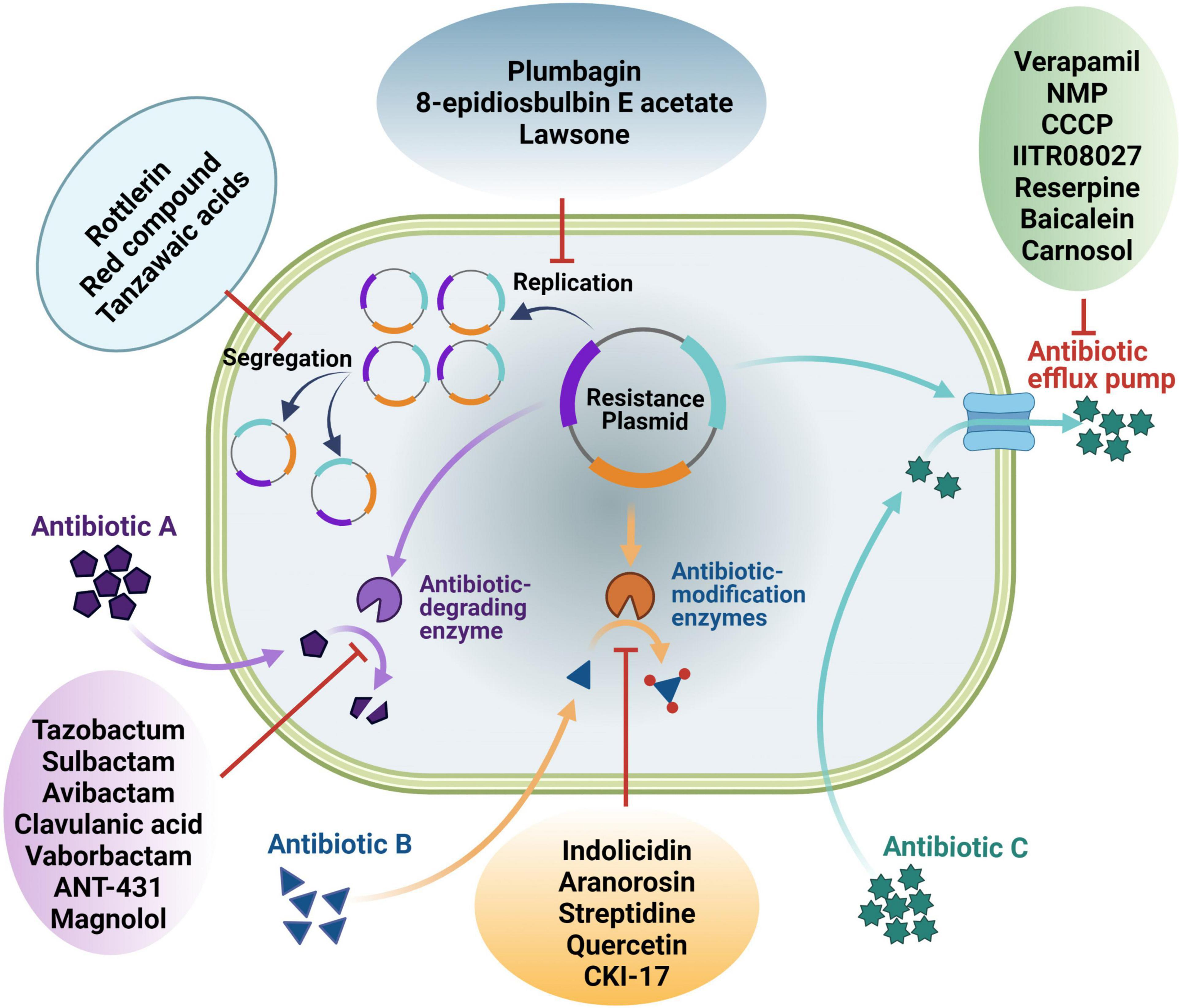
New Antibiotics for Drug-Resistant Bacteria: A Promising Venture
In the battle against drug-resistant bacteria, the development of new antibiotics for drug-resistant bacteria emerges as a beacon of hope. As antibiotic resistance continues to escalate, threatening global health by complicating the treatment of drug-resistant infections, innovative solutions are urgently needed. Companies like Kinvard Bio are paving the way for antibiotic discovery, focusing on unique strategies such as bacterial ribosome targeting. The promise of their new class of antibiotics could significantly alter the landscape of antibiotic resistance, providing much-needed alternatives to traditional treatments. As our understanding of these resilient pathogens deepens, breakthroughs in antibiotic innovation are not just beneficial—they’re essential for safeguarding future generations.
