Gene Editing Breakthroughs Revolutionize Disease Treatment
Gene editing breakthroughs have opened new frontiers in the field of medicine, revolutionizing our approach to genetic diseases and therapies. With advancements such as CRISPR technology reshaping our understanding of DNA manipulation, techniques like base editing and prime editing have emerged as powerful tools in this genetic revolution. These innovative approaches enable scientists to precisely alter the genetic code, offering hope for those affected by inherited disorders. As many as hundreds of millions of individuals worldwide grapple with genetic conditions, these advancements promise not only effective treatments but also a potential pathway to cures that were once thought impossible. With ongoing clinical trials demonstrating the efficacy of these gene editing methods, the future of gene therapy shines brighter than ever.
Recent innovations in DNA modification techniques are redefining the landscape of medical science and patient care. Terms like genome editing and genetic manipulation have gained prominence, reflecting the transformative power of novel therapies aimed at correcting mutations that lead to illnesses. The rise of techniques like base editing and prime editing represents significant strides in our fight against genetic disorders, enabling precise corrections at the molecular level. By utilizing advanced methodologies derived from CRISPR technology, researchers are forging pathways to groundbreaking treatments for a multitude of genetic diseases. These advancements not only promise to alleviate suffering but also highlight the vibrant possibilities of gene therapy in reshaping our health narratives.
The Impact of Gene Editing Breakthroughs on Cancer Treatment
Gene editing breakthroughs are revolutionizing the landscape of medical treatments, particularly in oncology. A striking example is the case of Alyssa Tapley, whose life was transformed by a clinical trial using base editing, a novel gene-editing technology developed by David Liu and his team. By targeting specific mutations that drive her T-cell leukemia, base editing has demonstrated how precise genetic corrections can lead to significant improvements in patient outcomes. This paradigm shift in cancer care is a testament to how gene editing can intervene effectively where traditional therapies may fall short.
As research continues to evolve, the application of base editing and other innovations like prime editing is showing promise not only in treating cancer but also in addressing a range of genetic diseases. With clinical trials underway, multiple patients have already experienced the life-changing benefits of these advanced gene therapies. The implications for public health are vast, with millions suffering from conditions previously deemed incurable now seeing hope through these cutting-edge techniques. This connection between innovative science and tangible health improvements is a beacon for the future.
The Role of CRISPR Technology in Modern Genetics
CRISPR technology has emerged as a groundbreaking tool in modern genetics, fundamentally altering our ability to study and edit genes. Initially discovered as a bacterial defense mechanism, CRISPR has rapidly transitioned into a versatile platform for gene editing, paving the way for revolutionary therapies in genetic disorders and cancers. The simplicity and efficiency of CRISPR have enabled researchers to conduct precise genetic modifications, fostering advancements like base editing and prime editing, which target specific DNA sequences without the need for more invasive techniques.
Moreover, the impact of CRISPR extends beyond basic research; it has catalyzed a surge in clinical applications aimed at correcting genetic diseases at their source. By harnessing the potential of this technology, scientists can now focus on creating targeted therapies that correct mutations responsible for hereditary conditions. Even as ethical debates surrounding gene editing practices intensify, the potential benefits of CRISPR technology in the realm of therapeutics remain compelling, marking a new era in our approach to genetic health.
Advancements in Base and Prime Editing Techniques
Base editing represents one of the most significant advancements in gene editing technologies, allowing scientists to make precise, single-base substitutions in DNA without causing double-stranded breaks. Developed by Liu’s team, base editing corrects mutations at their source, addressing the very foundation of genetic disorders. By focusing on the nucleobases—adenine, cytosine, guanine, and thymine—base editing holds promise for treating a variety of genetic diseases caused by common point mutations, thus enhancing the potential for personalized medicine.
On the other hand, prime editing takes precision a step further, functioning akin to a word processor that can not only modify existing gene sequences but also insert and delete DNA sequences. This nuanced approach allows for complex genetic corrections that were previously unattainable, showcasing a future where gene therapy can be tailored to individual patients’ needs. As ongoing clinical trials include these editing strategies, the landscape of genetic therapy is poised for expansion, potentially eradicating diseases that have plagued families for generations.
Gene Therapy: Transforming Lives with Innovative Treatments
Gene therapy has evolved from experimental treatments to a revolutionary approach in healthcare, providing hope for patients with chronic genetic conditions. By directly altering the genetic structure responsible for a disease, such therapies can restore normal function or even cure genetic disorders. The development of base editing and other gene editing technologies has accelerated this transformation, enabling tailored interventions that precisely address the underlying causes of conditions like hemophilia and cystic fibrosis.
The impact of such therapies is profound, as evidenced by personal stories like that of Alyssa Tapley, who went from a cancer diagnosis to being free from her disease thanks to innovative gene editing techniques. As these therapies advance, they not only promise to alleviate suffering but also shift the paradigm of how medical science approaches chronic illnesses, focusing on prevention and correction rather than mere symptom management. The potential to improve the quality of life for millions speaks to the importance of continued investment in genetic research and development.
The Future of Genetic Research and Innovation
As the field of genetics continues to evolve, the future of genetic research holds exciting potential for breakthroughs that could redefine our understanding of medicine. With pioneers like David Liu leading the charge, innovative technologies like CRISPR, base editing, and prime editing are at the forefront of this scientific revolution. These advancements not only enhance our ability to treat complex diseases but also challenge our ethical frameworks and regulatory approaches to gene editing applications.
Moreover, as we look to the future, fostering collaboration between academia, industry, and government agencies will be crucial for leveraging these innovations responsibly. Liu’s emphasis on the interconnectedness of basic science and clinical application underscores the need for a solid foundation in research that ultimately translates into meaningful patient outcomes. With continued investment and support, the next decade could witness transformative progress in our ability to combat genetic diseases and improve health on a global scale.
Ethical Considerations in Gene Editing
While the advancements in gene editing technologies present promising pathways for medical intervention, they also raise critical ethical questions that demand careful consideration. As scientists navigate the implications of editing human DNA, issues surrounding consent, equity, and the potential for unintended consequences come to the forefront. The responsibility falls on researchers to engage in dialogue with the public, policymakers, and ethicists to establish guidelines that ensure ethical practices in deploying these powerful tools.
Furthermore, the possibility of heritable gene edits amplifies these concerns, as modifications could be passed down through generations. This prospect necessitates a robust regulatory framework to mitigate risks and protect future generations. As we embrace the capabilities of gene editing, the integration of ethical considerations into research and clinical practices will play a pivotal role in shaping the responsible advancement of this field.
Understanding Genetic Diseases: The Role of Genetic Research
Genetic diseases affect millions of individuals worldwide, presenting formidable challenges for healthcare systems. Understanding the mechanisms behind genetic conditions is essential for developing effective treatments and preventive strategies. Ongoing research delves into the genetic underpinnings of these diseases, revealing the mutations and environmental factors that contribute to their manifestation. Breaking down the complexity of genetic disorders equips researchers and practitioners with the knowledge needed to craft targeted therapies.
With technologies like CRISPR, base editing, and prime editing leading the charge, the promise of correcting genetic mutations offers hope to those affected by chronic conditions. As scientists unlock the mysteries of the human genome, personalized medicine becomes increasingly achievable, paving the way for bespoke treatments that directly address the genetic root causes of diseases. The future of genetic research not only holds potential for cures but also fosters greater understanding and empathy towards those grappling with these often misunderstood ailments.
Clinical Trials: A New Era of Treatment Opportunities
Clinical trials are essential in bridging the gap between scientific discovery and practical application in medicine. The rise of gene editing technologies has catalyzed a remarkable expansion of clinical trials aimed at testing innovative therapies for genetic diseases. This new era of treatment opportunities empowers patients who have limited options, providing them access to cutting-edge interventions that could dramatically change their health outcomes. With dozens of patients already treated in ongoing studies of base editing and prime editing, the hope for life-improving therapies proliferates.
Participating in clinical trials also contributes to a larger understanding of gene therapies’ safety and efficacy. The data generated from these trials is invaluable in informing future research directions and regulatory decisions. As the landscape of clinical trials evolves, it is crucial to prioritize patient safety while accelerating the timeline for bringing effective treatments to market. This balance of innovation and caution defines the current trajectory of gene therapy research and highlights the importance of ethical practices in clinical settings.
The Importance of Basic Science in Advancing Genetic Research
The foundation of many scientific breakthroughs lies in basic science, which seeks to illuminate the underlying principles of biological phenomena without immediate practical applications. This essence of curiosity-driven research has played a crucial role in the development of gene editing technologies. Liu’s work at the Broad Institute exemplifies this approach, showing how fundamental investigations into bacterial immune mechanisms can lead to revolutionary therapeutic tools like CRISPR, base editing, and prime editing.
Investing in basic science not only fosters innovation but also inspires future generations of scientists to explore the unknown. The findings from such research serve as a catalyst for applied science that directly benefits society, particularly in healthcare. As we continue to embrace the interconnectedness of basic and applied research, the potential for transformative advancements in our understanding of genetics and medicine will only expand.
Frequently Asked Questions
What are some recent breakthroughs in gene editing technology?
Recent breakthroughs in gene editing technology include advancements in base editing and prime editing. Base editing allows for precise changes to the four nucleotide bases of DNA, targeting common mutations responsible for genetic diseases. Prime editing, on the other hand, functions like a word processor, enabling researchers to correct a wider variety of genetic errors, potentially offering solutions for previously untreatable conditions.
How does CRISPR technology relate to gene editing breakthroughs?
CRISPR technology is foundational to many gene editing breakthroughs. Developed from a bacterial immune system, CRISPR allows scientists to cut DNA at specific locations. Recent innovations like base editing and prime editing build on CRISPR principles, providing more precise methods for correcting mutations associated with genetic diseases, thereby enhancing the efficiency and safety of gene therapies.
What is base editing and how does it contribute to gene therapy?
