
AI Tool in Pediatric Cancer Recurrence: A New Hope
The emergence of an innovative AI tool in pediatric cancer recurrence has transformed the landscape of relapse risk assessment among young patients, particularly those battling brain tumors such as pediatric gliomas. Recent studies highlight the impressive capabilities of AI cancer prediction systems, which leverage machine learning to analyze MRI scans over time, offering a more accurate evaluation of recurrence risks compared to traditional methods. This breakthrough technology not only eases the burden of frequent imaging on children and their families but also enhances the precision of medical insights into their conditions. By implementing advanced temporal learning in medicine, researchers at leading institutions are redefining how pediatric cancer monitoring and treatment protocols are approached. The results demonstrate a significant shift towards improved patient outcomes, marking a pivotal moment in the fight against pediatric cancer.
In recent years, advanced artificial intelligence tools have begun to play a crucial role in monitoring the risk of relapses in pediatric oncology, particularly for conditions like brain tumors. These intelligent systems utilize complex algorithms to analyze sequential MRI images, facilitating a deeper understanding of pediatric gliomas and their recurrence patterns. Through sophisticated methods that emphasize the temporal aspects of medical imaging, healthcare providers can better assess the long-term risks that young patients may face. This progressive approach not only reduces the frequency of stressful imaging sessions but also provides actionable insights for tailored treatment plans. With ongoing research and development, we are at the forefront of a new era in healthcare that promises enhanced support and outcomes for children battling cancer.
The Breakthrough of AI in Pediatric Cancer Recurrence Prediction
Recent advancements in artificial intelligence (AI) have significantly changed the landscape of pediatric cancer care, especially in predicting the recurrence of brain tumors such as pediatric gliomas. Traditional methods relied heavily on individual MRI scans, which often lacked the predictive power necessary to effectively gauge the risk of relapse. However, a groundbreaking study conducted by researchers at Mass General Brigham has demonstrated that an AI tool trained to analyze multiple brain scans can predict relapse risk with remarkable accuracy, surpassing conventional techniques. This innovation is expected to enhance decision-making processes and treatment strategies for pediatric patients.
In the study, researchers utilized a technique known as temporal learning, which enables the AI model to synthesize findings from a series of MRI scans taken over time. By capturing subtle changes in tumor characteristics across these scans, the AI can more effectively discern patterns that indicate potential recurrence. This method not only improves the reliability of predictions but also lessens the reliance on frequent imaging, which can be distressing for children enduring long-term cancer treatment.
Frequently Asked Questions
How does the AI tool in pediatric cancer recurrence enhance MRI scans pediatric cancer assessment?
The AI tool in pediatric cancer recurrence specializes in analyzing multiple MRI scans over time, and it employs a technique called temporal learning. This method enables the AI to synthesize data from various scans, allowing for a more accurate assessment of recurrence risk in pediatric cancer patients, particularly those with gliomas.
What is the role of AI cancer prediction in managing pediatric gliomas?
AI cancer prediction plays a crucial role in managing pediatric gliomas by providing accurate risk assessments of cancer recurrence. The AI tool utilizes temporal learning to analyze sequential MRI scans, enabling healthcare providers to identify patients at higher risk of relapse and tailor treatments accordingly.
Why is temporal learning important for AI tools in pediatric cancer recurrence risk assessment?
Temporal learning is vital for AI tools in pediatric cancer recurrence risk assessment as it trains models to understand changes across multiple brain scans over time. This approach results in improved predictions of relapse, significantly outperforming traditional methods that rely on single images.
Can the AI tool in pediatric cancer recurrence reduce the stress of frequent MRI scans for children?
Yes, the AI tool has the potential to reduce the frequency of MRI scans for pediatric cancer patients deemed at low risk for recurrence. By accurately predicting which patients may not need frequent imaging, it alleviates the stress and burden associated with regular follow-ups for children and their families.
What accuracy did the AI tool achieve in predicting pediatric glioma recurrence?
The AI tool achieved an impressive accuracy rate of 75-89% in predicting the recurrence of low- or high-grade pediatric gliomas within one year post-treatment, a substantial improvement over traditional prediction methods that have an accuracy of only about 50%.
How is the AI tool in pediatric cancer recurrence validated for clinical use?
The AI tool is currently undergoing further validation to ensure its effectiveness in diverse clinical settings. Researchers plan to conduct clinical trials to determine if AI-informed predictions of recurrence can lead to improved care strategies for pediatric patients.
What are the future implications of using AI tools in pediatric cancer recurrence?
The future implications of using AI tools in pediatric cancer recurrence include better individualized treatment plans, reduced healthcare burden through fewer imaging requirements for low-risk patients, and enhanced early intervention strategies for high-risk cases, improving overall patient care.
How does the study contribute to understanding pediatric gliomas and their recurrence risks?
The study contributes to understanding pediatric gliomas by demonstrating how advanced AI tools can leverage temporal learning from MRI scans, ultimately improving the prediction of recurrence risks. This research provides a foundation for developing better management strategies for pediatric cancer patients.
Why is early detection crucial in pediatric cancer recurrence, specifically for gliomas?
Early detection of recurrence in pediatric gliomas is crucial because timely intervention can significantly improve treatment outcomes. By employing AI tools that predict relapse risks accurately, clinicians can initiate appropriate therapies sooner, potentially preventing serious health complications for young patients.
What impact could AI tools in pediatric cancer recurrence have on healthcare practices?
AI tools in pediatric cancer recurrence could revolutionize healthcare practices by enabling more precise, data-driven decisions, optimizing follow-up protocols, and enhancing the overall efficiency of pediatric oncology care, resulting in better outcomes and patient experiences.
| Key Point | Details |
|---|---|
| AI Tool Utilization | AI tool developed to analyze multiple MRI scans for relapse prediction in pediatric cancer patients. |
| Improved Accuracy | Predicts risk of glioma recurrence with 75-89% accuracy using temporal learning, surpassing traditional single image methods at 50% accuracy. |
| Research Collaboration | Study involved researchers from Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, with nearly 4000 MRI scans analyzed. |
| Temporal Learning Technique | AI trained on sequential MRI scans to recognize subtle changes over time that could indicate cancer recurrence. |
| Future Prospects | Further validation is needed; potential to reduce imaging frequency for low-risk patients or pre-emptive treatment for high-risk individuals. |
| Funding and Support | Study partially funded by the National Institutes of Health, highlighting strong institutional partnerships. |
Summary
The AI tool in pediatric cancer recurrence represents a significant advancement in predicting relapse risks for young patients with gliomas. By utilizing sophisticated temporal learning techniques to analyze multiple brain scans over time, this innovative approach offers a more accurate prediction model than traditional single-scan methods. The study’s success not only enhances our understanding of tumor behavior post-surgery but also paves the way for improved treatment strategies, potentially transforming care for pediatric cancer patients. Continued research and clinical trials will determine how these AI-powered predictions can be integrated into standard medical practices, ultimately aiming for better outcomes in managing pediatric cancer.

Pediatric Brain Cancer: AI Predicts Relapse Risks Accurately
Pediatric brain cancer poses significant challenges for young patients and their families, especially when it comes to the risk of recurrence. Among the various types of tumors, pediatric gliomas stand out due to their intricate nature and treatment variability. A recent Harvard study has shown that an AI tool analyzing MRI scans in children outperforms traditional methods in predicting glioma relapse risk. This breakthrough can enhance brain tumor treatment innovation, offering hope for improved outcomes and reduced stress for families. By leveraging advanced techniques in cancer prediction, we are one step closer to transforming the future of pediatric oncology.
Childhood brain tumors, particularly those categorized as pediatric brain cancer, represent a complex medical challenge with profound implications. Terms like pediatric gliomas or brain tumors specifically signal a variety of growths that affect the developing brain, encompassing everything from benign to malignant forms. Innovations in technology, such as the use of AI in cancer prediction, are increasingly becoming crucial tools in managing these conditions. With the ability to interpret and analyze multiple MRI scans over time, researchers are pioneering approaches that could significantly alter how we assess the risk of glioma relapse. As advancements in brain tumor treatment continue to evolve, the focus on accurate predictions and timely interventions becomes more vital.
The Role of AI in Pediatric Brain Cancer Prediction
Artificial intelligence has revolutionized many fields, and its application in healthcare, particularly in the context of pediatric brain cancer, has garnered significant attention. A recent study has shown that AI tools can analyze MRI scans over time with superior accuracy in predicting the relapse of pediatric gliomas compared to traditional methods. This innovation harnesses complex algorithms to observe subtle changes in brain scans that may indicate the likelihood of cancer recurrence, offering a beacon of hope for early intervention in high-risk cases.
The integration of AI in the prediction and management of pediatric brain cancer signifies a step forward in enhancing patient outcomes. With the ability to aggregate data from multiple scans, AI empowers healthcare professionals to make informed decisions that are tailored to individual risk profiles. This not only supports timely treatments but also alleviates the psychological burden on children and families, as fewer invasive monitoring procedures may be required, shifting focus towards more effective treatment pathways.
Understanding Pediatric Gliomas and Treatment Options
Pediatric gliomas, a type of brain tumor, present unique challenges in both diagnosis and treatment. Though many cases are amenable to surgical intervention, the possibility of relapse often looms large, necessitating ongoing vigilance through MRI scans. Innovations in brain tumor treatment, like combining traditional therapies with cutting-edge AI diagnostics, can lead to improved management strategies, ultimately enhancing survival rates and quality of life for young patients.
Treatment options for pediatric gliomas are evolving, with a focus on personalized therapy approaches and minimizing the long-term impact of the illness on a child’s development. As research progresses, integrating AI and advanced imaging techniques not only aids in assessing tumor characteristics but also paves the way for targeted therapies that specifically cater to the individual tumor’s behavior, proving essential in managing this complex condition.
The Impact of MRI Scans on Pediatric Cancer Management
MRI scans have long been a cornerstone in the diagnosis and monitoring of pediatric brain cancer, including gliomas. The introduction of AI tools promises to elevate the utility of these scans, as they can now be analyzed in a temporal context rather than in isolation. This advancement allows for a comprehensive understanding of tumor progression and relapse risks, informing clinicians and enabling them to adjust treatment plans proactively.
Moreover, the frequency and dosage of MRI scans can often be taxing for young patients. With more accurate predictive capabilities afforded by AI, healthcare providers can optimize imaging schedules, reduce unnecessary stress, and enhance the overall treatment experience. The hope is that by refining how we use MRI technology in pediatric oncology, we can transform not just the effectiveness of monitoring but also the emotional landscape for affected families.
Innovations in Brain Tumor Treatment
The journey toward innovative brain tumor treatment has accelerated dramatically with the rise of AI and its application in predicting pediatric brain cancer outcomes. The ability to analyze data from significant cohorts has informed better therapeutic decisions and customized care plans that evolve alongside patient needs. Innovations in treatment protocols that incorporate insights from AI models hold the potential to revolutionize how pediatric gliomas are managed, maximizing efficacy while minimizing harm.
Furthermore, as research continues, collaborations among institutions such as Mass General Brigham and various children’s hospitals are essential for fostering an environment where cutting-edge techniques can be tested and refined. The goal is a future in which targeted therapies are routinely available, guided by sophisticated AI analytics that can accurately predict responses to treatment and long-term outcomes, rendering outdated practices obsolete.
Challenges in Relapse Prediction for Pediatric Gliomas
Despite advancements, predicting relapse in pediatric gliomas remains fraught with challenges. Each tumor displays its own unique behavior and response to treatment, complicating the creation of a one-size-fits-all model for relapse prediction. Traditional methods have relied heavily on sporadic imaging, and due to their limitations, many high-risk patients might be either over-monitored or not adequately followed, leading to increased anxiety and healthcare costs for families.
However, the use of temporal learning algorithms represents a paradigm shift in how we approach these challenges. By analyzing longitudinal data from multiple MRI scans, researchers have started to bridge the gap between clinical unpredictability and proactive treatment strategies.Continued validation across diverse patient populations will be critical to overcoming these hurdles and establishing AI as a mainstay in relapse prediction for pediatric brain cancer.
Future Directions in Pediatric Oncology Research
Research in pediatric oncology is poised for exciting developments, particularly with the intersection of advanced imaging technologies and artificial intelligence. As the understanding of gliomas deepens, future studies aim to refine diagnostic tools and therapeutic approaches based on AI predictions, enhancing personalized medicine strategies. The focus on pediatric populations necessitates innovative research that acknowledges the unique aspects of childhood cancers and their treatments.
Moreover, scientific inquiry is increasingly moving towards collaborative efforts that leverage interdisciplinary expertise to tackle the complexities associated with pediatric brain cancer. By combining advancements in medical imaging, genetic research, and AI, the prognosis for children diagnosed with brain tumors looks promising. The ultimate vision is to create an integrated healthcare environment where AI not only supports clinical decisions but also enriches the entire patient-care continuum.
Leveraging Technology for Enhanced Patient Care
The advent of AI in healthcare signifies a pivotal moment for enhancing patient care, particularly in challenging fields such as pediatric oncology. By leveraging technology to analyze brain scans, healthcare providers can unlock new insights into patient risks, leading to more effective intervention strategies. This results in better health outcomes and a more supportive experience for patients and families facing the uncertainties of brain cancer.
Emphasizing a technological approach, combined with compassionate care, is vital. By focusing on tailored treatment plans driven by AI predictions, medical teams can create a more responsive and personalized healthcare experience. As research advances, the hope is to continuously improve the tools available for clinicians, ensuring that their patients receive the most appropriate and innovative care possible.
Ethical Considerations in AI-Driven Cancer Treatment
With the integration of AI in predicting and managing pediatric brain cancer, ethical considerations come to the forefront. As AI models become more sophisticated, questions arise about data privacy, the ability to explain AI-driven decisions, and the potential biases inherent in training datasets. Ensuring transparency and accountability in AI applications is crucial to maintaining the trust of patients and families as these technologies become increasingly influential in medical decision-making.
Moreover, the implications of AI on patient choices cannot be overlooked. It is vital to establish guidelines that prioritize the well-being of pediatric patients while respecting their autonomy and that of their families. Ethical frameworks are essential to navigate the complexities of AI in healthcare, ensuring that technological advancements serve to enhance, rather than compromise, the quality of care provided to young patients.
Collaboration and Funding in Cancer Research
The fight against pediatric brain cancer relies heavily on collaboration among research institutions, healthcare providers, and funding bodies. Projects like the one at Mass General Brigham demonstrate the importance of partnerships in accumulating substantial datasets that drive innovative AI modeling and predictive analytics. Not only does this collaborative approach foster shared knowledge and resources, but it also propels the advancement of treatment strategies tailored to the unique needs of pediatric brain cancer patients.
Additionally, sustained funding, such as that provided by the National Institutes of Health, is vital for supporting research that ultimately leads to breakthroughs in understanding and treating pediatric gliomas. By investing in these crucial research initiatives, stakeholders can help unlock the potential for effective therapies and improved patient outcomes, ensuring that future generations of young patients have access to the best possible care.