Tackling the growing crisis of antibiotic resistance requires a multifaceted approach, and the emergence of novel antimicrobial agents offers a fresh perspective. The increasing prevalence of infections resistant to standard treatments has created a dire need for effective solutions in combating these formidable pathogens. Innovations from startups like Kinvard Bio, which focus on antibiotic innovation and targeting critical elements of bacterial function, highlight the importance of renewed efforts in antibiotic research. As healthcare professionals and scientists strive to outpace the relentless evolution of bacteria, the development of new therapeutic options is crucial for managing the rise of drug-resistant diseases. A proactive stance on antibiotic discovery not only enhances treatment efficacy but also preserves the viability of existing medication regimens.
The Urgency of Addressing Antibiotic Resistance
Antibiotic resistance has become a monumental challenge in modern medicine, leading to an increase in drug-resistant infections that impact millions globally. A report from the World Health Organization highlights that over one million deaths were attributed to antibiotic resistance in 2019 alone. This alarming statistic underscores the urgency of fostering new solutions to combat bacteria that no longer respond to standard treatments. As traditional antibiotics lose their efficacy, patients are facing longer hospital stays, higher medical costs, and increased mortality rates, thereby creating a dire need for innovations in antimicrobial therapies.
In this context, research and development efforts must shift towards sustainable antibiotic solutions that can effectively target resistant pathogens. The majority of antibiotics in existing use were developed decades ago, and very few new classes have been introduced to the market. Current projections indicate that if antibiotic resistance continues at this pace, common surgical procedures and cancer treatments could become life-threatening due to the risk of infection. Consequently, it is imperative to recognize not just the scale of this crisis, but also the innovative strategies in antibiotic discovery that might offer hope against resistant bacterial strains.
Frequently Asked Questions
What are the innovative features of new antibiotics for drug-resistant bacteria?
New antibiotics for drug-resistant bacteria, such as those developed by Kinvard Bio, feature unique structural characteristics that allow them to bind more effectively to bacterial ribosomes. This preorganized binding enhances their ability to combat antibiotic resistance, making them potentially more effective against a wider range of drug-resistant infections.
How do new antibiotics address the issue of antibiotic resistance?
New antibiotics for drug-resistant bacteria target essential components like the bacterial ribosome in innovative ways that differ from traditional antibiotics. By developing compounds like oxepanoprolinamides, researchers aim to evade existing resistance mechanisms, thereby providing fresh options in the fight against antibiotic-resistant infections.
Why is antibiotic discovery crucial for combating drug-resistant infections?
Antibiotic discovery is essential to combat drug-resistant infections as the effectiveness of existing antibiotics diminishes due to bacterial resistance. With reports indicating millions of deaths from antibiotic resistance, new classes of antibiotics are vital for ensuring that healthcare providers have effective treatments available for stubborn bacterial infections.
What role do Kinvard Bio’s new antibiotics play in treating complicated infections?
Kinvard Bio’s new antibiotics are specifically designed to treat complicated infections, such as bacterial pneumonia and urinary tract infections. Their development focuses on meeting high unmet patient needs by demonstrating efficacy against pathogens that show resistance to current treatment options.
What is the significance of targeting the bacterial ribosome in antibiotic development?
Targeting the bacterial ribosome is significant because it remains a highly validated approach in antibiotic development. The unique binding methods employed by Kinvard Bio’s antibiotics allow for effective treatment against various pathogens, offering hope for addressing the pressing challenges posed by antibiotic-resistant bacteria.