Base editing is a novel gene editing technique that allows scientists to directly convert one DNA base into another, which is pivotal for correcting specific mutations that cause genetic diseases. Since it operates without causing double-strand breaks in DNA, it offers a safer alternative to traditional CRISPR techniques, making it a valuable tool in gene therapy and the search for cures.
What role do prime editors play in treating genetic diseases?
Prime editors play a crucial role in treating genetic diseases by allowing precise editing of DNA sequences at single letter changes or inserting/deleting letters. This advanced gene editing technology enables researchers to target more complex mutations that traditional methods cannot easily address, thus broadening the horizon for effective gene therapies.
How are clinical trials leveraging gene editing breakthroughs?
Clinical trials are utilizing gene editing breakthroughs such as base editing and prime editing to develop new treatments for various genetic disorders. These trials are currently testing the safety and efficacy of these innovative technologies in patients, indicating a significant step forward in gene therapy methods for treating illnesses that were previously deemed untreatable.
In what ways does gene editing technology aim to address genetic diseases?
Gene editing technology aims to address genetic diseases by targeting and correcting mutations within DNA that cause these conditions. Using techniques like CRISPR, base editing, and prime editing, researchers strive to restore normal gene function, ultimately improving patient outcomes and potentially curing diseases that affect millions of people worldwide.
What are the limitations of CRISPR technology compared to recent gene editing breakthroughs?
While CRISPR technology has revolutionized gene editing, its limitations include unintended off-target effects and difficulties in making precise corrections. Newer breakthroughs such as base editing and prime editing overcome some of these challenges by enabling more accurate and safer modifications to DNA without causing double-strand breaks, potentially leading to more effective treatments for genetic diseases.
| Key Points | Details |
|---|---|
| Breakthrough in Gene Editing | Base editing technology successfully cleared T-cell leukemia in a 13-year-old patient, marking a significant advance in gene editing. |
| David Liu’s Role | David Liu developed base editing, a safer and more precise alternative to CRISPR, addressing limitations in correcting genetic mutations, |
| Base Editing | Base editing modifies single DNA bases (A, T, C, G) to correct common mutations causing diseases. |
| Prime Editing | Prime editors can correct a variety of genetic errors by replacing flawed DNA with corrected sequences, similar to a word processor. |
| Current Clinical Trials | As of now, there are at least 18 clinical trials utilizing base and prime editing technologies. |
| Long-Term Impact | Research stemming from basic science has led to aspirations of correcting genetic diseases effectively. |
| Challenges Ahead | Concerns regarding the relationship between academia and government may hinder the progression of future scientific innovations. |
Summary
Gene editing breakthroughs have fundamentally changed the landscape of genetic medicine. In recent years, advancements such as base editing and prime editing have emerged from pioneering research, especially by scientists like David Liu. These innovative techniques not only offer safer, more precise methods for correcting genetic mutations that lead to diseases but also reflect the crucial need for continued support of basic science. As promising clinical trials continue to develop, the potential for these breakthroughs to transform healthcare and provide hope for patients suffering from genetic disorders is more apparent than ever.
Maternal Mortality in the U.S.: A Growing Concern
Maternal mortality in the U.S. has become an alarming public health crisis, with recent studies indicating a rise in pregnancy-related deaths that continues to outpace other high-income countries. Shockingly, over 80 percent of these deaths are deemed preventable, highlighting significant gaps in maternal healthcare. Disparities in maternal health outcomes across states and racial groups only exacerbate the issue, as American Indian and Alaska Native women experience markedly higher mortality rates than their white counterparts. The implications of high maternal mortality rates extend beyond pregnancy, affecting postpartum care and overall maternal health disparities in the nation. As we delve into this pressing topic, it becomes crucial to identify effective strategies to combat preventable maternal deaths and enhance care during and after pregnancy.
The rising rates of maternal fatalities in the United States pose a serious challenge for public health, raising concerns about the safety and efficacy of pregnancy and childbirth experiences. With a significant portion of pregnancy-related deaths classified as avoidable, the focus is increasingly on improving healthcare systems and support during and after delivery. Many women face elevated risks due to various factors, including socioeconomic disparities and inadequate access to quality care, particularly during the postpartum phase. This troubling trend calls for a thorough examination of maternal health conditions and the immediate need for interventions to curb the surge in these tragic outcomes. Understanding how social determinants impact maternal well-being is vital for developing comprehensive solutions to intervene in this growing crisis.
Understanding Maternal Mortality Rates in the U.S.
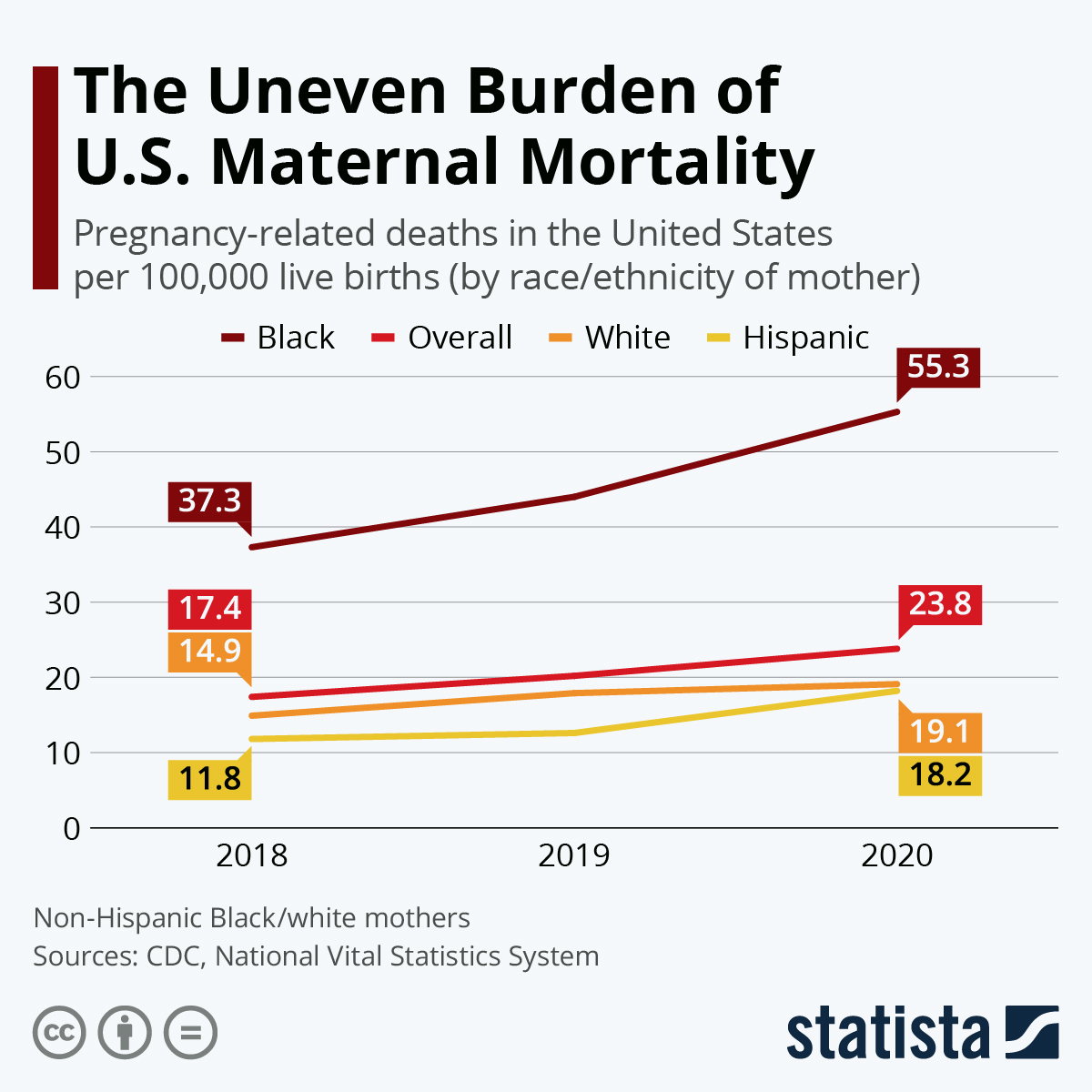
Maternal mortality in the U.S. remains a pressing public health issue, with pregnancy-related deaths significantly surpassing those in other high-income nations. A recent study indicates that about 80 percent of these deaths are preventable, emphasizing the critical need for improved healthcare during and after pregnancy. The U.S. recorded 32.6 maternal deaths per 100,000 live births in 2022, marking a stark increase from 25.3 in 2018, reflecting not just a troubling trend, but an urgent call for systemic change. Policy reform aimed at equitable healthcare access is crucial to reducing these mortality rates, particularly for disadvantaged population groups who face higher risks based on race and geography.
The rise in maternal mortality is characterized by stark disparities; American Indian and Alaska Native women, for instance, experience mortality rates nearly four times higher than their white counterparts. This suggests that maternal health disparities are deeply rooted in social determinants, such as income, education, and access to quality healthcare services. Effective policy changes must address these variances, fostering an environment where all women receive essential prenatal and postpartum care to mitigate risks associated with pregnancy-related deaths.
The Importance of Postpartum Care in Maternal Health
Postpartum care is an often-overlooked aspect of maternal health that has a profound impact on long-term wellness for new mothers. The U.S. healthcare system traditionally emphasizes the immediate post-birth recovery period, often neglecting a more extended approach to postpartum care. However, findings indicate that a significant proportion of pregnancy-related deaths occur in the months following childbirth, highlighting the necessity of comprehensive services that extend beyond the initial six weeks. This shift from reactive to proactive healthcare measures could drastically lower rates of preventable maternal deaths.
Holistic postpartum care should include mental health support, management of pre-existing conditions, and education about warning signs that could avert complications. With late maternal deaths accounting for nearly a third of total pregnancy-related fatalities, it is crucial to recognize that recovery does not end at the hospital discharge. By adopting a more inclusive and longitudinal approach to maternal care, healthcare providers can better address the complexities of maternal health, ultimately leading to improved outcomes and quality of life for mothers.