Frequently Asked Questions
What is pediatric brain cancer and how are gliomas related?
Pediatric brain cancer primarily refers to tumors that occur in children, with gliomas being one of the most common types. These tumors develop from glial cells in the brain and can vary significantly in type, grade, and treatment approach. Understanding the nuances of pediatric gliomas is crucial for developing effective treatment strategies and improving survival outcomes.
How does AI in cancer prediction enhance treatment for pediatric gliomas?
AI in cancer prediction improves treatment for pediatric gliomas by analyzing multiple MRI scans to predict relapse risk more accurately than traditional methods. This innovative approach allows for earlier identification of high-risk patients, leading to more tailored treatment strategies and potentially reducing the burden of frequent MRI scans on young patients.
Why are MRI scans important in monitoring pediatric brain cancer?
MRI scans are essential in monitoring pediatric brain cancer, particularly gliomas, as they provide detailed images of the brain’s structure, enabling doctors to assess tumor size, location, and potential recurrence after treatment. Regular MRI imaging is a key component of post-treatment follow-up to ensure any relapse is detected promptly.
What role does temporal learning play in predicting glioma relapse in children?
Temporal learning plays a pivotal role in predicting glioma relapse in children by training AI models to analyze sequential MRI scans over time. This method enhances the prediction accuracy of cancer recurrence by recognizing subtle changes in the brain’s imaging data, which traditional single-scan analysis often misses.
Can AI tools predict the recurrence of pediatric gliomas effectively?
Yes, AI tools can predict the recurrence of pediatric gliomas effectively. Recent studies have shown that AI models utilizing temporal learning can achieve 75-89% accuracy in predicting relapse within one year post-treatment, significantly outperforming traditional predictive methods that had accuracies around 50%.
What are the implications of AI advancements for pediatric brain tumor treatment innovation?
AI advancements in predicting pediatric brain tumor recurrence hold significant implications for treatment innovation. By accurately identifying patients at high risk for relapse, clinicians can personalize treatment plans, potentially reducing unnecessary interventions for low-risk patients, and focusing resources on high-risk cases for better outcomes.
How are recurrence predictions generated for pediatric brain cancer patients?
Recurrence predictions for pediatric brain cancer patients are generated through advanced AI models that analyze multiple MRI scans taken over time. By applying temporal learning, these models can integrate data from various imaging points to improve prediction accuracy for glioma relapse.
What is the impact of relapse in pediatric gliomas on patient care?
The impact of relapse in pediatric gliomas on patient care can be severe, as recurrences often lead to more complicated treatment regimens, increased stress on families, and potential declines in quality of life. Early prediction of relapse risk through AI can help manage these challenges by informing treatment decisions and follow-up strategies.
What future developments can be expected in pediatric brain cancer treatment due to AI research?
Future developments in pediatric brain cancer treatment are expected to include more personalized treatment plans driven by AI-generated predictions, refined follow-up protocols utilizing machine learning insights, and innovative therapeutic approaches targeting identified high-risk patients, ultimately leading to improved outcomes and optimized care for children with gliomas.
How does the accuracy of AI predictions compare to traditional methods for pediatric glioma recurrence?
The accuracy of AI predictions for pediatric glioma recurrence significantly surpasses traditional methods. Recent studies indicate that AI can predict relapse with 75-89% accuracy, whereas traditional single-image assessments typically yield accuracies closer to random guessing at about 50%.
| Key Point | Details |
|---|---|
| Research Context | Study conducted by Mass General Brigham and collaborators analyzed pediatric brain cancer relapse using an AI tool. |
| AI Tool | AI predicts relapse risk more accurately than traditional methods; accuracy ranges from 75-89%. |
| Temporal Learning | Technique that uses multiple scans over time provides better predictions for cancer recurrence. |
| Impact on Care | Potential to reduce stress from frequent MRIs and personalize treatment based on relapse prediction. |
| Future Steps | Further validation of the AI model is required before clinical application and the start of trials. |
Summary
Pediatric brain cancer is a significant concern for children affected by gliomas and other brain tumors. Innovative advancements, such as an AI tool developed to predict relapse risk, represent a promising shift in treatment and care. This technology significantly outperforms traditional methods, bringing hope for better management of pediatric brain cancer by potentially reducing the burden of frequent imaging procedures. As research progresses, it is crucial to validate these findings to enhance care and improve outcomes for young patients.

Research Funding for Health: A Vital Investment for Progress
Research funding for health plays a pivotal role in advancing public health initiatives and innovation in medical science. It provides the financial support necessary for scholars to explore vital areas such as cancer research, nutrition, and human health. Institutions like Harvard receive substantial contributions through NIH grant applications, which facilitate groundbreaking studies that can significantly impact disease prevention and treatment. However, the landscape of research funding is fraught with challenges, including competitive grant reviews and potential reductions in federal allocations. Despite these hurdles, successful funding not only accelerates scientific discovery but also ensures community health advancements, making it an essential aspect of modern healthcare.
Health-related research financing encompasses various terms and concepts crucial for enhancing scientific exploration and public welfare. Creative funding mechanisms, such as grants from national health organizations and private institutions, enable researchers to delve into critical topics like cancer prevention and nutrition’s impact on well-being. Securing a Harvard research grant or an NIH grant application represents a significant milestone for academic professionals striving to address pressing health challenges. Moreover, the intricate process involved in applying for research funding emphasizes the importance of thorough preparation and innovative thinking. As we navigate the complexities of healthcare research funding, it becomes clear that these financial resources are vital for future advancements in public health strategies.
The Importance of Research Funding for Health Long-Term Progress
Research funding plays a central role in the advancement of public health and medical sciences. Without adequate financial support, significant projects aimed at discovering new treatments or understanding complex health issues can come to a grinding halt. For instance, the National Institutes of Health (NIH) provides essential grants that not only enable researchers to delve into pressing health concerns but also support the workforce needed to carry out these critical studies. The carefully structured grant application process ensures that only the most innovative and impactful projects receive funding, which is crucial given the thousands of applications submitted each year.
Candid conversations about cancer research funding highlight the serious ramifications of funding freezes. Recent political shifts and budget cuts threaten to disrupt ongoing studies which aim to lower cancer risks or even eradicate certain types of cancer. For researchers like Karen Emmons, securing funding is not just about financial support; it’s also a commitment to communities that rely on academic advancements for better health outcomes. Thus, maintaining a steady influx of research funding for health is paramount to ensuring societal progress and addressing the myriad of health disparities in populations nationwide.
Navigating the NIH Grant Application Process
Successfully securing an NIH grant is a meticulous journey that starts long before the actual application is submitted. As experienced researchers like Jorge Chavarro highlight, the process involves extensive pre-planning, including identifying evidence gaps and potential impacts of the research. Researchers must work to create networks within the community and engage with peers to avoid duplicating previous efforts. Once an innovative idea is established, every detail must be mapped out, sometimes requiring months of work to write compelling narratives that appeal to grant reviewers.
The complete NIH grant application, which may encompass over 100 pages, encapsulates a comprehensive breakdown of prior results, methodologies, and ethical considerations. Given the rigorous nature of the review process involving multiple levels of scrutiny from Scientific Review Groups and advisory councils, the stakes are extremely high. Each successful application not only leads to funding but also signifies a stamp of approval from the scientific community regarding the research’s potential significance and feasibility in advancing public health.
Public Health Research: A Collaborative Effort
The intersection of public health research and community involvement is becoming increasingly recognized as vital for effective health interventions. Researchers like Karen Emmons emphasize the necessity of community partnerships to address disparities, especially when targeting under-resourced populations. By forging these connections, researchers can tailor their studies more appropriately to meet the specific health needs of different communities, resulting in more effective interventions and health outcomes.
Furthermore, collaboration extends beyond the community into academia and government sectors. The partnership between universities, such as Harvard, and the government reflects an acknowledgment of mutual benefits in fostering public health initiatives. These collaborations not only facilitate the sharing of knowledge and resources but also catalyze innovation by pooling diverse expertise to tackle pressing health challenges effectively.
Funding Disruptions and Their Impact on Health Research
Recent disruptions in research funding underscore the precarious nature of public health research investment. The implications of funding freezes, like those faced by Harvard, can stall crucial studies that are essential for understanding and improving health conditions. When significant funding streams are interrupted, researchers are left scrambling to adapt, often resulting in delayed studies and lost opportunities for making urgent health advancements.
Moreover, funding withdrawals can lead to a chilling effect on new research ideas and proposals. As the competitive landscape of grant applications tightens, researchers might shy away from pursuing groundbreaking projects due to fears of rejection. This ultimately hampers innovation in the field, which is alarming given our society’s need for fresh solutions to enduring health crises, including cancer and nutrition-related issues.
Innovations Driven by Federal Research Grants
Federal research grants can serve as a remarkable catalyst for innovation within health sciences. As academic institutions compete for limited resources, they are compelled to push the boundaries of conventional research, exploring new methodologies and technologies that might significantly alter how diseases are understood and treated. Researchers at institutions like Harvard have pioneered groundbreaking studies resulting from this fiercely competitive funding landscape.
For example, advancements in genomic medicine and precision health are often the direct result of federal support for inventive proposals. By investing in diverse research projects, funding agencies help nurture a culture of exploration that has the potential to yield life-saving therapies and improve overall public health outcomes. Therefore, the commitment to fostering innovation through robust research funding is essential for the future development of healthcare solutions.
Maximizing Grant Writing Strategies for Success
Crafting a successful grant proposal requires not only innovative ideas but also a strategic approach to writing. Skilled researchers understand the significance of articulating clear objectives and impactful outcomes as part of their application. They must convey how their project contributes to existing knowledge and public health, which involves effectively communicating complex scientific ideas in an accessible manner to reviewers.
Furthermore, establishing strong preliminary data is critical in demonstrating the credibility of the proposed research. The best grant proposals often showcase significant past achievements, progressive methodologies, and the research team’s qualifications. By meticulously developing each component of the application, from the initial specific aims to detailed financial breakdowns, researchers enhance their chances of securing vital funding needed to propel public health inquiries.
The Role of Peer Review in Research Funding Evaluation
Peer review serves as the backbone of the NIH grant application process, ensuring that applications are evaluated by knowledgeable experts in the field. This section of the application journey is crucial as it provides a platform for constructive feedback and fosters high standards within the research community. Reviewers not only assess the significance and innovation of the proposed studies but also their methodological soundness, which adds an important layer of quality control to the funding distribution process.
However, navigating peer reviews can be intense. Proposals that do not meet specific thresholds may be rejected even after extensive prior work. Researchers are encouraged to embrace this feedback, as it can significantly strengthen future submissions, enabling them to refine their methodologies and research focus. A well-rounded understanding of the review dynamics ultimately empowers researchers to contribute more effectively to the ongoing dialogue in public health research.
Networking in Research: Key to Fundraising Success
Building professional networks is an essential skill for researchers aiming to secure funding for their projects. Establishing connections with peers and community stakeholders can provide insights into research trends, funding opportunities, and potential collaborations. For many public health researchers, these networks create pathways to diversify their proposals, making them more attractive to funding agencies.
Moreover, collaborative relationships often open doors for multidisciplinary projects that combine various areas of expertise. Such innovative approaches can attract funding from different sources, revealing new aspects of health research that might not ordinarily be addressed. Therefore, strategic networking not only enhances the quality of research proposals but also broadens the scope of potential funding.
Challenges and Opportunities in Nutrition Research Funding
Nutrition and human health research represents a compelling area of inquiry, yet it often faces substantial funding challenges. Areas such as nutrition policies, dietary impacts on disease prevention, and community nutrition interventions require scientific exploration that can sometimes be overlooked in favor of more traditional medical research disciplines. Consequently, securing research funding for nutrition studies becomes critical, especially in educating populations about healthier lifestyles and food choices.
Researchers like Jorge Chavarro actively advocate for the importance of advancing nutrition science, recognizing its impact on human reproduction and overall public health. By framing nutrition research in terms of its direct implications for health outcomes, researchers can more effectively communicate the value of their work to potential funding bodies, paving the way for new grants that could drive innovative studies forward.
Frequently Asked Questions
What is the NIH grant application process for public health research?
The NIH grant application process for public health research is pivotal for securing funding to address health challenges. It starts with a one-page specific aims statement that outlines the research objectives and significance of the project. Researchers must provide detailed methodologies, preliminary results, and extensive documentation, particularly if human participants are involved. Applications undergo rigorous reviews by Scientific Review Groups, where they’re evaluated for innovation and impact, ensuring that only the most promising projects receive funding.
How can researchers secure cancer research funding from the National Cancer Institute?
Researchers can secure cancer research funding from the National Cancer Institute (NCI) by submitting a meticulously prepared NIH grant application. This involves demonstrating the need for the study, articulating innovative approaches, and providing robust scientific evidence. Proposals are scored based on their significance and methodology during the two-tier review process conducted by volunteer scientists. Given the competitive nature, with a success rate of about 14.6% for R01 grants, it is essential to showcase clear and impactful research objectives.
What are Harvard research grants available for studying nutrition and human health?
Harvard research grants for studying nutrition and human health focus on innovative projects that aim to advance our understanding of dietary impacts on health. Researchers can apply for various funding sources, including internal grants from Harvard and federal NIH grants. These applications typically require a detailed explanation of the significance of the research, expected outcomes, and methodologies used. Such funding is crucial for researchers like Jorge Chavarro, who explore the connections between nutrition and human reproduction.
What factors should be considered when applying for public health research funding?
When applying for public health research funding, several factors should be considered: establishing community partnerships to ensure relevance, staying updated with recent advancements in the field, and demonstrating the novelty of the proposed research. It’s also vital to present a compelling scientific rationale, detailed methodologies, accurate budgeting, and compliance with ethical standards. A successful application not only outlines the research goals but also shows a commitment to improving health outcomes in the community.
How do funding opportunities impact public health research initiatives?
Funding opportunities play a critical role in shaping public health research initiatives. Access to resources through grants like NIH allows researchers to conduct vital studies that can lead to innovations in health and well-being. These grants support the development of strategies to combat issues such as cancer, nutrition-related diseases, and neurodegenerative conditions. Without adequate funding, many promising research avenues may remain unexplored, thereby hindering progress in public health.
What is the significance of the NIH grant application in advancing health research?