How does Kinvard Bio plan to deliver its new antibiotics effectively?
Kinvard Bio aims to develop both intravenous and oral delivery methods for their new antibiotics, which is crucial in reducing hospital admissions and lengths of stay. This dual delivery approach is intended to enhance patient access to effective treatments for drug-resistant infections.
What challenges does antibiotic resistance pose in modern medicine?
Antibiotic resistance presents significant challenges in modern medicine, leading to increased morbidity and mortality rates. With only a limited number of new antibiotics being approved, the risk of inadequate treatment options against drug-resistant infections continues to grow, necessitating urgent innovation in antibiotic discovery.
How long have researchers at Harvard been working on new antibiotics?
Researchers at Harvard, specifically in the Myers Lab, have been working on developing new antibiotics for over a decade. Their ongoing research aims to create effective treatments for drug-resistant bacteria, with historical roots tracing back to the 1960s when early antibiotics were first explored.
What support has Kinvard Bio received for its antibiotic development?
Kinvard Bio has received considerable support from various organizations, including a $1.2 million grant from CARB-X and additional funding from the Blavatnik Biomedical Accelerator. Such backing facilitates the ongoing research and development of their promising new antibiotics targeting drug-resistant infections.
What is the future outlook for antibiotic resistance and new antibiotic innovation?
The future outlook for antibiotic resistance is critical, but companies like Kinvard Bio are poised to make significant contributions through innovative antibiotic research. Continuous progress in antibiotic discovery is imperative to ensure effective treatments are available for future generations facing drug-resistant infections.
| Key Points | Details |
|---|---|
| Launch of Kinvard Bio | A biotech startup from Harvard focusing on new antibiotics targeting drug-resistant infections. |
| Antibiotic Resistance Crisis | Over 1 million deaths in 2019 due to antibiotic resistance; fewer new antibiotics approved. |
| Kinvard’s Innovative Approach | Developing oxepanoprolinamides that uniquely bind to the bacterial ribosome, crucial for fighting resistance. |
| Historical Context | Antibiotic discovery dates back to the 1940s with penicillin; newer classes are urgently needed due to resistance. |
| Funding and Support | Receives funding from CARB-X and Harvard’s Blavatnik Biomedical Accelerator to advance research. |
| Research Goals | Targeting infections like pneumonia and urinary tract infections with a pipeline for urgent medical needs. |
Summary
New antibiotics for drug-resistant bacteria are crucial in addressing the escalating health crisis posed by antibiotic resistance. With millions affected and limited treatment options available, the launch of Kinvard Bio represents a beacon of hope in the fight against these formidable pathogens. By developing innovative antibiotics that harness unique binding mechanisms to target the bacterial ribosome, Kinvard Bio stands at the forefront of a new era in antibiotic research. Continued investment and innovation in this field are essential to ensure effective treatments for the next generation.