Factors Contributing to Preventable Maternal Deaths
Preventable maternal deaths highlight systemic issues within the U.S. healthcare landscape, marked by inequitable access to care, particularly for marginalized communities. The findings from recent studies suggest that many contributing factors such as chronic health conditions, a lack of affordable insurance, and inadequate prenatal care lead to high maternal mortality rates. Additionally, the COVID-19 pandemic has exacerbated these issues, as many hospitals faced capacity challenges while healthcare access became constrained. Addressing these barriers is essential to reducing preventable deaths.
Moreover, social determinants of health play a crucial role in these disparities. Economic instability, educational inequities, and systemic racism contribute to the heightened risks faced by women of color and those living in rural areas. Comprehensive public health strategies that advocate for policy changes, improved insurance coverage, and access to high-quality maternal services are necessary to combat these preventable deaths. The implementation of better tracking systems for maternal health outcomes can also lead to enhanced monitoring, informing strategies for reducing pregnancy-related deaths.
Addressing Maternal Health Disparities Across Racial Lines
Maternal health disparities are starkly evident, with significant differences based on race and ethnicity. American Indian and Alaska Native women experience the highest mortality rates, while non-Hispanic Black women also face disproportionately high rates compared to white women. These disparities suggest deep-rooted societal issues, including discrimination and inequities in healthcare access and quality. Efforts to diversify healthcare policy and increase representation within the medical community are critical to addressing these disparities.
To diminish these gaps, there must be an emphasis on culturally competent care that acknowledges and addresses the unique needs of diverse racial populations. This includes implementing community-based interventions that focus on education, access to prenatal and postpartum care, and outreach programs designed to connect underserved populations with the resources they need. Government initiatives should also support research aimed at understanding these disparities to inform effective policy changes and drive health equity across all demographics.
The Role of Chronic Conditions in Maternal Mortality
Chronic health conditions are emerging as significant contributors to maternal mortality rates in the U.S. Recent studies have shown an alarming trend: younger women are increasingly at risk of developing conditions like hypertension, which have traditionally impacted older demographics. The rise in chronic diseases among pregnant individuals can be attributed to various factors, including lifestyle changes and systemic inequalities in healthcare access, which require urgent attention.
Addressing chronic conditions within maternal healthcare requires a multi-tiered approach, including education, early screening, and tailored management strategies. Ensuring continuous monitoring of medical conditions prior to and throughout pregnancy could significantly reduce risks. Additionally, healthcare systems must prioritize preventative care and implement integrated health strategies that allow for comprehensive management of chronic illnesses, which in turn can lower rates of maternal mortality and improve overall pregnancy outcomes.
The Impact of State-Level Variations on Maternal Health Outcomes
State-level variations in maternal health outcomes pose significant challenges to achieving nationwide improvements in maternal mortality rates. The disparities illustrate how healthcare access, quality, and policies can differ drastically across the U.S., leading to better outcomes in some regions, notably California, which serves as a benchmark for effective maternal health strategies. Understanding these differences can guide targeted interventions tailored to each state’s unique challenges.
High maternal mortality rates in certain states point to systemic issues such as limited access to prenatal care, varying healthcare policies, and differences in public health funding. Addressing these issues at the policy level is vital to establishing a more equitable healthcare system. State governments must commit to improving maternal health by investing in supportive services for expectant mothers and by adopting best practices shared among states with successful outcomes, ultimately striving for a unified approach to maternal health challenges.
Innovations Needed in Maternity Care Systems
Innovation in maternity care is essential for addressing the high rates of preventable maternal deaths in the U.S. Current healthcare systems often lack the flexibility and resources needed to provide comprehensive care throughout the entire pregnancy and postpartum period. By investing in new models of care that prioritize continuity and communications among caregivers, maternal health outcomes could see significant improvement. Programs that emphasize team-based approaches involving obstetricians, midwives, and maternal-fetal specialists have been shown to enhance care quality and reduce complications.
Emerging technology also presents new opportunities for monitoring maternal health, such as telehealth services that allow for remote consultations and continuous health monitoring. The integration of such technologies can bridge gaps in care for women living in rural or underserved urban areas, providing them with timely interventions and support. As these innovations are implemented, ongoing evaluation and research must continue to gauge their effectiveness in improving maternal healthcare and address areas requiring further reform.
The Long-Term Consequences of Maternal Mortality
The impact of maternal mortality extends beyond the individual mother; it has lasting consequences for families and communities. The loss of a mother can lead to severe emotional and financial hardships, affecting children’s stability and well-being. Additionally, communities face broader socio-economic implications with increased healthcare costs and loss of productivity when mothers die preventably. Acknowledging the ripple effects of maternal mortality emphasizes the urgent need to prioritize maternal health within public health agendas.
Moreover, the societal undervaluation of maternal health often results in insufficient investment in programs aimed at preventing maternal deaths. Such neglect compromises not only the health of mothers but also the development and health of the next generation. Initiatives focused on improving maternal health must be framed within a broader context of family and community health, advocating for integrated policies that emphasize family well-being, reproductive health, and generational health outcomes.
Systemic Changes for Improving Maternal Health
Addressing the high maternal mortality rates in the U.S. necessitates systemic changes within healthcare systems. To effectively combat the prevalence of pregnancy-related deaths, investments in public health infrastructure are paramount. Funding cuts that target maternal health compromise the ability to monitor outcomes, track disparities, and implement effective interventions. It is essential for policymakers to recognize the need for sustained investment in maternal healthcare as a crucial area of public health.
Moreover, systemic changes should include increasing awareness and training regarding the unique healthcare needs of pregnant and postpartum individuals among healthcare providers. Continuous education on potential risks and up-to-date practices can empower healthcare professionals to deliver timely and effective care. Supporting initiatives that focus on reducing bias and improving communication between providers and patients can also foster a more supportive environment, ultimately leading to better maternal health outcomes.
Frequently Asked Questions
What is contributing to the high maternal mortality rates in the U.S.?
High maternal mortality rates in the U.S. are attributed to a combination of factors, including an inequitable healthcare system, lack of access to quality prenatal care, and systemic biases that affect maternal health across different racial and ethnic groups.
How do maternal health disparities impact pregnancy-related deaths in the U.S.?
Maternal health disparities significantly impact pregnancy-related deaths in the U.S. For instance, American Indian and Alaska Native women face the highest mortality rates, highlighting the urgent need to address these inequities through targeted healthcare policies and improved access to care.
What role does postpartum care play in preventing maternal mortality?
Postpartum care is crucial in preventing maternal mortality, as nearly one-third of pregnancy-related deaths occur beyond the immediate postpartum period. Comprehensive care extending throughout the first year postpartum is essential for monitoring health and addressing emerging risks.
Are most pregnancy-related deaths in the U.S. preventable?
Yes, over 80 percent of pregnancy-related deaths in the U.S. are considered preventable, indicating a critical opportunity for healthcare systems to improve maternal health outcomes through better prenatal and postpartum care.
What measures can help reduce high maternal mortality rates in the U.S.?
To reduce high maternal mortality rates, the U.S. needs to invest in public health infrastructure, enhance the quality of maternity care, and implement policies that address the specific needs of diverse populations, especially in states with higher mortality rates.
How has the COVID-19 pandemic affected maternal health in the U.S.?
The COVID-19 pandemic has been linked to an increase in pregnancy-related deaths, with significant spikes observed in 2021. The pandemic exacerbated existing health disparities and underscored the need for robust maternal healthcare systems.
What are the leading causes of pregnancy-related deaths in the U.S.?
Cardiovascular disease has emerged as the leading cause of pregnancy-related deaths in the U.S., accounting for over 20% of such fatalities. This shift from complications like hemorrhage to chronic conditions signifies a changing landscape of maternal health risks.
Why is late maternal death significant to maternal health discussions?
Late maternal deaths, occurring between 42 days and one year postpartum, are significant because they highlight the need for continuity of care and comprehensive support for women recovering after childbirth, a time often overlooked by healthcare systems.
What data tracking challenges exist regarding maternal mortality in the U.S.?
Until 2018, there was no standardized national system for tracking maternal deaths in the U.S., making it difficult to obtain accurate and comprehensive data on pregnancy-related deaths, which is now being addressed with improved death certificate protocols.
What actions are needed to improve maternal health outcomes in the U.S.?
Improving maternal health outcomes in the U.S. requires increased investment in public health initiatives focused on reducing maternal mortality rates, addressing health disparities, and expanding access to quality reproductive care throughout pregnancy and postpartum.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality | The U.S. leads high-income countries in maternal mortality rates, with a significant rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Disparities | Notable disparities exist by state, race, and ethnicity, with American Indian and Alaska Native women facing the highest mortality rates. |
| Leading Cause of Death | Cardiovascular disease is now the leading cause of pregnancy-related deaths, accounting for over 20%. |
| Impact of COVID-19 | The pandemic may have exacerbated the rise in maternal deaths, especially in 2021. |
| Postpartum Care | Late maternal deaths (42 days to 1 year after pregnancy) account for nearly a third of deaths, indicating the need for improved postpartum care. |
| Investment in Healthcare | Increased investment is needed in healthcare infrastructure and innovative solutions to improve maternal health outcomes. |
Summary
Maternal mortality in the U.S. has reached alarming levels, continuing to rise despite being in a high-income country. The trends from the latest studies highlight that over 80% of these deaths are preventable, emphasizing the urgent need for enhanced prenatal and postpartum care. Danial disparities influenced by race and state policies underscore the critical nature of addressing the healthcare inequalities contributing to this public health crisis. Investment in healthcare infrastructure and innovative solutions is essential to ensure better maternal health outcomes and reduce mortality rates in the future.