The NIH grant application is significant in advancing health research as it provides essential financial support needed to investigate and address pressing health challenges. By requiring a rigorous and detailed application process, the NIH ensures that only high-quality, impactful research projects receive funding. This process not only fosters innovation but also strengthens the commitment of the scientific community to improving human health outcomes through evidence-based research.
| Key Points | Details |
|---|---|
| Importance of Federal Grants | Federal grants enable researchers to impact public health significantly by allowing them to pursue essential studies. |
| Challenges in Securing Funding | Recent political actions have frozen substantial funding, disrupting vital research on health-related issues. |
| Research Process and Requirements | Grant applications require extensive preparation, including detailed proposals, budgets, and ethical considerations. |
| Funding Success Rates | Only about 14.6% of research proposals at the National Cancer Institute were funded, highlighting the competitive nature of research funding. |
| Role of Community Engagement | Collaborating with community partners is essential for researchers to identify and fill gaps in public health. |
| Long-term Investment in Health | Public-private partnerships support research that benefits society by enhancing health care and reducing costs. |
Summary
Research funding for health is crucial as it enables scientists and public health researchers to investigate pressing health issues and develop innovative solutions. Securing these funds can be a challenging and competitive process, yet it plays a fundamental role in advancing medical knowledge and improving patient care. As illustrated by the experiences of leading researchers at institutions like Harvard, the efforts to obtain federal grants are not just bureaucratic tasks; they reflect a commitment to enhancing public health outcomes. In an increasingly resource-constrained environment, continued investment and support for research funding in health must be prioritized to ensure ongoing advancements that benefit society as a whole.
Alzheimer’s Research: Beth Stevens’ Breakthrough Discoveries
Alzheimer’s research is at the forefront of addressing the complexities surrounding this devastating disease, which affects millions globally. Scientists like Beth Stevens are uncovering the critical role of microglial cells, the brain’s immune system, in the development and progression of neurodegenerative diseases. By understanding how these cells function, particularly in processes like synaptic pruning, researchers can identify potential biomarkers for Alzheimer’s that may pave the way for earlier diagnosis and innovative Alzheimer’s treatment options. Stevens’ groundbreaking work highlights the importance of foundational research in transforming our approach to combating this illness. As the number of individuals affected by Alzheimer’s is projected to soar, these scientific advancements are imperative for improving patient outcomes and reducing the financial burden on healthcare systems.
Exploring the intricacies of dementia-related ailments such as Alzheimer’s requires a new lens of scientific inquiry and innovation. The study of immune cells in the brain, particularly in the context of cognitive decline, has led to significant revelations about their roles in neuronal health. Researchers are now investigating the interplay between these immune agents and the pathology of memory disorders, as well as their potential as clinical markers for early detection. Pioneering work in this domain not only aids in deciphering the biology behind Alzheimer’s but also spurs the development of effective therapeutic strategies. As we advance our understanding of the cerebral landscape, the path toward addressing age-related cognitive impairments becomes clearer.
The Role of Microglial Cells in Neurodegenerative Diseases
Microglial cells serve as the primary immune defense in the brain, constantly monitoring the neural environment for signs of damage or disease. These cells play a multifaceted role in neurodegenerative conditions like Alzheimer’s disease by engaging in the removal of dead neurons and orchestrating synaptic pruning. However, their function is complex; an imbalance in their activity can lead to the mismanagement of neural circuits, potentially exacerbating conditions such as Alzheimer’s and Huntington’s disease. Recognizing the importance of microglia as both protectors and potential sources of pathology is crucial for developing innovative therapeutics.
Recent studies led by Beth Stevens have illuminated how misguided pruning by microglial cells may contribute to the cognitive decline associated with Alzheimer’s. In this way, microglia are not merely passive observers but active participants in disease progression. Their dual role emphasizes the need for targeted research into therapies that could modulate microglial activity, potentially leading to new treatment strategies that address the underlying neuroinflammatory processes in Alzheimer’s, ultimately providing hope for the millions affected.
Advancements in Alzheimer’s Research and Treatment
Alzheimer’s research has significantly evolved in recent years, particularly in understanding the role of microglial cells and identifying biomarkers for the disease. These advancements have opened new pathways for diagnosis and treatment, effectively shifting the paradigm in Alzheimer’s care. Beth Stevens and her team are at the forefront of this transformation, emphasizing that foundational research into microglia could lead to breakthroughs in spotting the disease before classic symptoms emerge, thereby allowing for earlier interventions.
The prospect of developing medications that target specific aspects of neurodegenerative diseases presents a vital opportunity to improve patient outcomes. As the population ages, with projected annual cases soaring, understanding the pathology of Alzheimer’s through the lens of microglial dysfunction becomes increasingly essential. This research promises to inform not only therapeutic strategies but also public health initiatives aimed at mitigating the impending crisis in dementia care.
Insights from Beth Stevens’ Research Journey
Beth Stevens’ journey in Alzheimer’s research exemplifies the profound impact of curiosity-driven science on understanding complex neurological processes. Her work highlights the importance of scientific exploration, driven by funding support from institutions like the National Institutes of Health. Stevens’ narrative underscores the often-unpredictable nature of fundamental research; what may seem like an intrinsic curiosity about a mouse’s visual system can yield insights with far-reaching implications for human health in neurodegenerative conditions.
With accolades such as the MacArthur Fellowship, Stevens showcases how persistent inquiry into basic science can yield practical applications for diseases such as Alzheimer’s. Her determination to follow the science, even in its most basic forms, provides a blueprint for future researchers. By examining how microglia interact with neural circuits, her team continues to unravel the complexities of brain health and disease, paving the way for therapies that could one day enhance quality of life for those impacted by Alzheimer’s.
The Future of Biomarkers in Alzheimer’s Detection
As the quest for effective Alzheimer’s treatments progresses, the identification of biomarkers has emerged as a crucial area of focus. Biomarkers can facilitate earlier diagnosis and better monitoring of disease progression. Beth Stevens has contributed significantly to this domain by exploring the cellular mechanisms at play in Alzheimer’s disease. By understanding how microglial cells function, researchers hope to develop biomarkers that accurately reflect the disease’s biological changes, advancing the timelines for intervention and treatment.
The potential for biomarker-driven strategies is immense, as they could lead to personalized medicine approaches tailored to the individual’s unique disease profile. This could not only enhance treatment efficacy but also help in tracking responses to therapy in real time. As scientists continue to unravel the cellular dynamics in neurodegenerative diseases, the pipeline for effective Alzheimer’s biomarkers could revolutionize the landscape of early detection and therapeutic decision-making, ultimately providing a beacon of hope for millions.
The Impact of Aging Population on Alzheimer’s Research
The growing aging population presents both challenges and opportunities in the realm of Alzheimer’s research. As life expectancy increases, so does the incidence of neurodegenerative diseases such as Alzheimer’s, with projections estimating a significant rise in cases. This demographic shift necessitates urgent attention to research, funding, and healthcare strategies aimed at combating Alzheimer’s and supporting affected individuals and their families.
With around 7 million Americans currently living with Alzheimer’s, the projected rise in cases by 2050 posits a potential healthcare crisis, elevating care costs dramatically. Thus, innovative research led by scientists like Beth Stevens is paramount in developing not only effective treatments but also preventive strategies, ensuring that the healthcare system is adequately equipped to manage the anticipated surge in Alzheimer’s cases across the nation.
Foundational Science and Its Role in Disease Understanding
Foundational science plays a critical role in informing our understanding of complex diseases, including Alzheimer’s. Researchers such as Beth Stevens emphasize that without robust basic scientific investigations, advancements in clinical application remain limited. Curiosity-driven studies into microglial cells and their function in neural development have ignited discussions around potential links to Alzheimer’s pathology, illustrating that what starts as basic science can lead to groundbreaking discoveries in disease understanding and treatment.
Stevens’ perspective teaches us that the relationship between basic research and its translational impact is pivotal. Each experiment, each discovery in understanding brain immune responses, is a building block towards deciphering the mechanisms behind diseases such as Alzheimer’s. As the field progresses, it is essential to recognize and support the interplay between foundational research and clinical innovation, which will ultimately drive the next generation of Alzheimer’s treatments.
The Role of Federal Funding in Alzheimer’s Research
Federal funding remains a cornerstone for advancing Alzheimer’s research, enabling scientists like Beth Stevens to pursue ambitious studies that might otherwise be unfunded. The consistent support from agencies such as the National Institutes of Health not only fuels groundbreaking research but also catalyzes collaborative efforts among institutions. These financial resources are critical in the long-term quest to unveil the mechanisms behind Alzheimer’s and other neurodegenerative diseases, as they facilitate comprehensive explorative studies able to yield significant insights.
Moreover, funding allows researchers to delve into developing therapies that could mitigate conditions exacerbated by microglial dysfunction, offering hope for millions affected by Alzheimer’s. As the urgency to combat this disease intensifies with an aging population, securing robust funding for Alzheimer’s research becomes essential to propel innovative solutions that could impact diagnosis, treatment, and ultimately, patients’ lives.
Future Directions in Alzheimer’s Treatment Research
The landscape of Alzheimer’s treatment is poised for transformation as researchers pivot towards innovative strategies that stem from recent findings about microglial cells. Current studies aim to identify precise mechanisms that underlie the disease, thereby opening doors to targeted therapies that truly address the intricacies of Alzheimer’s pathology. The shift towards a more nuanced understanding of these immune cells has prompted a re-examination of established treatment protocols and a quest for novel interventions.
As excitement builds around the possibilities of new medications derived from mechanistic insights into Alzheimer’s, it is crucial for the research community to remain collaborative and open-minded. The involvement of experts like Beth Stevens ensures a multidisciplinary approach that marries basic science with clinical application. This dynamic could lead to advancements not only in pharmacological treatments but also in preventive strategies aimed at delaying the onset of Alzheimer’s, defining the future of care for millions.
Understanding the Mechanisms of Synaptic Pruning
Synaptic pruning is a natural process essential for brain development and efficiency, involving the selective removal of synapses to facilitate more effective neural communication. However, dysfunction in this process, particularly involving microglial cells, can contribute to neurodegenerative diseases like Alzheimer’s. Beth Stevens’ research emphasizes this critical link, revealing that precise modulation of microglial activity can either support healthy brain function or lead to detrimental outcomes, emphasizing the need for vigilance in understanding these mechanisms as we strive for effective treatments.
Continuing to explore the intricacies of synaptic pruning opens new avenues for therapeutic intervention in Alzheimer’s. By targeting the pathways through which microglial cells operate, researchers can develop strategies that enhance the brain’s resilience to damage. This comprehensive understanding has the potential to redefine how we approach both prevention and treatment of Alzheimer’s, ultimately leading to improved outcomes for those at risk of or living with this complex disease.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are crucial in Alzheimer’s research as they function as the brain’s immune system. They monitor the brain for signs of illness and damage, aiding in the removal of dead cells and pruning synapses. However, improper pruning by microglia can contribute to the progression of Alzheimer’s disease, making them a focal point for developing new Alzheimer’s treatments.
How are biomarkers for Alzheimer’s disease identified through research?
Research into Alzheimer’s disease has led to the identification of biomarkers, which are biological indicators of the disease. Studies, such as those led by Beth Stevens, focus on the functioning of microglial cells and their role in neurodegenerative diseases. These biomarkers can enable earlier detection of Alzheimer’s, potentially leading to more effective treatments.
What advancements in Alzheimer’s treatment have come from studying microglial cells?
Advancements in Alzheimer’s treatment arising from the study of microglial cells include new therapeutic strategies aimed at enhancing the normal functions of microglia. By understanding how these immune cells fail to prune synapses correctly, researchers like Beth Stevens are paving the way for innovative treatments that address the underlying mechanisms of Alzheimer’s disease.
How does Beth Stevens’ research contribute to understanding neurodegenerative diseases?
Beth Stevens’ research significantly contributes to understanding neurodegenerative diseases like Alzheimer’s by investigating the behavior of microglial cells. Her findings have illustrated how these immune cells can impact synaptic integrity and lead to disease progression, thereby influencing future research directions and treatment approaches.
Why is finding new biomarkers for Alzheimer’s disease important?
Finding new biomarkers for Alzheimer’s disease is essential because they provide critical insights into the disease’s progression and enable earlier diagnosis. Early detection can lead to timely interventions, significantly impacting treatment outcomes for those affected by Alzheimer’s and other neurodegenerative diseases.
What is the significance of foundational research in Alzheimer’s studies?
Foundational research is vital in Alzheimer’s studies as it lays the groundwork for understanding complex biological processes. It provides the fundamental knowledge necessary to explore disease mechanisms, such as the role of microglial cells, ultimately leading to the development of effective therapies and diagnostic tools for Alzheimer’s.
| Key Points | Details |
|---|---|
| Microglial Cells | Act as the brain’s immune system, involved in synapse pruning and removal of dead cells. |
| Research Implications | Improper pruning linked to Alzheimer’s and other neurodegenerative diseases could lead to new medications and early detection biomarkers. |
| Beth Stevens | Neuroscientist at Boston Children’s Hospital, recognized for her work on microglia, and a MacArthur Fellow. |
| Future Projections | Annual Alzheimer’s cases expected to double by 2050, escalating the cost of care significantly. |
| Funding Importance | Federal support, particularly from the NIH, is crucial for advancing foundational research. |
Summary
Alzheimer’s research is advancing significantly through the pioneering work of scientists like Beth Stevens, who are uncovering critical insights into the brain’s immune response. Her research highlights the role of microglial cells in synaptic pruning and their implications for Alzheimer’s disease. By understanding the underlying mechanisms of neurodegenerative diseases, Stevens’ work lays the foundation for innovative treatments and early detection methods that could greatly enhance the quality of life for millions affected by Alzheimer’s.

Youth Well-Being: Insights from the Global Flourishing Study
Youth well-being is becoming an increasingly important topic in today’s society, highlighting the need for a collective effort to support young individuals in their development. Recent findings from the Global Flourishing Study reveal concerning trends regarding youth mental health, shedding light on the relationship between economic factors such as financial security and happiness, and personal connections like the importance of relationships. This comprehensive research emphasizes that merely having financial resources does not guarantee the flourishing of young people. In fact, many lower-income countries report higher levels of youth well-being compared to wealthier nations, challenging the notion that economic development leads directly to enhanced happiness. As we navigate these complex issues, it becomes crucial to address how nurturing socio-emotional skills and fostering supportive environments can enhance youth well-being and promote thriving communities.
The topic of young people’s overall health and happiness is vital for understanding their future prospects and societal contributions. This discussion encompasses various aspects such as mental wellness, social connections, and the gratifying elements that contribute to a fulfilling life. Emerging research indicates that the prosperity of youth is closely tied to their emotional and relational experiences rather than solely their financial circumstances. Indeed, the nuances of development during these formative years require a deeper examination of how social and economic factors interact to shape overall well-being. As we delve into the dimensions of youth health, it is essential to explore strategies that bolster resilience and enrich relationships among young individuals.
Understanding Youth Well-Being in the Context of Economic Development
Youth well-being is a crucial measure of a nation’s health, and the latest insights from the Global Flourishing Study shed light on this pressing issue. Financial security is often seen as a primary contributor to happiness, yet the findings illustrate that economic prosperity alone does not guarantee flourishing among younger populations. For instance, while countries like Japan boast significant wealth and longevity, their youth experience lower levels of well-being compared to nations with less financial affluence, such as Indonesia. This paradox emphasizes the importance of creating supportive environments that nurture the emotional and social health of young people, beyond mere economic indicators.