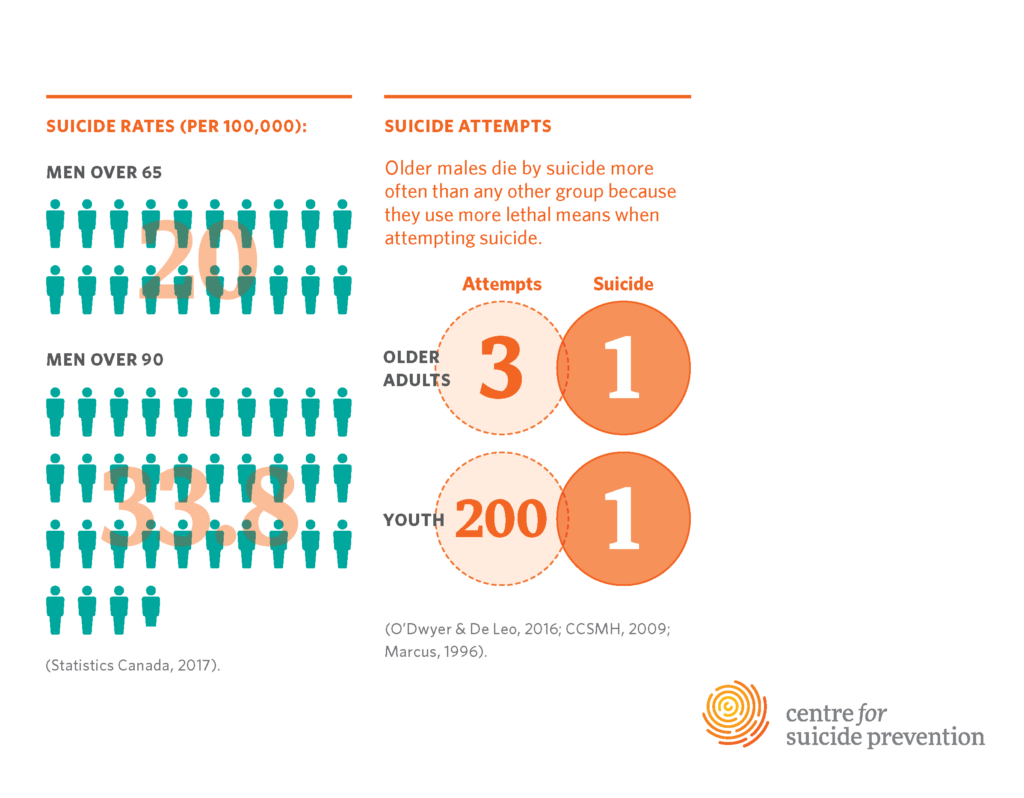
Suicide Prevention for Older Adults: A Critical Need
Suicide prevention for older adults is an urgent public health concern, especially given that individuals aged 75 and older face the highest rates of suicide compared to any other age group. Despite this alarming statistic, the available mental health resources specifically targeting the aging population remain insufficient. A recent study highlighted a significant gap in online suicide prevention efforts directed at older adults, emphasizing the need for geriatric psychiatry professionals to develop tailored strategies. The increasing prevalence of elderly suicide rates calls for immediate action, encouraging both healthcare providers and organizations to enhance their outreach and support mechanisms. By improving access to relevant information and resources, we can foster a safer environment for older adults seeking help at a time when they need it most.
Addressing the challenges of preventing suicide among senior citizens involves understanding the complex factors affecting their mental well-being. As the demographic landscape shifts with a growing elderly population, it becomes imperative to implement effective strategies to safeguard their mental health. Resources designed for online suicide intervention are critical for reaching older individuals who may feel isolated or hopeless. Ensuring that targeted programs in geriatric psychiatry are available can significantly reduce the risks associated with elderly suicide rates. By creating supportive environments and enhancing access to mental health resources, society can take meaningful steps towards preserving the lives of our seniors.
Understanding the Rise of Elderly Suicide Rates
Suicide rates among older adults, particularly those aged 75 and over, are alarming and have been on the rise in the United States. According to the Centers for Disease Control and Prevention (CDC), this demographic reports a suicide rate of 20.3 per 100,000 individuals, making them the age group with the highest incidence of suicide. This trend raises serious concerns regarding mental health resources available to the aging population, as traditional interventions often do not meet the unique needs of older individuals.
Factors contributing to these increasing suicide rates among seniors include social isolation, loneliness, and a lack of tailored mental health services that are accessible to them. Many older adults may feel disconnected from society, leading to a decline in mental health that can precipitate suicidal thoughts. Additionally, systemic biases within healthcare research often overlook the specific challenges faced by this age group, resulting in a gap in effective geriatric psychiatry interventions.
The Need for Targeted Suicide Prevention for Older Adults
The findings from recent studies indicate that there is a significant imbalance in the focus of online suicide prevention initiatives, which often target younger demographics while neglecting the pressing needs of the elderly. Despite acknowledging the high risk of suicide among older populations, many well-known organizations fail to provide easily accessible resources specifically designed for this age group. This lack of tailored programming highlights an urgent need for suicide prevention strategies that are attuned to the characteristics and healthcare challenges faced by older adults.