Boston Marathon Mental Health: Understanding Runners’ Stories
The Boston Marathon is not just a test of physical endurance; it also serves as a significant event in discussions about mental health. As more and more runners take on the challenge of this iconic 26.2-mile race, the emphasis on Boston Marathon mental health is becoming increasingly crucial. Many participants experience a range of psychological effects during marathon training, whether it’s the motivation to push through the miles or the mental hurdles faced on race day. This rich tapestry of human emotion is woven into the marathon experience, offering insights into the mental health during marathon preparation and the psychological effects of running long distances. Ultimately, the stories of Boston Marathon runner experiences illuminate the profound intersection of physical and mental resilience in the face of adversity.
Running long distances, such as during the Boston Marathon, presents unique psychological challenges and rewards, shaping participants’ mental well-being. This famous event not only tests athletes’ physical limits but also highlights significant aspects of mental health and self-discovery. Throughout the journey of marathon training psychology, runners often confront personal battles and cultivate motivation that extends beyond the finish line. The Boston Marathon serves as a communal space for diverse experiences, reflecting the multifaceted relationship between running and mental wellness. These narratives are not just about racing; they delve deep into the transformative power of endurance, revealing how such events can foster a stronger sense of self and community.
The Psychology of Marathon Training
Training for a marathon is not just a physical challenge; it is also a profound psychological journey. As runners prepare to tackle the daunting 26.2 miles, they undergo a transformation that often affects their mental health. Many runners find solace in the rhythm of their training, using it as a form of meditation that allows them to process their thoughts and emotions. This psychological effect can lead to improved mood, lower anxiety levels, and a stronger sense of self-worth—all critical components of overall mental health during marathon preparation.
Moreover, marathon training fosters resilience. Athletes face both physical and psychological hurdles, such as burnout, injuries, and the inevitable self-doubt that arises during long runs. Overcoming these challenges during training helps runners develop coping strategies that can be beneficial in everyday life. As they push through fatigue and learn to manage their mental state, they gain valuable insights into their capabilities, which can translate into improved mental fortitude in various life situations.
Mental Health During the Boston Marathon
The Boston Marathon serves as a unique convergence of physical exertion and mental health challenges. While many participants are driven by personal goals or reasons tied emotionally to loved ones, the psychological toll of the race can be strenuous. Upon crossing the finish line, some runners experience acute distress, which can manifest as panic or disorientation. Jeff Brown, lead psychologist of the Boston Marathon medical team, emphasizes the importance of mental health awareness during such a rigorous event, highlighting that the stressors of training and competing can significantly affect runners’ psychological states.
In many cases, completing the marathon is as much about personal triumph as it is about mental endurance. Runners often deal with overwhelming emotions—joy, relief, sadness—as they confront their vulnerabilities and celebrate their achievements. Brown points out that this connection between the mental and physical aspects of running the Boston Marathon can be profound: each medal not only symbolizes physical accomplishment but also represents emotional resilience. Runners leave with not just a tangible reward, but a deeper understanding of their mental capacity, inspiring them to tackle future challenges.
Running Motivation at the Boston Marathon
Motivation plays a pivotal role in the journey toward the Boston Marathon, influencing runners from various backgrounds and experiences. For many, the drive to participate stems from personal stories—be it honoring a loved one, overcoming personal health challenges, or simply seeking a sense of accomplishment. This intrinsic motivation often fuels their training, fostering a mental environment conducive to achieving their goals. As participants gather, their unique motivations create a supportive atmosphere where shared experiences amplify their individual resolve to conquer the marathon.
Understanding the runners’ motivations is crucial for mental health professionals like Jeff Brown, who provides psychological support during the event. He observes that the act of running the Boston Marathon becomes a ritualistic affirmation for participants. It allows them to channel their energy into a focused pursuit, granting meaning to their struggles and triumphs. This competitive yet communal environment cultivates resilience and determination, proving that motivation—whether external or internal—can significantly impact both mental and physical outcomes during the race.
The Psychological Effects of Marathon Running
The psychological effects of marathon running extend far beyond crossing the finish line. Runners often experience a range of emotions during training and on race day, including anxiety, excitement, and deep introspection. As they engage in the process of training, the repetitive nature of running can lead to moments of clarity and emotional release. This cathartic process enables individuals to confront personal challenges, giving them a platform to reflect on their lives and emotions through the lens of their running experiences.
Moreover, the psychological benefits gained from marathon running can last well beyond the race itself. Studies have shown that consistent long-distance runners report higher levels of self-esteem and lower levels of anxiety and depressive symptoms. This suggests that marathon running serves not only as physical exercise but also as a vital mental health tool. For many, the emotional highs and lows encountered throughout their training and racing experience contribute to a greater awareness of their mental health, reshaping their approach to life’s challenges.
Marathon Training Psychology
Understanding the psychology behind marathon training is essential for both novice and experienced runners. Training for such a grueling event demands not only physical preparation but also a strong mental framework. Runners often set specific, realistic goals—such as maintaining a steady pace or completing long runs—which require discipline and focus. Throughout this process, athletes learn to manage their expectations, cope with setbacks, and celebrate small victories, all of which contribute to their mental toughness.
Additionally, the community support surrounding marathon training plays a crucial role in nurturing a positive psychological environment. Runners often join clubs or groups, finding camaraderie and motivation among peers. This social element alleviates feelings of isolation, promotes a sense of belonging, and enhances their overall mental health. As participants share their experiences and challenges, they create a network of encouragement, making the arduous training process more enjoyable and psychologically enriching.
Unique Runner Experiences at the Boston Marathon
Every participant in the Boston Marathon has a unique story that shapes their experience on race day. From first-time runners to seasoned athletes, each individual brings their own motives, struggles, and aspirations to the marathon. For some, the journey may involve overcoming physical injuries or personal losses, while others see the marathon as a celebration of fitness and fortitude. This diversity in runner experiences adds a rich layer to the collective event, emphasizing the emotional and psychological significance of the day.
These personal narratives often intertwine with larger themes of resilience and community. Runners may form connections with fellow participants who share similar backgrounds or stories, fostering an environment of support and understanding. Jeff Brown acknowledges that witnessing these interactions can be a powerful reminder of the human experience—the vulnerabilities and strengths that come to light during such a demanding endeavor. Ultimately, each runner’s journey at the Boston Marathon is a testament to not only their physical capabilities but also their mental resilience.
Affirmation and Identity in Marathon Running
Marathon running often provides a sense of affirmation and identity for participants, allowing them to reshape how they view themselves. By conquering the challenges of marathon training and racing, individuals affirm their capabilities, fostering a positive self-image that can permeate other areas of their lives. Jeff Brown discusses how crossing the finish line can lead to a transformative moment for many; they feel a sense of pride and accomplishment, transitioning from a mere participant to a ‘hero’ in their own right.
This feeling of achievement often resonates deeply with runners, as they integrate their marathon experiences into their personal narratives. They return to their lives not just as individuals who completed a race but as empowered beings who have faced and overcome significant challenges. This strengthened self-identification can have lasting impacts, encouraging runners to engage more fully with their communities and personal goals, while also contributing positively to their mental health and overall happiness.
Coping Strategies for Marathon Runners
Developing coping strategies is essential for marathon runners to enhance their psychological resilience throughout their training and race-day experiences. Runners learn to navigate discomfort not only physically but mentally, often applying techniques such as visualization, positive affirmations, and mindfulness to manage stress. Visualization, for instance, allows athletes to mentally rehearse their race, enhancing their confidence and preparation. These strategies become crucial as runners face intense emotional and physical fluctuations during their training journey.
Beyond race-specific coping mechanisms, these strategies can provide tools that apply to other areas of life. By mastering emotional regulation techniques during the final weeks of training or on race day, runners can better handle daily stressors that arise, thereby promoting overall mental health. Jeff Brown advocates for these coping techniques as vital resources to help runners not only complete their marathon but also navigate the complex emotional landscape that accompanies such significant personal challenges.
Emotional Reflections Post-Marathon
The moments after crossing the finish line at the Boston Marathon can encapsulate a whirlwind of emotions. Runners often find themselves reflecting on their entire journey, from training to race day. They may feel overwhelming joy, significant relief, or even sadness as they process the culmination of their efforts. For some, the aftermath is a time for quiet reflection, allowing them to internalize what the marathon experience has meant for them on a personal level. Jeff Brown highlights that this reflective period is crucial for understanding the marathon’s deeper impact on their mental health.
As runners bask in the glow of their accomplishment, they are also confronted with the reality of what lies ahead. The transition from the structured training schedule to the post-marathon phase can evoke feelings of uncertainty or loss. Many marathoners will grapple with finding new goals or ways to maintain their physical and mental wellbeing. This transitional period plays an essential role in shaping their future interactions with running and community, influencing their ongoing commitment to mental health and personal development.
Frequently Asked Questions
How does mental health impact marathon running, specifically in the Boston Marathon?
Mental health plays a significant role in marathon running, especially in the Boston Marathon, where emotional and psychological challenges can be as intense as the physical demands. Runners often deal with anxiety, nervousness, or fear of failure leading up to the event. The Boston Marathon showcases various psychological effects of marathon running, from the euphoric feeling of achievement at the finish line to the intense distress some experience due to their physical conditions. The support of mental health professionals on-site helps runners navigate these challenges effectively.
What psychological effects can participants of the Boston Marathon expect during their training?
Training for the Boston Marathon can evoke a range of psychological effects, including increased motivation and a greater sense of achievement. Marathon training psychology suggests that as runners prepare, they often experience enhanced self-esteem and self-worth. However, they may also encounter periods of burnout or fatigue. Understanding these effects can help runners maintain a balanced mindset and focus on their mental health during demanding training periods.
What are some common mental health challenges faced by Boston Marathon runners?
Common mental health challenges faced by runners during the Boston Marathon include performance anxiety, stress from competition, and the fear of injury or failure. Many participants may feel overwhelmed due to the intense pressure and expectations they set for themselves. Addressing these psychological concerns through techniques like mindfulness, positive affirmations, and visualization can significantly improve one’s mental health during such a grueling marathon.
How can running the Boston Marathon serve as a motivation for mental health improvement?