Furthermore, the study highlights the integral role that relationships play in youth well-being. Strong parental ties and healthy social connections during childhood have been universally linked to higher levels of flourishing in adulthood. This reveals a critical aspect of youth development: while striving for financial security is important, fostering nurturing relationships and a sense of community may have an even more profound impact on young people’s happiness and long-term satisfaction. As such, policymakers and educators must prioritize initiatives that enhance social networks and supportive family dynamics among youth.
The Interplay Between Financial Security and Happiness
The traditional view that financial security leads directly to happiness is being challenged by recent findings from the Global Flourishing Study. Data from 22 nations, encompassing diverse economic backgrounds, reveal that the connection between wealth and well-being is complex and not always linear. For example, while countries like the United States rank high in terms of wealth, they fall short in mental health metrics when compared to lower-income nations that prioritize social relationships and community support. This suggests that true happiness may arise from social engagement and fulfillment rather than from financial gains alone.
Moreover, the study prompts a reevaluation of how wealth is measured against the backdrop of emotional fulfillment. In many regions, financial security has been linked to increased stress, particularly among younger demographics facing economic pressures alongside personal expectations. This highlights the potential for financial well-being to coexist with mental health struggles, complicating the narrative that money equates to happiness. Future economic development initiatives should, therefore, consider not only the growth of wealth but also the enhancement of mental health resources and community engagement strategies that foster a holistic sense of well-being.
The Importance of Relationships in Youth Flourishing
A striking takeaway from the Global Flourishing Study is the paramount importance of relationships in promoting youth flourishing. Empirical evidence suggests that youth who maintain strong connections with family and peers demonstrate higher levels of overall well-being. These relationships provide emotional support and a sense of belonging, which are essential for youth navigating the complexities of adolescence and young adulthood. As such, creating environments where positive, nurturing relationships can thrive is vital for enhancing youth mental health and resilience.
The findings also highlight that youth flourishing is closely tied to social engagement and community involvement. In many higher-ranked nations, such as Mexico and the Philippines, the correlations between social interactions and youth happiness are profoundly evident. By contrast, wealthier nations often exhibit isolation among their youth, resulting in lower levels of contentment and mental health issues. Therefore, cultivating programs and initiatives that encourage participation in communal activities, mentorship, and peer support can yield significant benefits for youth flourishing. Investing in social capital is just as important as examining financial metrics.
The Global Flourishing Study: A Wake-Up Call for Youth Investments
The Global Flourishing Study serves as a critical wake-up call for governments and organizations invested in the well-being of youth. With evidence indicating a troubling trend—where youth are flourishing less than older adults—there is an urgent need to reassess how resources are allocated. While financial security is undoubtedly a component of well-being, the study emphasizes that to truly impact youth well-being, investments must focus on holistic development, encompassing mental health support, robust educational opportunities, and strong community structures that foster connection.
Moreover, the findings indicate that efforts to bolster youth well-being should not be an afterthought, but rather a fundamental aspect of policy reform. As societies continue to advance economically, there must be parallel initiatives that address the emotional and relational needs of young people. This may involve cultivating innovative programs that connect youth with mentors and promote resilience through community-building activities. Comprehensive approaches that merge financial stability with relational well-being could pave the way for a healthier, more flourishing generation.
Reevaluating Economic Development Strategies for Youth Well-Being
As the Global Flourishing Study suggests, economic development strategies require a profound reevaluation to prioritize the well-being of youth. While improving economic conditions is critical, it is essential to recognize that simply increasing wealth does not directly translate into enhanced happiness or flourishing. Countries like Nigeria and Israel, which ranked well in certain areas of the study, exemplify this need for balance between economic growth and the cultivation of meaningful relationships and a supportive environment for youth.
This raises important questions about how nations can pursue economic development that aligns with the values of community and social cohesion. Efforts should focus on creating frameworks that allow economic progress to act as a means to enhance youth well-being, rather than an end goal with no social context. Sustainable development plans need to include strategies that promote mental health, educational access, and family support systems that facilitate deeper connections among youth. Only then can economic development truly contribute to a flourishing society.
The Global Perspective on Youth Mental Health
The Global Flourishing Study has illuminated the significant disparities in youth mental health across different nations. While financial security plays a role, it is evident that varying cultural, social, and familial factors heavily influence young people’s mental well-being. Areas like health, happiness, relationships, and character intersect uniquely within different environments, suggesting that localized approaches are essential in addressing youth mental health challenges. For example, while Japan may be economically developed, its youth experience alarming rates of isolation and mental distress—issues that require targeted interventions that consider cultural contexts.
Furthermore, addressing youth mental health cannot be undertaken in isolation. The interconnectedness of relationships, community, and individual well-being underscores the necessity for comprehensive strategies that include educational institutions, families, and local organizations. By embracing a global perspective while still tailoring solutions to fit local demands, stakeholders can foster healthier environments that equip youth with the tools they need for flourishing. Policy frameworks should incorporate mental health education, stigma reduction campaigns, and accessible resources that empower youth to thrive.
Exploring Spiritual Well-Being in Youth Flourishing
The intersection of spiritual well-being and youth flourishing emerges as a crucial area of exploration within the findings of the Global Flourishing Study. The data reveals that regular participation in spiritual practices, such as attending religious services, correlates with higher levels of overall well-being among youth. This points to the potential benefits that spiritual communities can provide, offering young individuals a sense of purpose and belonging that complements their emotional and psychological needs. Thus, fostering opportunities for youth to engage in spiritual exploration may yield favorable outcomes for their happiness and fulfillment.
Moreover, spiritual well-being can play an essential role during tumultuous transitional phases in adolescence and early adulthood. In many cases, when youth face challenges such as identity formation or societal pressures, spirituality can act as a stabilizing influence, providing comfort and support. Encouraging open discussions about spirituality, alongside mental health education, can help young people access important resources that guide them towards flourishing. As society advances, integrating discussions of spiritual health into youth programming could enhance support systems, leading to a more rounded approach to overall well-being.
Future Research Directions in Youth Flourishing
The vast dataset collected through the Global Flourishing Study paves the way for future research focusing on youth well-being. With longitudinal data being gathered annually, researchers have the opportunity to dive deeper into the underlying factors that contribute to flourishing across various cultures. Such analysis can uncover crucial patterns regarding how economic, social, and emotional parameters interact to shape the youth experience globally. This longitudinal approach will also allow for the monitoring of changes over time, which is vital for developing contextualized interventions that adapt to emerging trends.
In addition to examining existing data, researchers should also expand their inquiries into the specific characteristics that promote resilience among youth in different cultural contexts. Exploring variables like familial support, community engagement, and socio-economic factors can provide a comprehensive understanding of youth well-being. By identifying and analyzing these variables, stakeholders—from policymakers to educators—can better design programs that foster flourishing among young people, ensuring that their developmental needs are met in an increasingly complex world.
Frequently Asked Questions
What is the Global Flourishing Study and how does it relate to youth well-being?
The Global Flourishing Study is a comprehensive investigation assessing individual well-being across nations. It specifically examines factors that contribute to youth well-being, such as health, happiness, relationships, and economic circumstances. Conducted with a diverse sample worldwide, the study highlights significant trends in youth mental health and the importance of financial security in fostering a flourishing life.
How does financial security affect youth well-being according to the Global Flourishing Study?
The Global Flourishing Study reveals that financial security is only one aspect of youth well-being. While financial conditions play a role, factors like relationships and community connections are equally crucial. This demonstrates that youth mental health can thrive in environments where supportive relationships exist, regardless of economic status.
Why are relationships considered important for youth well-being?
Relationships are vital for youth well-being as they provide emotional support, foster social connections, and contribute to a sense of belonging. The Global Flourishing Study indicates that youth who report strong familial and social ties experience higher levels of happiness and overall flourishing.
What are the key factors affecting youth mental health identified in the Global Flourishing Study?
Key factors affecting youth mental health identified in the Global Flourishing Study include childhood health, family dynamics, social relationships, and spiritual well-being. A supportive environment during childhood is crucial for promoting resilience and escalating levels of happiness and flourishing as youth transition into adulthood.
How does economic development influence youth well-being according to the findings of the Global Flourishing Study?
The findings from the Global Flourishing Study suggest that economic development does not automatically guarantee youth well-being. While wealthier nations tend to have more resources, lower-income countries like Indonesia have shown higher levels of social connectedness and youth flourishing due to strong community ties and supportive relationships.
What implications do the findings of the Global Flourishing Study have for youth investment policies?
The findings imply that investment policies should prioritize nurturing relationships and community support systems alongside financial initiatives. Enhancing youth well-being requires a multifaceted approach that encourages social connectedness, mental health resources, and opportunities for meaningful relationships, rather than solely focusing on economic metrics.
How can parents and communities improve youth well-being based on the Global Flourishing Study results?
Parents and communities can improve youth well-being by fostering strong relationships, encouraging open communication, and providing supportive environments. Engaging youth in community activities and ensuring access to mental health resources are also essential for promoting happiness and flourishing outcomes.
What trends concerning youth flourishing have emerged from the Global Flourishing Study?
The Global Flourishing Study has revealed a concerning trend where measures of youth flourishing have plateaued from the late teens into the 20s, showing a lack of happiness during these formative years, particularly in the U.S. This shift indicates the need for targeted interventions to enhance youth mental health and overall well-being.
In what ways does the Global Flourishing Study suggest balancing economic development with youth well-being?
The Global Flourishing Study suggests that societies should balance economic development with youth well-being by integrating measures of happiness, relationships, and meaning into policies. By doing so, nations can promote a holistic approach to development that supports both economic growth and the flourishing of youth.
What role does spirituality play in youth well-being according to the Global Flourishing Study?
Spirituality plays a significant role in youth well-being, as indicated in the Global Flourishing Study. Regular participation in religious or spiritual activities is linked to higher levels of flourishing and mental health, emphasizing the importance of spiritual pathways in fostering a sense of purpose and connectedness among youth.
| Key Points |
|---|
| A global study of youth well-being reveals troubling trends, particularly in wealthier nations like the U.S., where youth flourishing rates are significantly lower than those of older adults. |
| The study involved 203,000 participants from diverse countries to assess factors contributing to well-being, including health, happiness, and relationships. |
| Ranking countries without financial indicators showed Indonesia and Mexico leading in youth well-being, while the U.S. ranked 15th. |
| Childhood relationships and good health significantly predict adult flourishing. |
Summary
Youth well-being is a critical issue highlighted by a recent study showing that financial success does not equate to higher levels of happiness and fulfillment among young people. This research emphasizes the need for society to invest more in youth development, as factors like relationships and health play vital roles in their overall flourishing. Addressing these concerns is essential for ensuring that future generations can thrive both personally and as part of a community.

Global Health: Atul Gawande’s Warning on USAID Cuts
Global health stands at a critical juncture, with recent policy shifts posing substantial challenges to international health systems. Notably, Atul Gawande, a prominent figure in health leadership and former head of USAID’s Bureau for Global Health, has highlighted the detrimental effects of funding cuts on vital health infrastructure. The drastic reduction of public health funding has left millions vulnerable, marking a significant step back for the U.S. as a leader in global health initiatives. As Gawande notes, the dismantling of programs has not only hindered disease surveillance but has also stunted advancements in maternal and child health. This situation demands urgent attention and a reimagining of how we approach partnerships and support in global health.
The realm of international wellness and health management is currently experiencing unprecedented turbulence, significantly affecting vulnerable populations worldwide. Influential medical professionals like Atul Gawande have brought attention to the escalating crisis stemming from reduced financial support for essential health services. As federal programs face cuts, the backbone of health infrastructure, particularly in regions reliant on USAID, is at risk of collapse. Challenges such as these underline the urgency for innovative solutions and reinforced collaboration amongst nations, foundations, and health authorities. Ultimately, safeguarding global health requires a concerted effort to address the funding deficits that threaten to unravel years of progress.
Impact of USAID Cuts on Global Health
The cuts made to USAID represent a critical juncture for global health initiatives and have left a significant void in health infrastructure globally. As Atul Gawande noted, these decisions have not only dismantled the agency’s operational capacity but have also diminished the United States’ stature as a global health leader. Programs that were pivotal in tracking and responding to infectious diseases like Ebola and bird flu have been severely impacted, leading to increased vulnerability in many nations. In essence, such cuts translate into a less coordinated global response to health crises, which can ultimately cost lives.
Furthermore, the termination of over 85% of USAID programs disrupts critical health interventions that have historically improved health outcomes worldwide. From enhancing maternal and child health to fighting preventable diseases like HIV, tuberculosis, and malaria, the ramifications of reduced funding will be felt for years. Studies have shown that partnerships forged through USAID have added longevity and improved life quality for millions of people, highlighting how essential these programs are for public health advancements.
Strengthening Health Infrastructure Worldwide
To mitigate the adverse effects of USAID cuts, a concerted effort must be made to reinforce health infrastructure across developing nations. This can involve leveraging partnerships with local governments and organizations to sustain existing programs while innovating new strategies that can operate with limited resources. By investing in community health workers and local healthcare systems, countries can create long-term resilience against health emergencies. Supporting training programs and resources can ensure that communities are equipped with the necessary skills to respond effectively to health challenges.
Moreover, enhancing public health funding from diverse sources beyond government allocations can help fill the void left by USAID cuts. Initiatives such as crowdfunding for health projects or encouraging private sector investments can promote a more sustainable model of healthcare delivery. For the international community to step up, collaboration and collective action towards building health systems capacity will be vital. Countries must recognize that the strength of global health infrastructure not only depends on international aid but also on local engagement and resourcefulness.
The Role of Public Health Funding in Disease Prevention
Public health funding plays a critical role in preventing diseases and promoting health equity around the world. With the U.S. government reducing its contributions through agencies like USAID, the repercussions on public health programs can be deeply felt. For example, results from health interventions supported by USAID show that investments in vaccinations and disease prevention have substantial returns, leading to healthier populations and reduced healthcare costs in the long run. Programs financed by public health budgets are instrumental in providing timely health interventions, data collection, and mobilization of community health initiatives.
Moreover, the dwindling funding poses serious threats to ongoing preventive measures that have historically contributed to declines in maternal and child mortality rates. Without these funds, many groundbreaking initiatives aimed at ensuring access to essential medical care and education could falter, creating a disservice to vulnerable populations. Mobilizing diverse funding sources, including partnerships with NGOs and philanthropic organizations, can bring necessary resources back into the fold, reinforcing the importance of sustained financial commitments to uphold and enhance global health.
The Future of Global Health Leadership
As articulated by Atul Gawande, the future of global health leadership is uncertain, especially with the U.S. stepping back from its traditional role. Nonetheless, this transition presents an opportunity for other countries to step forward and bridge the gap left by American withdrawal. Emerging leaders from various nations may adopt innovative approaches to manage health crises and contribute to global public health efforts. For instance, countries that previously benefited from U.S. aid may step up to share knowledge, resources, and best practices within their regions.