To address these disparities, more targeted campaigns should be launched that cater explicitly to older adults, providing them with the mental health resources they require. Such initiatives could include online platforms that offer easy navigation, support groups, and personalized communication methods catered to the preferences of the aging population. By bridging the gap in online suicide prevention efforts, we can ensure that older adults receive timely and appropriate support to mitigate their risk of suicide.
Barriers to Accessing Mental Health Resources
One of the primary barriers older adults face in accessing mental health resources is the lack of geriatric-specific information accessible through online channels. As noted in the research led by the Technology and Aging Laboratory at McLean Hospital, many older adults are increasingly turning to the internet for health information. However, when they search for suicide prevention resources, they often find few meaningful results that cater to their specific needs. This can create feelings of frustration and hopelessness.
Even when older adults are aware of their mental health struggles, they may encounter difficulties in navigating the digital landscape. Many websites fail to present information in an easily digestible format, which can deter seniors from seeking help. Therefore, it is vital for mental health organizations to revamp their online resources, ensuring they are user-friendly and include materials that resonate with the geriatric population.
Collaboration for Improved Online Suicide Prevention
Collaboration between mental health professionals, researchers, and organizations is crucial to enhance online suicide prevention efforts for older adults. Partnerships can help facilitate the development of resources that address the unique challenges faced by this demographic. By taking a collective approach to research and resource distribution, mental health providers can create a more supportive environment for older adults seeking help.
Furthermore, public awareness campaigns that specifically focus on older adults can be significant in changing perceptions about mental health within this community. Targeted outreach can encourage seniors to engage with mental health services and highlight the importance of seeking help when needed. This collaborative effort could ultimately lead to reduced suicide rates and improved mental well-being among older individuals.
Innovations in Geriatric Psychiatry
Geriatric psychiatry plays a crucial role in addressing the mental health needs of older adults, especially concerning suicide prevention. Innovations in this field are necessary to develop effective interventions that can resonate with the aging population. Approaching mental health care from a geriatric lens involves understanding the unique life experiences of older individuals and tailoring therapies that consider these factors.
Additionally, advancements in technology can also support innovations in geriatric psychiatry. For example, teletherapy and other online mental health resources can create greater accessibility for older adults who may have mobility issues or difficulties accessing traditional mental health services. Implementing these innovations could ensure that elderly individuals receive the mental health care they need promptly.
Psychosocial Factors Influencing Elderly Suicide
The psychosocial factors affecting older adults are diverse and complex, significantly influencing their mental health and suicide risk. Issues such as the death of a spouse, chronic pain, and family disconnection can compound feelings of despair and isolation. Understanding these factors is essential for developing effective suicide prevention strategies tailored to older adults.
Additionally, the impact of mental health stigma may prevent older adults from seeking help. Many within this generation were not exposed to discussions surrounding mental health, leading them to feel ashamed of their struggles. Mental health resources must not only provide support but also work to destigmatize the conversation around mental health among older adults, encouraging them to seek the help they deserve.
Importance of Community Support
Community support is a critical component of suicide prevention for older adults. Programs that encourage social engagement, such as senior centers or community activities, can alleviate feelings of loneliness and isolation that often lead to suicidal thoughts. By fostering connections among older individuals, these programs create a support network that can enhance mental well-being.
Moreover, involving family members in discussions around mental health can strengthen these initiatives. Education on recognizing signs of distress in older relatives can empower families to provide the support needed during challenging times. Community-based approaches that emphasize relationship-building can significantly mitigate the risk of suicide among elderly populations.
Role of Technology in Suicide Prevention
In today’s digital age, technology can play a significant role in suicide prevention for older adults. With the increasing comfort of this demographic in using the internet, there is immense potential for innovative online platforms that provide mental health resources tailored to their needs. These platforms can offer educational content, support groups, and easily accessible crisis intervention services.
Moreover, technology such as mobile applications can remind older adults to engage in positive activities, connect with friends, or even check in with mental health professionals. By integrating technology into suicide prevention efforts, we can create a more responsive and accessible mental health landscape that supports the needs of aging populations.