Running the Boston Marathon can be a powerful motivator for mental health improvement. The emotional journey involved in preparing for and completing the marathon can foster a strong sense of purpose and belonging. Many runners find that achieving personal goals creates a positive feedback loop that boosts their overall mental health. Additionally, connecting with fellow runners during training and on race day provides a supportive community that encourages sharing experiences and coping strategies.
What role does community support play in the mental health of Boston Marathon runners?
Community support significantly contributes to the mental health of Boston Marathon runners. Engaging in group training sessions allows runners to share their experiences, struggles, and successes, which helps build camaraderie and reduces feelings of isolation. This collective spirit not only enhances motivation but also provides the emotional backing needed during challenging moments of preparation and race day, promoting a sense of belonging that can improve mental resilience.
How can runners prepare for the emotional toll of the Boston Marathon?
Runners can prepare for the emotional toll of the Boston Marathon by developing coping strategies to manage stress and anxiety. Techniques such as mindfulness meditation, visualization, and relaxation exercises can help runners stay focused and calm. Setting realistic goals, practicing positive self-talk, and seeking support from mental health professionals or fellow runners can also aid in preparing emotionally for both training and race day challenges.
What insights do Boston Marathon runner experiences provide about mental health in sports?
Boston Marathon runner experiences offer valuable insights into the correlation between mental health and sports. Many runners report transformative moments of reflection on personal challenges and growth during the race. The diverse motivations behind their participation often reveal how physical endurance merges with emotional resilience. These experiences highlight the importance of mental health awareness in sports, emphasizing that both mindset and physical ability are crucial for success in challenging events like the Boston Marathon.
| Key Point | Details |
|---|---|
| Mental Health Assessments | Psychologist Jeff Brown evaluates runners for psychological distress, which can manifest in various forms like confusion and fear. |
| Personal Drivers | Runners often have deeply personal reasons for participating, such as honoring deceased loved ones or overcoming health challenges. |
| Transformational Achievement | Completion of the marathon serves as a significant milestone for runners, often bringing a profound sense of accomplishment. |
| Community and Support | The event fosters a strong sense of community among participants, providing emotional support and affirmation. |
| Variety of Experiences | Each runner has unique motivations and experiences, highlighting the psychological diversity present in the marathon community. |
Summary
The Boston Marathon mental health aspect is an essential theme, as it identifies the deep, personal journeys that each runner undertakes. This iconic race not only tests physical endurance but serves as a crucible for psychological reflection and reaffirmation of self-worth. Runners face various emotional and mental challenges, and through overcoming these obstacles, they experience a transformational journey that culminates at the finish line. The mental resilience developed by participants during the marathon exemplifies the profound impact that such events can have on an individual’s mental health.
TIM-3 Therapy for Alzheimer’s: A Revolutionary Discovery
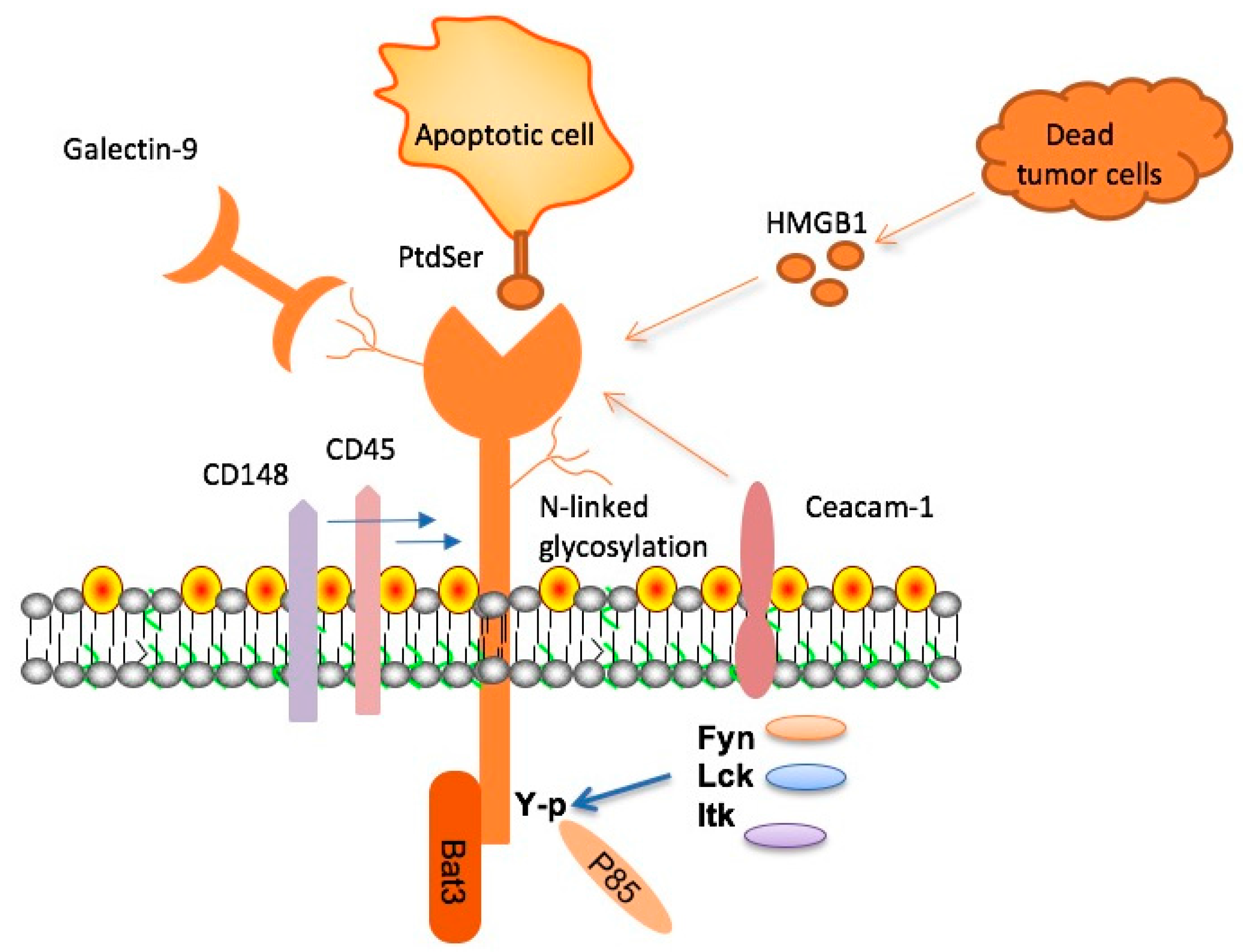
TIM-3 therapy for Alzheimer’s is an innovative approach that leverages the immune system’s mechanisms to combat Alzheimer’s disease, a condition that afflicts millions worldwide. Recent research highlights the potential of TIM-3, a checkpoint molecule, to enable microglia – the brain’s immune cells – to effectively clear toxic amyloid plaques linked to cognitive decline. This breakthrough is particularly significant as it aligns with developments in Alzheimer’s disease research that suggest harnessing immune strategies can enhance cognitive function improvement. By releasing the inhibitory effects of TIM-3, scientists aim to rejuvenate microglia, restoring their ability to facilitate plaque clearance and memory enhancement. As we explore the intricate connection between the immune system and Alzheimer’s, TIM-3 therapy may emerge as a promising candidate in the landscape of treatment strategies.
The exploration of TIM-3 in Alzheimer’s treatment reflects broader innovations in addressing neurodegenerative diseases through immune modulation. By targeting checkpoint molecules similar to those used in cancer therapies, researchers are investigating how therapeutic strategies aimed at this genetic factor can lead to advancements in cognitive health. Additionally, the unique role of microglia in maintaining brain homeostasis while combating plaque formation by amyloid beta underscores the delicate balance necessary for cognitive preservation. This situation invites further inquiry into how immune dysfunction contributes to Alzheimer’s, potentially reinforcing the relationship between immunological health and neurodegeneration. With studies like these paving the way, they challenge conventional approaches and stimulate a new paradigm in Alzheimer’s disease management.
The Role of TIM-3 in Alzheimer’s Disease Therapy
Recent research highlights the potential of TIM-3 therapy for Alzheimer’s disease, revealing that blocking this immune checkpoint molecule could enhance the ability of microglia to target and remove amyloid plaques from the brain. When researchers deleted the TIM-3 gene in a laboratory setting, they observed that mice demonstrated improved cognitive function and plaque clearance. This finding is significant because it suggests that TIM-3 plays a restrictive role in the brain’s immune response, and by inhibiting it, we may be able to shift the immune system’s balance toward more effectively combating Alzheimer’s pathology.
The therapeutic strategy surrounding TIM-3 focuses on its dual function within the immune system; while it is crucial for regulating T cell activity to prevent autoimmunity, its overexpression in Alzheimer’s patients hinders microglial functionality. By utilizing anti-TIM-3 antibodies or other small molecules that block its action, researchers could potentially restore microglial activity, facilitating the clearance of harmful plaques and leading to significant cognitive improvements. This approach may usher in new, targeted Alzheimer’s treatments that effectively harness the body’s immune mechanisms.
Understanding Microglia’s Role in Alzheimer’s Disease
Microglia are the brain’s primary immune cells, and they perform essential roles in maintaining healthy cognitive function. In Alzheimer’s disease, however, the role of microglia becomes complicated. Elevated levels of TIM-3 inhibit their function, preventing the clearing of amyloid beta plaques that contribute to cognitive decline. Understanding this relationship highlights the need for innovative strategies, such as TIM-3 therapy, to restore normal microglial activity without compromising their critical functions in the brain.
In the context of Alzheimer’s disease research, it is crucial to explore the dual role of microglia not only in plaque removal but also in synaptic pruning and maintaining neurological health. Typically, microglia help eliminate excess synapses, fine-tuning circuits critical for memory and learning. With aging and the onset of Alzheimer’s, however, their function becomes impaired due to molecular signals like TIM-3, underscoring the significance of targeting these pathways for therapeutic interventions.