This changing dynamic in global health leadership signals a potential shift toward a more decentralized and multi-faceted approach to health initiatives. Strengthening partnerships among countries and fostering regional cooperation can catalyze collective action against public health threats. The focus should be on collaborative governance where countries take ownership of health outcomes, ensuring an equitable distribution of resources and combating inequities experienced across different health systems.
Challenges Facing Health Infrastructure Today
The challenges that health infrastructure faces today are a direct result of political decisions and economic constraints. With USAID cutbacks, many countries are grappling with the collapse of crucial health services which previously provided necessary support to combat infectious diseases and health disparities. Decreased funding is linked to an increase in preventable diseases, reflecting a trend that could lead to health crises that exacerbate existing inequities among populations. It highlights the urgent need for strategic investment to reboot and sustain robust health systems.
Additionally, the depletion of resources has hindered the capabilities of healthcare providers who depend on external funds for training, technology, and research. The loss of personnel and expertise in public health sectors can create gaps in service provision and response to crises. By re-evaluating and restructuring current funding frameworks, it could be possible to stabilize health networks and invest in areas that have proven successful under previous programs, thereby safeguarding against future health emergencies.
Maintaining Momentum in Public Health Research
Despite the setbacks from reduced public health funding, there remains a significant opportunity to maintain momentum in public health research. Gawande’s experience illustrates the value of research in developing innovative health solutions, emphasizing that ongoing studies can significantly impact health outcomes. By drawing attention to the importance of funding research initiatives, stakeholders can advocate for resources that will lead to tangible health improvements. Ensuring a robust pipeline of research projects will foster new discoveries and enable a sustained response to health challenges.
Additionally, collaboration between academic institutions, public health entities, and private organizations is key to securing funding and driving research efforts effectively. Partnerships can lead to shared objectives, pooling resources in critical areas such as epidemiology and health technology. By leveraging different sectors, public health research can enhance its impact and effectiveness, reinforcing the importance of continuous investment even in uncertain times. The need for resilience and adaptability in research practices will ensure progress towards a healthier future.
Community Engagement in Global Health
Engaging communities in global health initiatives is essential, especially in times of funding cuts and systemic changes. As Gawande emphasized, health solutions are more effective when they are driven by local need and involvement. Public health professionals should focus on empowering communities to take charge of their health outcomes, cultivating environments where local knowledge enhances health interventions. This approach not only fosters ownership but also builds trust and cooperation among community members.
Moreover, fostering community engagement allows for a better understanding of specific health challenges and preferences, leading to tailored interventions that are culturally appropriate and effective. Active community participation can inform public health policies and prioritize resource allocation towards initiatives that resonate most with those served. As such, community engagement becomes a fundamental cornerstone for rebuilding health systems globally and ensuring that health interventions are responsive and effective.
The Significance of Global Health Partnerships
Global health partnerships have historically facilitated the sharing of resources and expertise, significantly enhancing the effectiveness of health initiatives. At a time when USAID has faced cuts, these partnerships can fill the void left in the international health arena. Collaborations between governments, NGOs, and private sectors can ensure that health services remain accessible and scalable, allowing for a more coordinated response to global health challenges.
Beyond immediate resource sharing, these partnerships create an ecosystem of collaboration that fosters innovation and encourages knowledge exchange. By aligning goals and sharing best practices, partners can tackle pressing health issues collaboratively, leading to sustainable improvements in health outcomes. As nations face similar health challenges, forming robust global health partnerships becomes imperative in ensuring collective resilience against public health threats.
Health Equity: A Global Mandate
Health equity is a pressing issue that requires a global mandate, particularly as funding for health initiatives fluctuates. Gawande’s insights highlight the dire consequences of inequitable health access, stressing that solutions must be designed to meet the needs of the most vulnerable populations. The cuts to USAID may disproportionately affect marginalized groups who rely heavily on public health programs for care and prevention, reinforcing existing disparities. Therefore, tackling health equity should be an integral part of any global health strategy moving forward.
Addressing health inequities means prioritizing investments in underserved communities, ensuring that essential services reach those who need them the most. Initiatives aimed at improving accessibility and affordability of care can lead to significant strides in fostering health equity both regionally and globally. It’s essential for governments and organizations to commit to equitable health policies that focus on removing barriers and eliminating disparities—an endeavor that is crucial for achieving sustainable global health.
Frequently Asked Questions
How have USAID cuts affected global health initiatives?
The cuts to USAID have significantly harmed global health initiatives by terminating over 85% of its programs. This dismantling has impacted vital health infrastructure, resulting in devastating consequences for millions of people worldwide, especially in areas like maternal and child health, disease surveillance, and emergency response.
What role does USAID play in global health leadership?
USAID has traditionally played a crucial role in global health leadership by funding medical research, improving health infrastructure in developing countries, and coordinating international health responses. The agency has built robust networks for disease surveillance and has been instrumental in addressing health crises more effectively.
What is the impact of recent funding cuts on public health funding worldwide?
Recent funding cuts to public health agencies, including USAID, threaten the continuity and effectiveness of global health programs. These reductions impact research initiatives and essential services that prevent diseases and improve health outcomes, thus jeopardizing the progress made in global health.
Why is global health infrastructure important for disease prevention?
A strong global health infrastructure is vital for disease prevention as it facilitates rapid response to outbreaks, supports immunization campaigns, and enhances health systems in vulnerable regions. USAID, for example, played a key role in reducing emergency response times and enhancing health systems globally.
What strategies are effective in enhancing vaccination rates in global health programs?
Effective strategies for enhancing vaccination rates in global health programs include providing technical assistance, ensuring vaccine availability, and community engagement. USAID has demonstrated that targeted support can move vaccination rates from 60% to 90%, illustrating the importance of strategic follow-through.
How can the global health community rebound after the USAID program cuts?
The global health community can rebound by advocating for restored funding, fostering partnerships with universities and research centers, and training a new generation of health leaders. Emphasizing the importance of science and healthcare innovation can also help in rebuilding health infrastructures weakened by the recent cuts.
What potential solutions exist for the challenges faced in global health due to funding cuts?
Potential solutions for overcoming challenges in global health include mobilizing private sector funding, fostering international collaborations, leveraging technology for health innovations, and increasing local capacity through education and training. These strategies can help mitigate the impact of reduced public funding.
What message does Atul Gawande convey about the future of global health?
Atul Gawande emphasizes that while the state of global health is concerning due to recent funding cuts, there is still hope. He encourages individuals in the health sector to remain committed to science and medicine, and acknowledges that, though the U.S. may retreat from its leadership role, other nations could rise to fill the gap.
| Key Point | Details |
|---|---|
| Dismantling of USAID | Gawande describes the serious consequences of the Trump administration’s cuts to USAID, highlighting that the agency has lost nearly all staff and over 85% of its programs. |
| Global Health Impact | The dismantling has caused ‘devastating’ damage to millions of people and undermined the U.S. role as a global health leader. |
| Urgency for Action | Gawande emphasizes that it is still possible to salvage health and science infrastructure and insists on the need to stop the destruction. |
| Research Funding Crisis | Federal programs supporting health and science have come under threat; this includes cuts to research funding for critical health issues. |
| Former USAID Achievements | Gawande praises USAID’s past role in building networks to combat diseases, improving health outcomes, and significantly reducing emergency response times for global outbreaks. |
| Hope for the Future | Despite challenges, Gawande expresses optimism about the future of global health and highlights the pivotal role that emerging leaders can play. |
Summary
Global health is facing unprecedented challenges due to severe cutbacks in funding and resources, particularly the dismantling of critical agencies like USAID. Atul Gawande’s insights reveal the significant ramifications this has had on global health initiatives and the well-being of millions worldwide. While the situation is dire, Gawande’s message encourages commitment to science and the importance of global health leadership from all nations. Immediate action is required to ensure the continuation of health programs that save lives, emphasizing collaboration, expert engagement, and a renewed focus on health infrastructure.
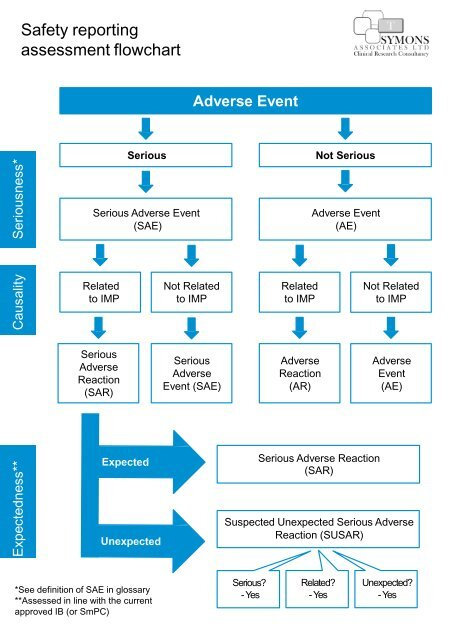
Medical Research Safety: Funding Cuts and Patient Impact
In the world of medical research safety, ensuring the well-being of patients is paramount. This field encompasses critical aspects such as patient safety in research and the ethical frameworks outlined by clinical research ethics to protect volunteers. Without robust IRB oversight, the rights of research participants could be compromised, leading to potential harm and ethical breaches. Additionally, the growing concerns about funding cuts impact on research threaten not only the integrity of studies but also the very safety mechanisms designed to uphold standards. Protecting research participants is not merely a regulatory requirement; it is a moral obligation that shapes the future of medical advancements.
Medical research safety, often referred to as participant protection in clinical studies, plays a vital role in healthcare advancement. This often includes ensuring that patient welfare is at the forefront of all research activities, guided by ethical standards and oversight from Institutional Review Boards (IRBs). The intricate balance between innovation and the rights of research subjects hinges on ethical considerations and rigorous monitoring systems. As financial support wanes, the ramifications extend beyond research outputs; they can erode public trust and confidence in the safety of medical trials. Therefore, upholding research integrity is essential not only for generating new treatments but also for maintaining community engagement and safeguarding participant rights.
The Impact of Funding Cuts on Patient Safety in Medical Research
At the forefront of medical research, patient safety is paramount. Recent funding cuts, particularly those impacting institutions like Harvard, significantly hamper the ability to conduct comprehensive reviews and oversight that protect patients involved in clinical trials. With over $2 billion in grants frozen, vital infrastructures, including Institutional Review Boards (IRBs), struggle to fulfill their mandate of ensuring patient safety. These cuts not only stall ongoing studies but also diminish the resources available for training and supporting the investigators who oversee patient care during the research.
Moreover, the repercussions of these funding interruptions extend beyond immediate research projects. A curtailed financial landscape can lead to a lack of innovative studies exploring groundbreaking therapies and interventions that could have long-term benefits for patient health. This situation creates a ripple effect, as delays in research can result in missed opportunities for developing new treatments, thus affecting the potential health outcomes for patients awaiting breakthroughs in medical science.
The Role of Institutional Review Boards (IRBs) in Safeguarding Research Participants
Institutional Review Boards (IRBs) are integral to the ecosystem of medical research, acting as guardians of ethical standards and patient safety. Their primary duty is to meticulously review research proposals, ensuring that every aspect—from the design and recruitment of participants to the consent process and risk assessment—is rigorously evaluated. The IRB’s function is critical, as it determines the ethical feasibility of studies before they commence, thus protecting individuals who volunteer for research. These boards help to mitigate potential harm and enhance the standards of clinical research ethics.
Additionally, IRBs play a proactive role in educating research teams about ethical practices and regulatory compliance. This helps create an environment where researchers are not only aware of the regulations but are also committed to the fundamental principles of patient safety and welfare. By fostering a culture of accountability and transparency, IRBs ensure that research participants are treated with respect and dignity while facilitating scientifically valid studies that can lead to significant advancements in healthcare.
Navigating the Ethical Challenges of Clinical Research
The landscape of clinical research is fraught with ethical challenges, particularly when it revolves around human participants. The historical precedents such as the Tuskegee Syphilis Study highlight the critical need for stringent ethical guidelines and oversight mechanisms. Today, ethical considerations are embedded in the research framework, with strict regulations designed to uphold the rights and welfare of research participants. The commitment to ethical standards is not just a legal obligation; it is a moral imperative that ensures trust in the research process.
Researchers and institutions must continuously engage with the ethical dilemmas posed by changing societal norms and scientific advancements. Each study poses unique challenges, from managing informed consent to balancing risks and benefits. The ongoing training and education provided through IRBs are essential in equipping researchers with the knowledge to navigate these complexities, ensuring they are prepared to handle ethical concerns responsibly and effectively.
The Interdependence of Research Funding and Patient Protection
The relationship between adequate research funding and the protection of patients cannot be overstated. Funding is crucial for not only initiating innovative studies but also sustaining the infrastructures that guarantee participant safety. When financial support wanes, it affects the full spectrum of research activities, often leading to compromised compliance with ethical standards and oversight. The resulting gap in resources can hinder IRBs from performing their critical function, ultimately jeopardizing patient protection in medical studies.
Moreover, when funding cuts occur, they can instill a climate of skepticism among participants, who may fear that a lack of oversight compromises their safety. The ethical principle of respect for persons is violated when individuals doubt the integrity of the research process. This can lead to unintended consequences, making it harder to recruit participants for future studies and diminishing the overall trust between the public and the research community.
Advancements in Patient Safety through Collaborative Research
Collaborative research efforts, facilitated by national frameworks like SMART IRB, aim to enhance patient safety through shared resources and expertise across multiple institutions. This cooperative model allows for streamlined oversight, enabling research teams to leverage diverse insights and experiences, which in turn bolsters protections for participants. By pooling resources, institutions can foster innovative studies that not only comply with rigorous ethical standards but also push the boundaries of scientific discovery.
In such collaborative environments, training and education on clinical research ethics are more effectively disseminated. Researchers from different institutions can share best practices and experiences related to patient safety, thereby improving the overall quality of clinical investigations. The collaborative framework empowers IRBs to operate more efficiently, ensuring that the rights and safety of research participants are universally prioritized across all participating sites.
The Future of Clinical Trials Amidst Funding Challenges
As funding challenges persist, the future of clinical trials faces uncertainty, particularly concerning the safety of research participants. The financial constraints leading to halted projects compromise the integrity and oversight necessary for protecting patients. Clinical trials designed to discover new treatments or evaluate existing therapies are critical components of medical advancement, and any disruption can have far-reaching effects on patient care and public health.
Looking ahead, it becomes imperative to advocate for sustainable funding models that prioritize patient safety without compromising the ethical standards of clinical research. Stakeholders must engage in discussions about the long-term implications of funding cuts and the necessity of maintaining robust oversight systems that protect research participants while allowing for scientific innovation. Ensuring that funding mechanisms support both the ethical conduct of research and patient safety is essential for fostering public trust in the medical research enterprise.