Advocating for Increased Funding in Geriatric Mental Health
Increased funding for geriatric mental health services is vital for addressing the rising suicide rates among older adults. Without adequate financial support, initiatives designed to tackle the unique challenges facing this population cannot be fully developed or implemented. This funding is essential for research that focuses specifically on late-life mental health issues and the effectiveness of various interventions.
Advocacy efforts must highlight the importance of allocating resources to geriatric mental health, ensuring that older adults have access to the services they need. By bringing attention to this critical issue, stakeholders can help secure the funding necessary for meaningful suicide prevention strategies that can save lives.
Frequently Asked Questions
What are effective suicide prevention strategies for older adults?
Effective suicide prevention strategies for older adults include increasing access to mental health resources tailored specifically for this aging population, promoting awareness about geriatric psychiatry, and encouraging social engagements to reduce isolation. Programs focusing on mental health education and support networks can also aid in reducing elderly suicide rates.
How can online suicide prevention resources be improved for older adults?
Online suicide prevention resources can be improved for older adults by making them more accessible and user-friendly. This includes using larger text for easy reading, providing straightforward navigation, and specifically targeting information related to the unique challenges older adults face in mental health, thereby reducing barriers to accessing critical support.
Why are older adults at higher risk for suicide?
Older adults are at higher risk for suicide due to factors like loneliness, social isolation, chronic health issues, and mental health conditions. The aging population faces unique challenges that often require specialized geriatric psychiatry interventions, yet they frequently encounter a lack of targeted mental health resources.
What role does social isolation play in elderly suicide rates?
Social isolation significantly contributes to increased elderly suicide rates as it can lead to feelings of loneliness and despair. Engaging older adults in community activities, fostering relationships, and providing mental health resources can mitigate these feelings and promote better mental health outcomes.
How does geriatric psychiatry contribute to suicide prevention in older adults?
Geriatric psychiatry plays a critical role in suicide prevention for older adults by providing specialized knowledge about mental health issues affecting this demographic. This includes assessing risk factors, tailoring therapeutic interventions, and advocating for mental health resources that meet the needs of this aging population.
What types of mental health resources are available for older adults at risk for suicide?
Mental health resources available for older adults at risk for suicide include counseling services, support groups, crisis intervention hotlines, and mental health education programs. It’s essential to ensure that these resources are tailored to address the specific needs and concerns of the aging population.
How can family members support older adults in suicide prevention?
Family members can support older adults in suicide prevention by maintaining open lines of communication, encouraging them to seek mental health resources, and fostering social connections. Being attentive to changes in mood or behavior can also help family members identify when additional support may be needed.
Why is there a need for more research on late-life suicide prevention?
There is a pressing need for more research on late-life suicide prevention due to the increasing rates of suicide among older adults and the underrepresentation of this population in mental health studies. Enhanced research efforts can lead to improved interventions and more effective mental health resources tailored to the needs of older adults.
| Key Point | Details |
|---|---|
| High Suicide Rates | Adults aged 75 and older have the highest suicide rates at 20.3 per 100,000 according to the CDC. |
| Lack of Resources | Study shows national suicide prevention organizations provide few resources for older adults. |
| Internet Usage | Older adults increasingly use the internet to seek health information but struggle to find targeted resources. |
| Imbalance in Targeting | Most suicide prevention campaigns do not focus on the unique needs of older adults. |
| Need for Tailored Campaigns | Research emphasizes the need for campaigns that cater to older adults’ healthcare and social needs. |
Summary
Suicide prevention for older adults is an urgent and critical issue, as this demographic experiences the highest rates of suicide yet has limited access to necessary resources. The study conducted by researchers at McLean Hospital reveals a significant gap in suicide prevention efforts tailored for seniors, highlighting the need for targeted campaigns addressing their unique needs. Increasing awareness and accessibility of these resources is essential to mitigate the rising suicide rates among older populations, particularly as issues like loneliness and social isolation contribute to their vulnerability. By focusing on creating more inclusive and age-appropriate prevention strategies, we can better support the mental health of older adults.