The Connection Between the Immune System and Alzheimer’s Disease
Emerging findings emphasize the intricate connection between the immune system and Alzheimer’s disease progression. As checkpoint molecules such as TIM-3 regulate immune responses, they can also impact the brain’s susceptibility to plaque accumulation. By understanding how the immune system interacts with Alzheimer’s pathology, researchers can identify new therapeutic avenues to modulate these interactions and potentially enhance cognitive function in patients.
Research into the immune system’s role in Alzheimer’s disease further underscores the potential for developing innovative treatments that can simultaneously address neuroinflammation and cognitive decline. By leveraging knowledge from cancer immunotherapy, where checkpoint inhibitors have shown promise, similar strategies may enhance the body’s immune response in combating Alzheimer’s, as studies suggest TIM-3 blockade could lead to improved microglial activity and plaque clearance.
Cognitive Function Improvement through TIM-3 Inhibition
The inhibition of TIM-3 has been associated with significant improvements in cognitive function in experimental models of Alzheimer’s disease. By allowing microglia to resume their natural role in clearing amyloid plaques, cognitive behaviors in mice were restored, resembling conditions prior to plaque accumulation. This breakthrough suggests that TIM-3 may be a critical target for therapeutic intervention aimed at not only halting progression but also reversing some cognitive deficits associated with Alzheimer’s.
Strategies focused on TIM-3 inhibition pave the way for a new class of Alzheimer’s treatments. These could potentially yield substantial benefits, especially considering the limited success of existing therapies. By prompting microglial activation, TIM-3 targeted treatments may restore cognitive abilities, offering hope where other strategies have fallen short. As pharmaceutical advancements progress, this mechanism holds promise for enhancing the quality of life for Alzheimer’s patients.
Current Strategies in Alzheimer’s Disease Research
Amid numerous drug trial failures in Alzheimer’s treatment, novel strategies leveraging immune pathways are gaining traction. Research focusing on checkpoint molecules like TIM-3 represents a paradigm shift in the understanding of Alzheimer’s pathology, providing fresh insights into manipulating the immune response to facilitate plaque clearance. Trials assessing the effectiveness of TIM-3 inhibitors are anticipated to yield critical data that could lead to viable solutions for challenging Alzheimer’s cases.
The emphasis on immune modulation through TIM-3 therapy underscores a broader trend in Alzheimer’s disease research that seeks to identify and exploit immune checkpoints for potential cognitive intervention. As new findings emerge, the prospect of integrating immunotherapy alongside conventional approaches may redefine treatment methodologies, creating a more comprehensive arsenal to combat Alzheimer’s and improve patient outcomes.
Future Implications of TIM-3 Research in Alzheimer’s Therapy
The implications of TIM-3 research are far-reaching and may transform Alzheimer’s therapeutics. As scientists explore the potential of TIM-3 inhibition, they are starting to bridge knowledge from immunology and neuroscience, potentially leading to groundbreaking treatments for Alzheimer’s that harness the body’s own immune responses. This could not only mitigate symptoms but also address the underlying mechanisms contributing to the disease, promising a future where Alzheimer’s can be effectively managed.
Looking ahead, the size and scope of ongoing studies into TIM-3 signaling pathways are crucial for determining the precise effects on human populations. Current investigations involving mouse models will help refine these treatment modalities, bringing researchers closer to human clinical applications. By understanding how TIM-3 inhibition can enhance microglial functionality, future therapies might significantly alter the landscape of Alzheimer’s disease management.
Mechanisms of Alzheimer’s Disease Progression
The mechanisms driving Alzheimer’s disease progression are complex and multifaceted, involving a range of biological processes. Central to this is the accumulation of amyloid plaques, which are not effectively cleared by microglia due to inhibitory signals like TIM-3. This accumulation leads to neuroinflammation and neuronal damage, underscoring the importance of understanding how to manipulate these pathways for effective treatment.
Research into the molecular intricacies of Alzheimer’s disease reveals the role of genetic factors in influencing disease severity and progression. Studies have shown that a heightened expression of TIM-3 in individuals with the disease correlates with cognitive decline, suggesting that targeting this molecule could restore lost cognitive functions. Comprehensive exploration of these mechanisms is vital for deciphering potential therapeutic interventions.
Clinical Trials and the Future of Alzheimer’s Treatments
The journey toward effective Alzheimer’s treatments is increasingly focused on clinical trials investigating TIM-3 inhibitors. With early results demonstrating promising outcomes in pre-clinical models, there is optimism about advancing these therapies to human trials. The unique role of TIM-3 in modulating immune responses presents a compelling case for its potential in restoring cognitive function and improving quality of life for patients.
As clinical trials continue to unfold, researchers are assessing not only efficacy but also long-term effects of TIM-3 targeted therapies. Understanding the pharmacodynamics and safety profile of these inhibitors will be paramount as they move toward approval processes. Future research directions will undoubtedly focus on optimizing these therapies to maximize benefits for Alzheimer’s patients and provide new hope in the fight against this debilitating disease.
Challenges and Considerations in Alzheimer’s Research
Despite the exciting prospects of TIM-3 as a therapeutic target in Alzheimer’s disease, challenges remain. Understanding the specific mechanisms by which TIM-3 affects microglial activity is crucial, as overly tampering with immune responses could lead to unforeseen consequences, including potential neuroinflammation. Balancing efficacy with safety is paramount in this evolving research landscape.
Furthermore, the variability of Alzheimer’s presentation among patients complicates the development of universally applicable treatments. As researchers strive to tailor TIM-3 therapies to individual genetic profiles, personalized approaches may emerge, maximizing effectiveness and minimizing risks. Continued exploration of the immune system’s role in Alzheimer’s will be critical for overcoming these hurdles and advancing therapeutic strategies.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s targets the TIM-3 molecule, which inhibits microglia, the brain’s immune cells, from clearing amyloid plaques. By blocking TIM-3, this therapy frees microglia to attack and remove these plaques, which can improve cognitive function and memory.
How does TIM-3 relate to Alzheimer’s disease research?
TIM-3 is linked to late-onset Alzheimer’s disease through genetic studies. Research has shown that high TIM-3 expression on microglia leads to reduced plaque clearance, making it a significant target in Alzheimer’s disease research for restoring cognitive function.
Could TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Yes, TIM-3 therapy has been demonstrated to enhance cognitive function in animal models of Alzheimer’s. By allowing microglia to effectively clear amyloid plaques, TIM-3 inhibition may lead to memory improvement in patients.
What role do microglia play in TIM-3 therapy for Alzheimer’s?
Microglia are the immune cells of the brain responsible for clearing away harmful plaques. In TIM-3 therapy, inhibiting TIM-3 enables these crucial cells to attack amyloid plaques more effectively, which is essential for treating Alzheimer’s disease.
What are the implications of TIM-3 therapy for future cancer treatment strategies?
While TIM-3 therapy primarily focuses on Alzheimer’s, its approach of blocking immune checkpoint molecules may offer insights into developing more effective cancer treatment strategies by enhancing immune responses against tumors, given TIM-3’s role in regulating immune activity.
How long did the research into TIM-3 therapy for Alzheimer’s take?
The research on TIM-3 therapy for Alzheimer’s spanned five years, focusing on the genetic implications and the impact of TIM-3 on microglial function, leading to potential therapeutic applications in human conditions.
What evidence supports the effectiveness of TIM-3 therapy in Alzheimer’s?
Evidence from mouse models indicates that deleting the TIM-3 gene enhances plaque clearance and improves cognitive behaviors. This suggests that TIM-3 therapy could be a viable option to improve cognitive function in Alzheimer’s patients.
What is the next step in TIM-3 therapy research for Alzheimer’s patients?
The next step is testing human anti-TIM-3 antibodies in mouse models of Alzheimer’s to evaluate their effectiveness in preventing plaque formation, paving the way for clinical applications in treating Alzheimer’s disease.
Is TIM-3 only relevant for Alzheimer’s disease or can it be applied to other conditions?
While TIM-3 is particularly relevant in Alzheimer’s disease due to its role in immune regulation and plaque clearance, its mechanisms may also provide insights for other neurodegenerative conditions and autoimmune diseases where immune checkpoints are involved.
What challenges exist in delivering TIM-3 therapy to human patients with Alzheimer’s?
Challenges include ensuring that TIM-3 inhibitors effectively reach the brain, as some therapies targeting amyloid plaques have previously failed due to vascular complications. Research is focusing on developing targeted therapies that minimize risks while maximizing therapeutic effects.
| Key Points | Details |
|---|---|
| TIM-3 Therapy for Alzheimer’s | The therapy utilizes TIM-3 molecule deletion to enhance clearance of plaques and restore memory. |
| Study Findings | Mice without TIM-3 had improved memory as microglia could clear Alzheimer’s plaques. |
| Role of TIM-3 | TIM-3 inhibits microglia from attacking harmful amyloid plaques in the brain. |
| Research Duration | The study took five years, involving multiple experiments and collaborators. |
| Potential Human Application | Proposed treatments include anti-TIM-3 antibodies or small molecules to block TIM-3’s function. |
Summary
The research into TIM-3 therapy for Alzheimer’s disease offers promising insights into potential new treatment avenues. By deleting the TIM-3 molecule, scientists can free microglial cells in the brain to clear away harmful plaques, resulting in improved cognitive functions in affected models. This groundbreaking approach not only highlights the interconnectedness of immune checkpoints in both cancer and Alzheimer’s, but it also reinforces the potential of TIM-3 as a viable target for therapeutic intervention, making TIM-3 therapy a noteworthy consideration in the battle against Alzheimer’s.
Gene Therapy for Hemophilia: A New Era of Healing
Gene therapy for hemophilia is revolutionizing the way we approach the treatment of this challenging condition. Traditionally reliant on regular injections of clotting factor IX, patients like Terence Blue are now experiencing promising new interventions, such as the breakthrough therapy Hemgenix. This innovative treatment aims to provide lasting benefits, reducing the need for frequent infusions and transforming hemophilia management. With gene therapy news advancing rapidly, the potential benefits are becoming clearer, as patients envision a future free from constant worry and the burden of daily needles. As we explore this exciting development in hemophilia treatment, understanding the implications and success stories will shed light on the evolving landscape of gene therapy and its profound effects on patient lives.