The Effect of Policy Changes on Research Oversight
Policy changes can have dramatic effects on research oversight, especially regarding funding and patient safety. Recent shifts in governmental approaches to research funding have raised concerns about the sustaining of robust oversight mechanisms crucial for protecting research participants. These changes not only directly impact the availability of resources for IRBs but also influence the regulatory environment that shapes clinical research practices, potentially leading to lapses in participant safety.
It is vital for the research community to remain vigilant and adaptive in the face of evolving policies. By continuing to advocate for the importance of IRB oversight and the ethical conduct of research, stakeholders can help ensure that patient safety remains a priority in medical research. Collaborating with policymakers to develop guidelines that support ethical practices and safeguard participant rights is essential for maintaining trust in research endeavors.
Building Public Trust in Clinical Research
Ensuring public trust in clinical research is a critical endeavor, particularly amidst funding cuts and shifting political landscapes. Trust is foundational to participant recruitment, as individuals are more likely to engage in studies when they feel assured of their safety and ethical treatment. Teaching communities about the role of ethics in research and the safeguards in place can enhance public confidence and foster greater participation in clinical trials.
Specific outreach efforts focused on explaining the importance of IRBs and the rigorous processes involved in safeguarding study participants can demystify clinical research. By actively engaging with the community, researchers can reinforce their commitment to ethical conduct and priorities, portraying a transparent image that builds rapport and trust. Ultimately, a collaborative relationship between researchers, participants, and the public is paramount for advancing medical research and ensuring participant protection.
The Long-Term Consequences of Disrupted Research
The long-term consequences of disrupted research due to funding cuts can be profound, not only for researchers but also for patients relying on new innovations. Delays in studies can lead to prolonged gaps in available therapies, impacting health outcomes for patients who could benefit from expedited research findings. As critical studies remain unfinished, patient health may stagnate, inhibiting progress in treating diseases and conditions that require immediate attention.
Furthermore, halted research projects can contribute to skepticism among the public regarding the reliability and integrity of clinical trials. If the perception of research is marred by funding issues, it can deter individuals from participating in studies and delay breakthroughs that could improve public health. Therefore, addressing this disruption is crucial not just for current research participants but for the overall advancement of healthcare and the medical field at large.
Frequently Asked Questions
What is the role of IRB oversight in ensuring patient safety in medical research?
Institutional Review Boards (IRBs) play a critical role in protecting patients involved in medical research. They review study proposals to ensure compliance with ethical standards, evaluate risks, and oversee the informed consent process. This oversight safeguards the rights and welfare of research participants, thereby enhancing overall patient safety in research.
How do funding cuts impact research participant protection in medical studies?
Funding cuts can severely undermine the mechanisms in place for research participant protection. Without sufficient resources, IRBs may struggle to maintain rigorous oversight, leading to lapses in patient safety protocols and potentially exposing participants to unmonitored risks in ongoing medical research.
What are the implications of federal research funding on clinical research ethics?
Federal research funding is essential for upholding clinical research ethics as it supports the functioning of IRBs, training of researchers, and monitoring of studies. A reduction in such funding can compromise ethical practices, jeopardizing patient safety and the integrity of clinical trials.
How does IRB oversight contribute to patient safety in multi-site medical research?
IRBs ensure patient safety in multi-site medical research by mandating a single IRB (sIRB) to oversee collaborative studies. This system streamlines ethical review processes, maintains consistent safety standards across all sites, and minimizes risks to research participants.
What historical events led to the establishment of current patient safety measures in medical research?
Historically significant events, such as the Tuskegee Syphilis Study and unethical experiments during World War II, highlighted the need for stringent ethical oversight in medical research. These events prompted the establishment of IRBs and regulations designed to protect patient safety in research.
How do IRBs ensure the safety of participants in clinical trials?
IRBs ensure safety by meticulously reviewing research methodologies, evaluating the risk-benefit ratio, overseeing informed consent, and monitoring ongoing studies for adverse events. This comprehensive review process is vital for the safety of participants in clinical trials.
What challenges arise from halted funding for patient safety initiatives in medical research?
Halted funding presents significant challenges for patient safety initiatives, including delays in research studies, lack of resources for IRB operations, and impaired ability to monitor compliance with ethical standards, all of which compromise the safety of research participants.
What is the SMART IRB system and how does it promote patient safety in research?
The SMART IRB system is designed to facilitate IRB oversight across multiple research sites. By allowing a single IRB to oversee studies, it promotes patient safety through streamlined evaluations and consistent application of ethical standards, ensuring better protection for research participants.
How does patient safety in research affect public trust in medical studies?
Patient safety in research is paramount for maintaining public trust. When research studies demonstrably protect participants and adhere to ethical standards, it fosters confidence among the community in the research process, ensuring ongoing collaboration and participation in future studies.
| Key Points | Details |
|---|---|
| Funding Freeze | The Trump administration froze over $2 billion in federal research funds to Harvard, impacting patient safety in medical research. |
| Role of IRBs | Institutional Review Boards (IRBs) review and oversee medical research to ensure participant safety and adherence to laws and ethics. |
| Impact of Cuts | Research funding cuts disrupt studies, risking participant safety, causing delays, and undermining public trust in research. |
| Historical Context | Historical abuses in medical research highlight the need for ethical oversight and the establishment of IRBs. |
| Ongoing Support | Despite funding cuts, Harvard Medical School is supporting the continuation of vital collaborative research efforts. |
Summary
Medical research safety is greatly threatened by funding cuts, as the halt in financial support disrupts essential oversight mechanisms like IRBs that protect patient welfare. Ensuring that adequate resources are available is critical to maintain ethical standards and to continue the vital work necessary to uphold the safety of participants in research studies.

CRISPR Gene Editing Ethics: A Deep Dive into Dilemmas
CRISPR gene editing ethics are at the forefront of modern scientific discourse, raising significant questions about the implications of gene editing technology on society. As this groundbreaking method promises potential cures for genetic disorders like sickle cell anemia, the ethical implications of CRISPR cannot be overlooked. With the ability to make germline gene modifications that could affect future generations, the conversation surrounding health equity in gene editing is becoming increasingly urgent. This technology’s power evokes a duality of hope and concern, prompting us to reconsider what it means to be human and the boundaries of medical intervention. Thus, as we explore the vast potential of CRISPR, it’s essential to balance innovation with responsible ethical frameworks.
The ethics surrounding CRISPR technology, often seen as a pivotal advancement in genetic engineering, invite a multitude of considerations. This revolutionary approach to gene editing presents the possibility of treating conditions like sickle cell disease, yet it simultaneously prompts a deeper examination of its societal impacts. The discussion around the moral responsibilities of gene manipulation, particularly regarding germline alterations, becomes vital as we ponder health disparities within access to these innovations. Furthermore, the dialogue on the consequences of such powerful tools emphasizes the need for a nuanced understanding of ethical boundaries in science. As we navigate this complex landscape, it becomes crucial to address the rights and responsibilities associated with altering human genetics.
Understanding the Promise of CRISPR Gene Editing Technology
CRISPR gene editing technology represents a significant leap forward in the realm of genetic medicine. With its ability to precisely alter DNA sequences, CRISPR provides a potential cure for genetic disorders such as sickle cell anemia. By using this innovative technology, scientists can modify somatic cells directly, thereby targeting diseases at their root. As we advance, it is crucial to grasp not only the scientific workings of CRISPR but also its implications for health outcomes. The potential to eradicate devastating conditions has led to widespread optimism, yet it simultaneously raises pressing questions about accessibility and equality in health treatment.
The excitement surrounding CRISPR is not solely about its capabilities—it also highlights the disparity in access to such pioneering gene editing technology. Currently, treatments like CRISPR for sickle cell anemia are exorbitantly priced, reportedly around $2.2 million per patient. This raises a fundamental concern: how do we ensure that life-saving gene therapies are available to everyone, regardless of socioeconomic status? Addressing this inequity is essential as we continue to explore the balance between innovation and justice in healthcare.
The Ethical Implications of CRISPR in Gene Editing
As CRISPR technology advances, it becomes vital to address the ethical implications that accompany its use. The questions surrounding the morality of gene editing are manifold. For instance, should we apply CRISPR to conditions that do not pose immediate life-threatening risks, such as Down syndrome? This introduces a slippery slope where the definition of what constitutes an acceptable genetic modification could vary drastically between individuals and cultures. Dr. Neal Baer emphasizes that as each edit is made, we must consider the consequences—both intended and unintended—on the fabric of our society and the essence of human diversity.
Adding to the ethical complexity is the concept of germline gene modifications, which allow changes to be heritable. This escalates the discussion from curative treatments to designer babies, which poses a profound ethical dilemma. Who should wield the power to select traits or enhance abilities in future generations? The debate underscores the need for a framework governing gene editing practices that emphasizes bioethics and social equity. Without such guidelines, we risk fostering a society where genetic enhancements deepen the existing divides among populations.
Health Equity and Gene Editing: A Critical Conversation
Health equity must be at the forefront of conversations about gene editing and CRISPR technology. While the scientific advancements offer hope for treating conditions like sickle cell anemia, the reality remains that access to these treatments is disproportionately skewed toward wealthier populations. As highlighted by Rebecca Weintraub Brendel, innovations often benefit those who already have resources, further widening the gap between different socio-economic groups. Addressing health equity means that as we progress in gene editing, we must advocate for policies that ensure fair access for all individuals, irrespective of their financial background.
Moreover, as CRISPR becomes more integrated into medical practice, it is vital that we consider how these technologies can be distributed fairly across diverse populations. Health justice is not merely about creating effective treatments; it also involves dismantling barriers that prevent marginalized communities from accessing these breakthroughs. In striving for health equity, it is essential to prioritize inclusive policies that allow everyone the chance to benefit from advancements in gene editing technology, thereby fostering a more just healthcare system.
The Future of Germline Gene Modifications
The prospect of germline gene modifications raises significant questions about the future of human evolution and the ethical boundaries of science. These modifications present an opportunity to eliminate genetic disorders at the embryonic stage, potentially leading to a healthier population. However, the implications of altering human DNA in ways that are inheritable stretch beyond medical ethics to the core of what it means to be human. As we contemplate the capabilities of CRISPR, we must consider who gets to decide the traits and characteristics deemed ‘desirable’ and how this power could be misused.
In light of these concerns, a robust regulatory framework is imperative to oversee germline modifications. Countries must come together to establish guidelines that prioritize ethical considerations, ensuring that gene editing does not lead to a society defined by genetic elitism. Ongoing discussions about the implications of CRISPR must include voices from diverse fields, including bioethics, sociology, and public policy, to create a holistic understanding of the impact of genetic technologies on humanity’s collective future.
The Economic Aspects of Gene Editing Treatments
The high costs associated with CRISPR treatments, such as those for sickle cell anemia, spark intense discussions about the economic implications of gene editing technology. With treatments nearing $2.2 million, it raises significant barriers to access, restricting availability primarily to affluent patients. This situation prompts questions about who will finance these therapies and how we can build a health system that does not leave vulnerable populations behind. As gene editing evolves, determining strategies for equitable distribution of treatments will be essential to maximizing its potential benefits.
Furthermore, the economic model for gene editing therapies must shift to ensure sustainability and accessibility. Investment in gene therapies should consider long-term health benefits over immediate profits. By creating policies that incentivize equitable access to innovative treatments, we can advance health equity while promoting the responsible use of technology. Collaboration between governments, healthcare providers, and pharmaceutical companies is crucial in establishing frameworks that support affordable gene editing solutions.
The Role of Oversight in CRISPR Implementation
As CRISPR technology becomes increasingly accessible, the importance of oversight cannot be overstated. Without proper regulatory mechanisms in place, there is a risk of unethical applications, such as germline editing without consent or for non-medical enhancements. Countries like China and Russia, which may operate outside stringent regulations, exemplify the ethical dangers of unmonitored gene editing. Hence, establishing a global consensus on ethical regulations and standards is essential to prevent misuse and protect the integrity of scientific advancements.
In light of potential abuses, continuous dialogue involving bioethicists, scientists, and legislators is critical to developing comprehensive oversight structures. These frameworks should not only safeguard against harmful practices but also promote transparency in gene editing applications. As we navigate these complex ethical waters, it is vital that we prioritize accountability to ensure that CRISPR technology serves the greater good and does not exacerbate existing societal issues.
Navigating the Unintended Consequences of Gene Editing
One of the most profound challenges with gene editing, particularly through CRISPR, is the unpredictability of unintended consequences. As scientists edit genes to alleviate specific health issues, there remains the potential for unforeseen side effects that could impact other genetic functions. For example, while reducing LDL cholesterol may seem beneficial, as highlighted by Dr. Baer, the interactions of genes are incredibly complex, and altering one aspect can have cascading effects throughout the individual’s health. This uncertainty necessitates caution and a deeper understanding of genetic interactions.
As we move forward with CRISPR, it’s vital to incorporate rigorous testing and ethical evaluation of gene editing outcomes. Researchers must prioritize transparency in their methods and findings to build public trust and confidence in these emerging technologies. By taking a cautious approach, we can explore the potential of gene editing while minimizing risks, ensuring that the benefits of CRISPR technology are maximized without compromising human health.
Cultural Perspectives on Human Genetics and Modifications
Cultural perceptions play a crucial role in the reception and application of gene editing technologies like CRISPR. Perspectives on genetic modifications differ significantly around the globe, influenced by societal values, religious beliefs, and historical contexts. For instance, some cultures may resist the idea of altering genetic traits, viewing it as a challenge to natural order, while others may embrace it as a pathway to innovation and progress. Understanding these diverse perspectives is essential as we navigate the ethical landscape of gene editing.
In order to foster responsible discourse on CRISPR and gene editing, it is crucial that we engage with various cultural contexts and their attitudes towards genetic manipulation. By fostering dialogues that include a multitude of voices, we can unpack the societal implications of gene editing technologies. This inclusivity will not only contribute to a more nuanced understanding of the ethical dilemmas at play but also facilitate collaboration that respects cultural diversity while advancing scientific knowledge.
Enhancing Public Understanding of CRISPR and Health Technology
To unlock the full potential of CRISPR and gene editing technology, enhancing public understanding is paramount. Many individuals lack in-depth knowledge of how these technologies work and their implications for health and society. Public education campaigns can help demystify the science behind gene editing and address common misconceptions while incorporating discussions about ethical considerations. By empowering people with knowledge, we not only foster informed dialogue but also promote informed consent in the medical arena.
Furthermore, active engagement between scientists, policymakers, and the community can lead to greater public understanding and trust in gene editing technologies. By presenting balanced information that encompasses both the benefits and risks associated with CRISPR, we can stimulate thoughtful conversations about its application in medicine. As we navigate these complexities, ensuring an informed public will be essential for the responsible deployment of gene editing technologies in the future.
Frequently Asked Questions
What are the ethical implications of CRISPR gene editing technology?
The ethical implications of CRISPR gene editing technology include concerns about health equity, as its benefits may not be accessible to all populations. This raises questions about who decides which traits are desirable, especially in cases like sickle cell anemia treatment. Furthermore, there are worries about the potential long-term effects of germline gene modifications and how they could affect future generations.
How does CRISPR gene editing impact health equity in treatment options for diseases like sickle cell anemia?
CRISPR gene editing has the potential to revolutionize treatment options for conditions like sickle cell anemia. However, the high cost of such treatments, which can exceed $2 million, creates a disparity in access, raising significant health equity concerns. This disparity could lead to an increased gap between those who can afford treatment and those who cannot.
What should we consider regarding germline gene modifications and their ethical implications?
Germline gene modifications can eradicate genetic diseases from future generations, but they also raise deep ethical concerns about ‘designer babies’ and parental control over traits. The question of who decides what traits to modify is complex and involves considerations of societal norms, disability rights, and the potential rise of genetic inequality.
Are there risks associated with the use of CRISPR gene editing for diseases that are compatible with life?
Yes, using CRISPR gene editing for diseases that are compatible with life raises ethical dilemmas. For instance, editing genes for conditions like Down syndrome sparks debate on whether it is humane to eliminate variations that contribute to the human experience. Each case requires thoughtful deliberation on the implications for individuals and society.
What oversight exists for CRISPR gene editing technologies, and why is it important?
While there are regulations against cloning and germline editing in many countries, the lack of international oversight allows practices that may not adhere to ethical standards, particularly in locations with lax regulations. This raises concerns about misuse, such as creating genetically altered individuals or populations with unforeseen consequences.
What are the unintended consequences of gene editing technologies like CRISPR?
Gene editing technologies such as CRISPR could lead to unintended consequences, including unforeseen interactions with other genes. For example, editing a gene that controls LDL cholesterol may have implications for insulin regulation and other vital bodily functions. The complex nature of genetic interactions demands careful consideration and thorough testing before any modifications are made.
| Key Points | Details |
|---|---|
| CRISPR’s Promise and Peril | Gene editing raises ethical questions about human alteration. |
| Curing Diseases | CRISPR can potentially cure conditions like sickle cell anemia. |
| Ethical Dilemmas | Questions arise about which diseases should be targeted and who decides. |
| Cost and Accessibility | Gene therapies can be extremely expensive, raising equity issues. |
| Parental Rights | Parents may want to genetically modify attributes of their children. |
| Oversight and Regulation | Concerns about the enforcement of laws prohibiting germline editing. |
| Unintended Consequences | Editing genes can have unexpected effects on other biological processes. |
Summary
CRISPR gene editing ethics are a crucial aspect of the ongoing debate over this revolutionary technology. The ability to edit genes offers promising cures for severe conditions like sickle cell anemia, but it also poses significant ethical dilemmas about human intervention. As we navigate this new frontier, it is essential to consider the socio-economic implications, potential misuse, and the inherent unpredictability of gene editing. In the quest for medical advancement, we must ensure we uphold ethical standards that respect human diversity and rights.
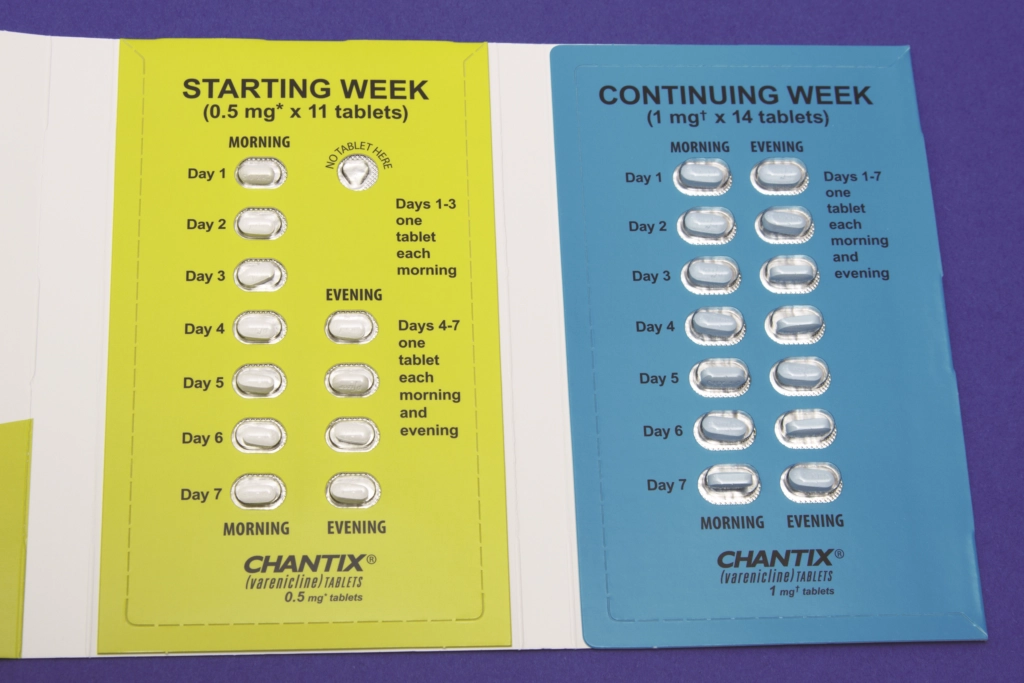
Smoking Cessation Pill Helps Teens Quit Vaping Effectively
The FDA-approved smoking cessation pill, varenicline, has emerged as a pivotal tool in addressing the escalating vaping epidemic among teens and young adults. A recent study published in JAMA highlights its effectiveness, showing that participants aged 16 to 25 who used varenicline were three times more successful at quitting vaping compared to those receiving only behavioral counseling. This groundbreaking research not only underscores the pressing need for effective cessation strategies but also reveals the potential of pharmacological treatments in combating nicotine addiction. With vaping becoming increasingly common, particularly among adolescents, understanding the success of varenicline could reshape the landscape of smoking cessation efforts. As we delve into the world of vaping cessation, it’s crucial to recognize how FDA-approved treatments like varenicline can significantly impact the lives of young nicotine users seeking to break free from their dependence.
In the realm of nicotine dependence, alternative solutions such as varenicline — a clinically endorsed pill for quitting smoking — are gaining widespread attention. Designed specifically for individuals struggling with the habit of vaping, this treatment shows promise in helping younger populations achieve lasting cessation. Research indicates that combining this medication with behavioral therapies yields remarkable results, especially among teenagers and young adults. As communities strive to find effective means to counter the viral rise of vaping, understanding the benefits of such FDA-sanctioned therapies becomes increasingly relevant. Addressing the addiction crisis among youths can pave the way for healthier futures, where quitting nicotine is a manageable milestone.
The Impact of Varenicline on Vaping Cessation
Varenicline, an FDA-approved smoking cessation pill, has demonstrated significant efficacy in helping teens and young adults overcome their vaping habits. In a recent clinical study, participants aged 16 to 25 who were prescribed varenicline were over three times more successful in quitting vaping when compared to those taking placebo. This highlights the potential for medication like varenicline to serve as a pivotal tool in addressing the growing issue of nicotine addiction among younger populations. By engaging in a structured treatment plan that includes behavioral counseling alongside medication, these individuals can tackle the psychological and physical challenges associated with quitting.
Moreover, the accessibility of varenicline for those as young as 16 expands the opportunities for effective intervention. Given the alarming rates of vaping among teens, with approximately 25% of young adults and 8% of high schoolers vaped recently, there is an urgent need for FDA-approved treatments like varenicline. These findings from Harvard-affiliated Mass General Brigham illuminate not only the success rates but also the overall safety of varenicline, as participants did not shift to traditional cigarette smoking post-treatment. This establishes varenicline as a cornerstone in the fight against youth nicotine addiction.
Understanding Vaping Trends Among Teens
The prevalence of vaping among teens is a pressing health issue that necessitates comprehensive strategies for cessation. Recent studies indicate that the popularity of vaping has surged, leading to a significant public health concern given its association with nicotine addiction and its potential to act as a gateway to more harmful substances. Vaping products, often perceived as safer than traditional cigarettes, still pose substantial risks, including exposure to carcinogens and heavy metals. Understanding the trends and patterns of vaping among youth is essential for developing targeted prevention and treatment initiatives.
Effective vaping cessation programs must engage with this demographic using relatable and impactful messaging. It is important for healthcare providers to discuss the realities of nicotine addiction and the long-term health consequences of vaping, as well as to promote evidence-based FDA-approved treatments. By informing young people about the resources available to them, such as varenicline, there is a better chance of altering the trajectory of nicotine use among future generations. Empowering teens with knowledge and medication options can make a significant difference in curbing the vaping epidemic.
Innovative Behavioral Support for Teens Quitting Vaping
In addition to pharmacological interventions, behavioral support is a fundamental component of successful vaping cessation among teens. The study conducted by Mass General Brigham incorporated weekly behavioral counseling alongside varenicline, reflecting an integrative approach to treatment. This combination allows young individuals to address the emotional and cognitive aspects of addiction while receiving medical support. Behavioral therapy provides crucial coping strategies and lifestyle changes necessary for long-term cessation, which can enhance the efficacy of medications like varenicline.
Utilizing services like ‘This is Quitting,’ a text-based support platform aimed at younger users, complements traditional counseling. By fostering a community of support through digital platforms, teens can voice their struggles and successes, ultimately feeling less isolated in their journey to quit. This dual approach not only promotes accountability but also reinforces the commitment to quit vaping, showing promising results in treatment efficacy among young adults. As this age group continues to face unique challenges, innovative support systems are key to overcoming nicotine dependence.
The Role of Public Health in Combating Vaping
Public health initiatives play a crucial role in addressing the vaping epidemic among teens. Educational campaigns aimed at raising awareness about the dangers of vaping and the availability of effective cessation tools such as varenicline are essential. These campaigns should be tailored to resonate with youth, employing platforms they frequently engage with, such as social media, to disseminate accurate and compelling information about vaping risks. By leveraging influencers and relatable content, public health messaging can work to shift perceptions of vaping from a benign activity to a serious health risk.
Furthermore, increasing access to cessation resources, including prescriptions for varenicline and behavioral support services, is fundamental in public health strategies. Targeted outreach to schools and community centers can help identify at-risk youth and provide them with the necessary tools to quit vaping. Collaborating with stakeholders, including healthcare providers and educators, can help create a supportive environment that fosters discussions around nicotine addiction and promotes healthier choices among adolescents. Community-driven initiatives not only empower youth but also contribute to a broader societal effort to reduce nicotine dependence.
Research Insights into Nicotine Addiction
Ongoing research into nicotine addiction is critical for understanding the dynamics of vaping and the effective methods for cessation. Studies like the one from Mass General Brigham are pioneering efforts to investigate the impacts of varenicline on young individuals, emphasizing the need for tailored interventions that address the unique health behaviors of teens. As data reveal more about the biological and psychological factors associated with nicotine dependency, healthcare professionals can refine treatment approaches, ensuring they meet the specific needs of adolescents battling against vaping.
Future research should also consider the long-term effects of vaping and the potential for dual addictions, particularly among teens who shift from vaping to traditional cigarettes. By examining the nuances of addiction trajectories and developing comprehensive treatment methodologies, healthcare providers can better assist young individuals in overcoming their dependencies. Collaboration between researchers, healthcare professionals, and policymakers is essential to inform best practices in vaping cessation and enhance the effectiveness of FDA-approved treatments like varenicline.
Addressing Safety Concerns in Vaping Treatment
While varenicline shows promise in helping teens quit vaping, it is essential to address concerns regarding safety and potential side effects. The recent study underscores that no participants who quit vaping transitioned to cigarette smoking, which is a critical outcome in evaluating the safety of varenicline. Monitoring participants during follow-ups allows researchers to assess not only the effectiveness of the treatment but also the overall health of the individuals involved. This vigilance is crucial as it helps ensure that innovative treatments do not introduce new risks.
Additionally, healthcare providers should communicate transparently about the safety profile of varenicline, reassuring teens and their caregivers of its low risk compared to other nicotine products. Strategies must also include thorough patient education on the importance of following prescribed guidelines and reporting any adverse effects. This approach fosters a culture of safety and trust, encouraging young individuals to seek help in their quitting journey while feeling supported by the healthcare system.
Community Engagement in Vaping Cessation Efforts
Community engagement plays a vital role in the effectiveness of vaping cessation programs, especially among teens. Involving local organizations, schools, and healthcare providers in outreach initiatives can create a robust support network for young people struggling with nicotine addiction. Community-driven programs can also facilitate workshops and informational sessions that educate families about the dangers of vaping and the tools available for cessation, including varenicline. By harnessing community resources, we can build a comprehensive framework that encourages collaboration and mutual support.
Moreover, peer-led initiatives can be particularly effective in combating vaping among teens. Programs that empower young leaders to educate their peers about the risks of vaping and share their cessation journeys can resonate more deeply than traditional methods. Through storytelling and shared experiences, teens can influence one another positively, creating an environment that prioritizes health over nicotine dependency. By placing youth at the forefront of prevention and cessation efforts, communities can enhance their effectiveness and inspire lasting behavioral change.
Cultural Factors Influencing Vaping Behavior
Understanding the cultural factors that influence vaping behavior among teens is crucial for developing effective interventions. Cultural narratives around vaping often depict it as a trendy and socially acceptable alternative to smoking, which can perpetuate its appeal to adolescents. By analyzing these cultural perceptions, public health professionals can craft messages that challenge these narratives and highlight the real health consequences associated with vaping. Effective communication strategies must resonate with the values and interests of teens, helping them see quitting as a desirable path.
Additionally, engaging cultural figures and influencers in these efforts can amplify the reach and impact of cessation campaigns. When peers and public figures openly discuss their own experiences with vaping, including struggles and successes in quitting, it can demystify the challenges of addiction and make the goal of cessation seem more attainable. Tailoring messages to reflect the diverse backgrounds and experiences of teens can help foster a more inclusive dialogue about vaping, ultimately encouraging a broader cultural shift away from nicotine dependence.
Future Directions in Vaping Research and Treatment
As vaping continues to evolve, future research must adapt to emerging trends and address the challenges of nicotine addiction among youths. Investigating the long-term effects of vaping on health, developing diverse cessation strategies, and exploring the efficacy of alternative treatments, alongside varenicline, are necessary areas of focus. The ongoing dialogue in the scientific community about vaping will enable us to understand better how addiction operates among evolving nicotine products and the best ways to combat it in younger populations.
Moreover, collaboration between researchers, clinicians, and public health officials is essential in translating study findings into actionable policies and practices. By leveraging insights gained from research, stakeholders can work together to enhance prevention efforts, increase access to cessation resources, and promote a unified message against vaping. The ultimate goal is to foster an environment where young individuals can make informed decisions about their health and be supported in their journey to quit nicotine entirely.
Frequently Asked Questions
What is the FDA-approved smoking cessation pill for quitting vaping?
The FDA-approved smoking cessation pill for quitting vaping is varenicline. It is designed to help individuals, including teens and young adults, to break their nicotine addiction effectively.
How effective is varenicline in helping young adults quit vaping?