In the landscape of advanced medical therapies, genetic modifications are emerging as a significant focus, specifically in the realm of hemophilia management. This cutting-edge approach, often referred to as genomic medicine, targets the underlying genetic issues that cause hemophilia, offering hope to those afflicted with the disorder. By utilizing revolutionary techniques that enhance the body’s natural ability to produce essential clotting factors, patients are beginning to experience newfound freedom from conventional treatment protocols. The efficacy of treatments like Hemgenix signals a new era in hemophilia care, where individuals may be freed from the repetitive burden of factor injections, enhancing their quality of life. As the science of gene therapy continues to progress, it brings with it a wave of optimism that could lead to transformative outcomes for patients struggling with blood disorders.
Understanding Hemophilia and Its Challenges
Hemophilia is a rare genetic disorder that impairs the body’s ability to make blood clots, a process crucial for controlling bleeding. Patients like Terence Blue have spent years grappling with the implications of hemophilia, enduring frequent hospital visits and daily injections of clotting factors. Particularly in severe cases, the fear of spontaneous bleeding and the constant management of the condition can lead to significant physical and emotional challenges. Despite advancements in treatment, many patients still encounter barriers that affect their quality of life.
The complexity of living with hemophilia not only encompasses medical needs but extends to social interactions and psychological impacts. Patients often have to navigate conversations about their condition, which can lead to feelings of isolation. For those diagnosed, the psychological burden of needing to be cautious in everyday activities, combined with the potential social stigma, adds layers to the condition that are often overlooked. This nuanced understanding is essential for comprehending the driving forces behind new treatments and therapies.
The Role of Innovative Treatments in Hemophilia Management
Recent advancements in hemophilia treatment, particularly gene therapy options like Hemgenix, offer renewed hope for many patients. Hemogenix represents a landmark achievement; it is designed to make a single intervention that provides long-term relief from the need for regular clotting factor infusions. This therapy not only alleviates the physical routine of managing hemophilia but also opens the door to a lifestyle with greater freedom and less anxiety about bleeding episodes. The development of such therapies showcases a pivotal shift in the treatment landscape for hemophilia.
The introduction of gene therapy reflects an era of medical innovation that targets the underlying causes of genetic disorders rather than just managing their symptoms. Hemgenix, in particular, corrects the genetic mutation responsible for hemophilia B, allowing for the production of the missing clotting factor IX. As more patients experience the benefits of gene therapy, it stands to redefine the standards of hemophilia management and potentially improve long-term outcomes.
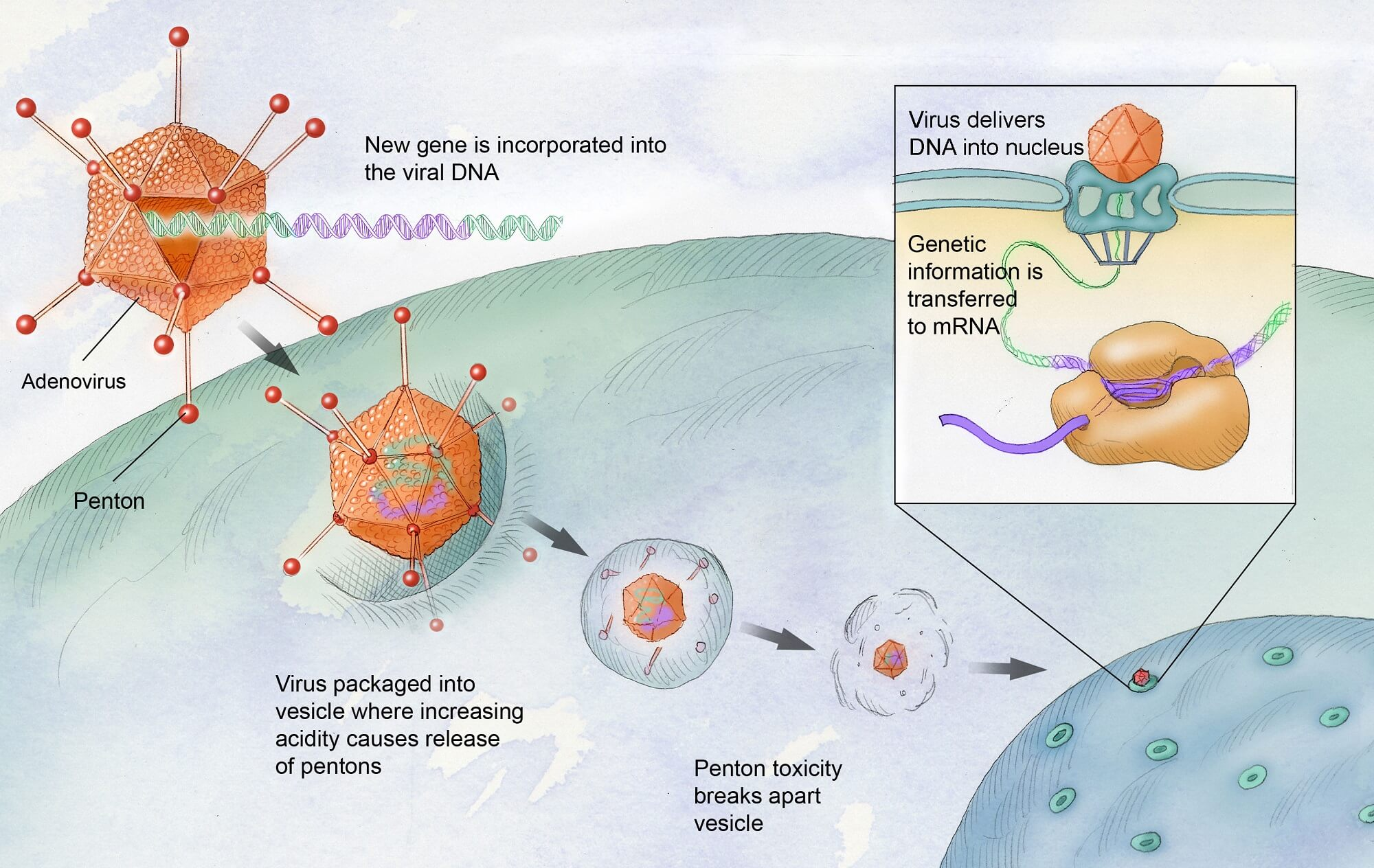
Gene Therapy for Hemophilia: A Breakthrough in Treatment
The FDA’s approval of Hemgenix marked a significant milestone in the landscape of hemophilia treatment. Unlike traditional therapies that require ongoing administration, gene therapy provides a one-time infusion that can permanently alter a patient’s ability to produce clotting factor IX. By using a modified virus to deliver the therapeutic gene into liver cells, gene therapy has the potential to revolutionize how hemophilia B is treated and managed, shifting from routine injections to a more sustainable solution.
Clinical trials have shown that Hemgenix effectively improves factor IX levels in patients, leading to fewer bleeding episodes and reduced reliance on clotting factor injections. This advancement not only represents hope for those living with hemophilia but also embodies the broader trends in medicine that prioritize personalized treatment approaches. As ongoing research continues to unveil the long-term benefits of gene therapy, it is clear that this innovative treatment could transform the lives of countless patients.
The Emotional Experience of Living with Hemophilia
For many living with hemophilia, the treatment journey is as much emotional as it is physical. Patients like Terence Blue describe a life filled with vigilance and care, often highlighting the emotional weight of the condition in social settings and relationships. The ongoing need for factor administration creates a psychological burden that burdens their day-to-day experiences, making treatments like Hemgenix incredibly meaningful as they promise greater normalcy.
The psychological impact of hemophilia cannot be underestimated; many patients face anxiety related to bleeding episodes and the fear of injuries. The hope brought on by gene therapy extends beyond physical health — it encompasses the desire for a more liberated lifestyle, free from the limitations imposed by regular blood factor treatments. As patients begin to experience the effects of successful gene therapy, their stories reflect a renewed sense of optimism and relief.
Market Considerations in Gene Therapies for Hemophilia
While the advancements in gene therapy for hemophilia are promising, they also face significant market challenges. The high costs associated with therapies like Hemgenix create a dynamic where accessibility becomes a concern for many patients. As treatment prices can reach millions, discussions around coverage and patient reimbursement take center stage, impacting the willingness of patients and physicians to adopt new therapies.
The market reality reflects the complexities of balancing innovation with the economic sustainability of treatments. As gene therapies continue to emerge, the effectiveness of these treatments must also translate into patient affordability and insurance coverage. Stakeholders in the healthcare sector are pressing for solutions that not only prioritize patient outcomes but also account for the financial implications of delivering such potent treatments.
Developments in Hemophilia Research and Future Directions
Significant research in hemophilia is underway, driving advancements in treatment modalities, including gene therapies. As scientists and researchers continue to explore innovative approaches to manage hemophilia, new discoveries may soon reshape the landscape of care. The potential of CRISPR technology and other genetic editing methods offers excitement for future breakthroughs that could address various types of hemophilia more effectively.
Current data suggests that ongoing advancements may lead to the development of therapies with broader applications, potentially benefiting not just hemophilia patients but those suffering from related clotting disorders as well. With an ever-growing catalog of gene therapy applications, the future of hemophilia management looks promising, suggesting an era defined by improved health outcomes and enhanced patient quality of life.
Awareness and Education in Hemophilia Treatment
Raising awareness about hemophilia and its treatment options is crucial for ensuring that patients receive optimal care. Educational initiatives can empower patients and their families and contribute to better understanding and acceptance of innovative treatments like gene therapies. By informing individuals about the latest advancements, healthcare providers can support and counsel patients more effectively in their treatment journeys.