Varenicline has shown to be highly effective in helping young adults quit vaping. Clinical studies indicate that participants who used varenicline were more than three times as likely to quit compared to those who received a placebo.
Can teens use varenicline as a smoking cessation pill?
Yes, teens aged 16 to 25 can use varenicline as a smoking cessation pill to help them quit vaping. It has been studied specifically for this vulnerable population and is deemed safe and effective.
What are the benefits of using varenicline for vaping cessation?
The benefits of using varenicline for vaping cessation include significantly higher success rates in quitting compared to other methods, the ability to reduce cravings, and a positive impact on health without leading to a switch to cigarette smoking.
Are there any side effects associated with varenicline as a smoking cessation pill?
While varenicline is generally safe for use, some individuals may experience side effects. It’s important for users to discuss these with their healthcare provider to manage any potential risks.
How does varenicline work to help people quit vaping?
Varenicline works by stimulating nicotine receptors in the brain, which helps reduce withdrawal symptoms and cravings associated with quitting nicotine. This dual-action approach aids in breaking the vaping habit more effectively.
Is behavioral counseling necessary when using varenicline for vaping cessation?
While varenicline can be effective on its own, combining it with behavioral counseling can enhance quitting success rates. The best results often come from a comprehensive treatment plan that includes both medication and counseling.
How long should someone take varenicline to quit vaping?
Typically, varenicline is prescribed for a period of 12 weeks, during which users receive support and monitoring to maximize their chances of quitting vaping successfully.
What is the success rate of varenicline for vaping cessation among young adults?
In clinical studies, about 51% of young adults using varenicline were able to stop vaping after 12 weeks, which is considerably higher than the success rates of those using placebo treatments.
What should I do if varenicline does not work for quitting vaping?
If varenicline does not work, it’s advisable to consult a healthcare provider for alternative treatment options or therapeutic approaches that may better suit your individual needs.
| Key Point | Details |
|---|---|
| FDA-approved Medication | Varenicline is the key smoking cessation pill, approved for adults but effective in teens 16-25. |
| Clinical Trial Success Rates | Participants taking varenicline were 3 times more likely to quit vaping than those with placebos (51% vs 14% at 12 weeks). |
| Behavioral Support | All groups received weekly counseling and access to the ‘This is Quitting’ text support service, highlighting the added importance of medication. |
| Vaping Among Youth | Approximately 25% of 18-25 year-olds and 8% of high schoolers were found to vape, underlining the critical need for effective smoking cessation tools. |
| Safety of Varenicline | The study concluded that varenicline was safe for use in the younger population without leading to a switch to cigarette smoking. |
Summary
The smoking cessation pill, varenicline, has proven to be a groundbreaking solution in aiding teens and young adults to quit vaping effectively. As highlighted in a recent clinical trial, this FDA-approved medication demonstrates significant success, with participants quitting at three times the rate of those using placebo treatments. With the alarming rise of vaping among youth, the findings underscore the urgent need for accessible, effective smoking cessation options. Varenicline not only facilitates quitting but does so safely, marking a vital step in addressing nicotine addiction within this vulnerable group.
Bile Imbalance and Liver Cancer: Key Insights Uncovered
Bile imbalance and liver cancer have become critical areas of research, particularly as studies highlight their intricate relationship. Recent findings indicate that an imbalance in bile acids, essential for fat digestion, can significantly escalate the risk of developing hepatocellular carcinoma (HCC), the most common form of liver cancer. By understanding the mechanisms behind bile acid metabolism and its regulation, particularly through the FXR receptor and the YAP signaling pathway, researchers are uncovering valuable insights that could revolutionize liver cancer treatment. This emerging connection between bile regulation and liver disease opens doors to innovative therapeutic interventions. As scientists continue to explore these pathways, they pave the way for potential strategies that could significantly impact patient outcomes in liver cancer care.
The disruption in bile acid equilibrium has emerged as a potential catalyst for severe liver conditions, intertwining with the pathology of liver malignancies. Investigating the role of bile acids in digestion reveals not only their digestive functions but also their hormonal regulation impact on liver health. Moreover, this field of study delves into the molecular underpinnings of liver cancer, especially focusing on key receptors and signaling pathways like FXR and YAP. Such insights are crucial, as they could lead to novel treatment modalities aimed at counteracting the effects of dysregulated bile functions. The implications of understanding this relationship underscore the need for continued research into liver disease and its treatment options.
Understanding Bile Imbalance and Its Link to Liver Cancer
Bile imbalance has emerged as a critical factor in the onset of liver cancer, particularly hepatocellular carcinoma (HCC). Bile acids, essential for fat digestion and metabolism, play an intricate role in maintaining liver health. When the production and regulation of these bile acids are disrupted, it can lead to an accumulation in the liver, causing inflammation and, ultimately, liver cancer. Recent studies have spotlighted how specific molecular pathways, notably the YAP signaling pathway, influence bile acid metabolism and contribute to these disease processes.
In examining the interplay between bile acid homeostasis and liver cancer, it becomes evident that the FXR receptor is crucial. FXR is a nuclear receptor that regulates bile acid synthesis and excretion. Dysregulation, particularly through the action of YAP, has been shown to paralyze FXR’s function, leading to the overproduction of bile acids. This overproduction can create a toxic environment in the liver, promoting fibrosis and increasing the risk for hepatocellular carcinoma. Thus, understanding and targeting these molecular switches may provide new avenues for liver cancer treatments.
The Role of YAP in Regulating Bile Acid Metabolism
YAP, or Yes-associated protein, has been identified as a key regulator in the signaling pathways that govern bile acid metabolism. According to recent research, YAP’s activation plays a dual role—while it is commonly associated with promoting cell growth, it simultaneously disrupts the bile acid regulatory mechanisms. By repressing FXR, YAP leads to an imbalance of bile acids that can escalate the risk of liver injuries and facilitate the progression to liver cancer. The duality of YAP’s role underscores the need for targeted therapies that can mitigate its effects in the liver.
Researchers are exploring pharmacological strategies to enhance FXR function, seeking to reverse the negative effects of YAP activation. Treatments that either activate FXR or inhibit YAP’s repressive activities could restore bile acid balance and prevent liver disease progression. Early experimental models demonstrate that such interventions may significantly reduce liver damage and inhibit the precursors of hepatocellular carcinoma. Investigating YAP’s role in this context not only broadens the understanding of liver cancer but also points towards innovative treatment methodologies that leverage the body’s regulatory mechanisms.
Potential Treatment Strategies for Liver Cancer Through Bile Acid Modulation
The growing body of research highlights the importance of targeting bile acid metabolism as a viable therapeutic approach for treating liver cancer. By modulating the FXR receptor activity, researchers can potentially influence liver cell functions and mitigate the effects of bile acid overload. Interventions that enhance FXR activity have shown promise in experimental settings, where they help restore balance in bile acid production and protect against liver damage. This pharmacological approach could pave the way for new liver cancer treatments that are less invasive and more effective.
Moreover, promoting the excretion of bile acids through targeted therapies offers another pathway to combat liver cancer. Enhancing the function of bile acid export proteins, like BSEP, could reduce bile acid accumulation in the liver and lower inflammation levels. These strategies show potential in not only treating existing liver diseases but also in preventing the onset of hepatocellular carcinoma by addressing the root cause—bile imbalance. As research continues, understanding these intricate relationships will be crucial in developing comprehensive treatment protocols for patients at risk of liver cancer.
The Importance of Nutrient Sensing in Liver Health
A pivotal aspect of liver health is its capability to sense nutrients and adjust its metabolic responses accordingly. This nutrient sensing is crucial for maintaining metabolic homeostasis, and when disrupted, it can lead to various liver-related diseases, including liver cancer. Recent advancements demonstrate the significance of cell signaling pathways in this process, particularly those mediated by YAP. As YAP not only influences cell growth but also plays a critical role in regulating bile acid metabolism, its dysregulation can have cascading effects on liver health.
Understanding how nutrient sensing affects liver function could lead to innovative strategies for maintaining liver health and preventing disease progression. By exploring the relationships between nutrient availability, bile acid metabolism, and liver signaling pathways, researchers aim to uncover targets for pharmacological interventions. This multifaceted approach can provide robust methods for enhancing liver vitality, developing preventative care and treatment plans tailored to individual metabolic profiles.
Exploring FXR as a Target for Liver Cancer Treatment
The Farnesoid X receptor (FXR) has emerged as a promising target in the fight against liver cancer due to its central role in regulating bile acid metabolism. FXR is integral in maintaining the balance of bile acids in the liver, and its dysfunction is closely associated with liver diseases. Recent studies underline the potential of FXR activation as a therapeutic mechanism to counteract the harmful effects of bile acid accumulation, which, if left unchecked, can lead to hepatocellular carcinoma.
By enhancing FXR function through various pharmacological agents, researchers hope to restore normal bile acid homeostasis and reduce liver fibrogenesis. This approach not only addresses the immediate issues of bile imbalance but also provides a long-term strategy to mitigate cancer risk. The pursuit of FXR-focused therapies exemplifies a shift towards targeted treatments that aim to refine metabolic control and improve liver health, ultimately impacting outcomes for patients at risk of liver cancer.
The Role of Cell Signaling in Liver Disease Progression
Cell signaling pathways play a fundamental role in the progression of liver diseases, particularly liver cancer. Pathways such as Hippo/YAP have been shown to regulate essential cellular processes, influencing growth and metabolism within the liver. Disruptions in these signaling cascades can lead to adverse effects on liver function and increased susceptibility to diseases such as hepatocellular carcinoma. Understanding these pathways provides crucial insights into the mechanisms underlying liver disease progression.
Research into cell signaling not only enhances our understanding of liver biology but also opens new avenues for therapeutic interventions. By identifying specific signaling proteins and their functions, scientists aim to develop targeted therapies that can interrupt the pathological processes involved in liver disease. Progress in this area could lead to innovative treatments that effectively combat liver cancer and enhance patient outcomes through more precise and tailored approaches.
Investigating the Interplay Between Bile Acids and Cancer Metabolism
The interplay between bile acids and cancer metabolism underscores the complexity of liver biology and the pathophysiology of liver cancer. Bile acids serve not only digestive functions but also influence metabolic pathways that can either promote or inhibit cancer progression. Recent findings suggest that an imbalance in bile acids can trigger metabolic switches that favor tumor development, particularly in the context of hepatocellular carcinoma. Understanding these dynamics is vital for developing effective treatment strategies.
By exploring how bile acids interact with cancer metabolism, researchers can identify novel therapeutic targets that may disrupt the tumor-promoting environments created by bile acid dysregulation. This multifaceted approach highlights the necessity of integrated research efforts that encompass both metabolic and cellular aspects of liver cancer, promoting a more comprehensive understanding of the disease and potential intervention strategies.
Future Directions in Liver Cancer Treatment Research
As the understanding of liver cancer mechanisms deepens, future directions in treatment research are becoming increasingly clear. The focus on bile acid metabolism and its regulation through pathways such as YAP and FXR represents a significant frontier in combating liver diseases. Researchers are now poised to investigate innovative drug formulations that target these pathways, which may lead to breakthroughs in therapeutic interventions. The promise of personalized medicine, based on individual metabolic profiles, could further enhance the efficacy of these treatments.
Continued collaboration between biologists, pharmacologists, and clinicians is essential to translate these laboratory findings into viable clinical treatments. As research progresses, the commitment to uncovering the links between bile imbalance and liver cancer will undoubtedly yield new strategies that can improve prognosis and quality of life for patients. With a focus on understanding the underlying molecular mechanisms, the future of liver cancer treatment appears promising, laying the groundwork for advanced therapies that tackle the disease at its root.
Frequently Asked Questions
What is the connection between bile imbalance and liver cancer?
A notable connection exists between bile imbalance and liver cancer, specifically hepatocellular carcinoma (HCC). Disruptions in bile acid production can lead to liver injury and inflammation, which are risk factors for HCC. The imbalance triggers responses that can result in tumor formation through mechanisms such as the Hippo/YAP signaling pathway.
How does bile acid metabolism relate to liver cancer treatment?
Bile acid metabolism is crucial in liver cancer treatment strategies. Research indicates that disturbances in bile acid levels may worsen liver conditions, including HCC. By targeting components like the FXR receptor to restore bile acid balance, new therapeutic options may emerge that can inhibit cancer progression and improve liver health.
What role does the FXR receptor play in hepatocellular carcinoma?
The FXR receptor is vital for maintaining bile acid homeostasis. In the context of hepatocellular carcinoma, FXR dysfunction—often caused by YAP signaling—can lead to increased bile acid production that contributes to liver fibrosis and cancer. Therapies aimed at enhancing FXR function may provide new avenues for liver cancer treatment.
Can YAP signaling pathway influence bile imbalance and liver cancer development?
Yes, the YAP signaling pathway significantly influences bile imbalance and liver cancer development. YAP has been found to act as a repressor of FXR, which disrupts bile acid metabolism. This disruption can lead to an overproduction of bile acids, inflammation, and ultimately the onset of hepatocellular carcinoma.
What are the potential pharmacological solutions for liver cancer related to bile imbalance?
Potential pharmacological solutions for liver cancer related to bile imbalance include drugs that enhance FXR function, inhibit YAP’s repressive role, or promote bile acid excretion. Targeting these pathways may halt the detrimental cycle of bile acid accumulation, reducing liver damage and cancer progression.
How does liver cancer treatment focus on bile acid metabolism?
Liver cancer treatment increasingly focuses on bile acid metabolism because imbalances can aggravate liver disease. By manipulating bile acid levels and ensuring proper metabolism through mechanisms involving FXR and YAP, researchers hope to develop targeted therapies that mitigate liver cancer progression.
What is the significance of the research on bile imbalance and liver cancer?
The significance of recent research on bile imbalance and liver cancer lies in the identification of molecular pathways that link bile acid dysregulation to tumor development. Understanding these connections can inform novel treatment strategies aimed at restoring bile acid homeostasis and potentially preventing or managing hepatocellular carcinoma.
| Key Points |
|---|
| Bile Imbalance and Liver Cancer |
| Bile acids are essential for fat digestion and regulate metabolic processes. |
| Disruption in bile acid regulation can lead to liver diseases, particularly hepatocellular carcinoma (HCC). |
| The Hippo/YAP signaling pathway plays a crucial role in bile acid metabolism and liver cancer progression. |
| YAP activates at FXR, disrupting bile acid homeostasis causing liver inflammation and fibrosis. |
| Targeting YAP activity or enhancing FXR could provide new treatment avenues for liver cancer. |
Summary
Bile imbalance is closely linked to liver cancer, particularly hepatocellular carcinoma (HCC). Recent research has identified critical pathways involved in bile acid regulation, which are essential for maintaining liver health. Disruptions in these processes can lead to liver injury and cancer progression. By focusing on the YAP pathway and its interaction with bile acid metabolism, new therapeutic strategies can be developed to prevent or treat liver cancer effectively.