Moreover, as healthcare systems evolve, integrating educational efforts with community outreach can facilitate improved health literacy around hemophilia. Such approaches not only enhance patient experiences but also foster a supportive environment where patients feel informed and engaged in their health care decisions. Enhanced awareness can bridge the gap between cutting-edge treatment options and the real-world challenges that patients face, ultimately leading to better outcomes.
Patient Stories: Impact of Gene Therapy on Daily Life
Personal narratives from patients who have undergone gene therapy highlight the transformative potential of treatments like Hemgenix. Stories of individuals who have seen drastic reductions in bleeds and a newfound freedom from daily injections underscore the significance of these medical advancements. Hearing firsthand accounts of patients who have experienced life after gene therapy can serve as motivation for others facing similar challenges.
Such patient stories contribute to a broader understanding of the emotional and physical impact of hemophilia and the hope that innovative treatments bring. As more individuals share their experiences, a narrative emerges that champions resilience and the pursuit of healthier lives. Capturing these personal testimonies not only inspires ongoing research but also reinforces the importance of patient perspectives in shaping the future of hemophilia treatment.
The Future of Hemophilia Treatment: A Holistic Approach
Looking forward, the future of hemophilia treatment lies in developing a more holistic approach that encompasses not only medical interventions but also psychological support and lifestyle adjustments. As therapies like Hemgenix become available, the need for a comprehensive care plan that addresses emotional, social, and physical aspects of living with hemophilia becomes increasingly important, ensuring that patients attain overall well-being.
Future treatment methodologies will likely prioritize collaborative efforts between patients and healthcare professionals, fostering environments where patients feel empowered to engage actively in their care. This holistic perspective can help bridge the gap between medical breakthroughs and day-to-day living, ensuring that patients not only receive adequate treatments but also thrive in their personal lives.
Frequently Asked Questions
What is gene therapy for hemophilia and how does it work?
Gene therapy for hemophilia, such as the treatment known as Hemgenix, involves delivering a corrected copy of the gene responsible for producing clotting factor IX directly into the patient’s liver cells. Using a modified virus as a delivery system, this therapy aims to enable the body to produce its own clotting factors, potentially reducing the need for regular injections of clotting factor in hemophilia patients.
What are the benefits of gene therapy for hemophilia compared to traditional treatments?
The benefits of gene therapy for hemophilia include the potential for a long-lasting solution that reduces or eliminates the need for frequent injections of clotting factor. For many patients, this could drastically improve their quality of life, allowing them to engage in activities without the constant burden of monitoring their condition and managing bleeds.
What is the latest news on gene therapy for hemophilia treatments?
Recent advancements in gene therapy for hemophilia include the FDA approval of Hemgenix, which shows promising results in clinical trials. Patients like Terence Blue have reported significant improvements in their condition post-treatment, highlighting the potential of gene therapy to provide sustainable relief from symptoms associated with hemophilia.
How effective is the Hemgenix gene therapy for hemophilia B?
Hemgenix has demonstrated efficacy in clinical trials, with 94% of participants maintaining sufficient clotting factor IX levels without needing prophylactic treatment three years post-therapy. For many patients, this significant improvement can represent a major breakthrough in managing hemophilia B.
Are there any risks associated with gene therapy for hemophilia?
As with any medical treatment, gene therapy for hemophilia carries potential risks, including immune responses to the viral vector used for gene delivery and elevated liver enzymes. Close monitoring by healthcare providers is essential to manage any side effects and ensure patient safety during and after treatment.
How much does gene therapy for hemophilia cost and is it covered by insurance?
The cost of gene therapy for hemophilia, like Hemgenix, is approximately $3.5 million. While this high price tag poses challenges, many insurance companies negotiate lower rates, and coverage can vary depending on the policy and individual circumstances.
Is gene therapy for hemophilia a permanent solution?
Gene therapy for hemophilia is not universally deemed a cure, but it offers a potentially long-lasting solution, as evidenced by patients who continue to produce clotting factor IX years after treatment. The hope is that these therapies will provide durable effects, greatly enhancing patients’ quality of life.
What does the future look like for gene therapy for hemophilia treatments?
The future of gene therapy for hemophilia looks promising, with ongoing research and potential new therapies in the pipeline. Enhancements in research could lead to more effective treatments, greater accessibility, and improved outcomes for patients living with hemophilia.
| Key Points | Details |
|---|---|
| Gene Therapy Introduction | Gene therapy for hemophilia B, specifically Hemgenix, is a new treatment approved by the FDA in November 2022 that aims to provide long-lasting benefits with a single dose. |
| Patient Experience | Terence Blue, the first patient in New England to receive Hemgenix, experienced a significant improvement with rising factor IX levels and reduced reliance on regular treatments. |
| Market Challenges | Despite the promise of gene therapies, market pressures including high costs and patient acceptance are challenges that impact the availability and sustainability of these treatments. |
| Advancements in Research | Gene therapy research is advancing rapidly, with an increasing number of therapies approved for various conditions, indicating optimism within the scientific community. |
Summary
Gene therapy for hemophilia is revolutionizing the treatment landscape for patients suffering from this condition, offering hope for a more manageable life. As showcased by Terence Blue’s journey with Hemgenix, this innovative therapy not only reduces patients’ dependence on regular interventions but also has the potential to enhance their overall quality of life. The ongoing advancements in gene therapy bring optimism, albeit coupled with market challenges, as healthcare systems adapt to these new possibilities. The future of hemophilia treatment looks promising with these cutting-edge gene therapies, which could significantly alter the day-to-day reality for those living with hemophilia.

Shared Meals and Happiness: The Key to Well-Being
Shared meals and happiness go hand in hand, creating a delightful tapestry of social connections that enrich our lives. Recent happiness research highlights that dining with others significantly boosts well-being indicators, providing not just physical nourishment but also mental health benefits. In fact, individuals who frequently partake in communal meals report higher satisfaction and more positive emotions. This correlation underscores the importance of shared dining experiences, suggesting that our relationships around the table are as crucial as factors like income or employment status. As more people find themselves eating alone, the exploration of how shared meals can promote happiness becomes increasingly vital.
The joy of communal dining is a topic gaining traction in discussions about mental wellness and social engagement. As social connections strengthen through shared culinary experiences, the effects on overall well-being are profound. Recent studies indicate that people who gather for meals are likely to report greater life satisfaction, illuminating a deeper understanding of emotional fulfillment beyond mere financial metrics. This interplay between social gatherings and psychological health opens a dialogue on how integrating shared meals into our daily lives can counteract feelings of isolation and enhance happiness. By fostering these connections, we not only celebrate food but also the relationships that nourish our spirits.
The Importance of Shared Meals for Happiness
Shared meals have emerged as a vital indicator of happiness, surpassing even traditional measures like income and employment. Research indicates that individuals who frequently dine with others report higher satisfaction levels and display more positive emotions. The harmonic atmosphere of shared meals not only fosters social connections but also contributes significantly to overall well-being. Dining together acts like a glue, binding people emotionally and enhancing feelings of joy and contentment.
Moreover, the World Happiness Report emphasizes that this trend transcends demographics, holding true across different cultures and age groups. Interestingly, young people exhibit the sharpest decline in shared meals, correlating significantly with rising feelings of loneliness in their demographic. As social interactions wane, understanding the role of dining together in cultivating happiness is critical for addressing broader mental health challenges.
Social Connections Through Dining
Engaging in meals with others fosters profound social connections, enriching our lives with meaningful interactions. The act of breaking bread together facilitates conversations that deepen bonds between family and friends. This tradition not only promotes emotional well-being but also serves as a platform for reinforcing relationships, thus contributing positively to mental health. When individuals gather around a table, the shared experience of dining transcends mere consumption; it nurtures a sense of belonging and community.
Additionally, the routine of regular family meals or gatherings can help bridge generational gaps and strengthen community ties. As Kaats suggests, understanding how many meals individuals have shared can provide a clearer picture of their social engagement and overall happiness than more ambiguous indicators like income. This insight emphasizes the need for policies targeting communal dining initiatives to enhance social connections and take real steps toward improving community well-being.
Exploring Well-Being Indicators
Measuring happiness and well-being has always posed challenges for researchers, with traditional metrics often failing to capture the nuances of human experience. Shared meals offer a refreshing and objective indicator that researchers, like Micah Kaats, advocate for in their studies. Rather than focusing solely on monetary wealth, assessing someone’s social interactions, particularly their shared dining experiences, offers a more holistic view of their emotional landscape.
This perspective broadens the understanding of well-being indicators by integrating social behaviors into the health conversation. As society grapples with issues surrounding mental health and isolation, it becomes imperative to explore how simple acts such as dining together can serve as a barometer for happiness and fulfillment within communities. This evolving research paradigm could point toward innovative social policies designed to cultivate better mental health outcomes.
The Mental Health Benefits of Shared Meals
Shared meals are more than just sustenance; they play an essential role in promoting mental health. The simple act of gathering around a table encourages communication and bonding, acting as a protective factor against feelings of loneliness and isolation. Studies have shown that regular social interactions during meals can significantly reduce stress levels, leading to improved mental health outcomes. For individuals facing challenges, the support derived from shared dining experiences can be invaluable.
As our society faces increasing mental health crises, encouraging communal dining could serve as a straightforward yet effective intervention. By prioritizing shared meals in our daily lives, we create opportunities for social engagement that are critically linked to improved mental well-being. Policy initiatives that promote communal eating could thus represent a proactive approach in addressing not only mental health issues but also fostering stronger, happier communities.
Strategies for Encouraging Shared Dining
To harness the happiness derived from shared meals, it is crucial to implement strategies that encourage communal dining. Creating community events that focus on dining can facilitate connections among residents. Local governments and organizations can organize potlucks, food fairs, or neighborhood dinners, providing avenues for individuals to come together, share their culinary traditions, and cultivate friendships. Such initiatives can significantly boost social interactions and contribute to the overall happiness of community members.
Additionally, incorporating shared meal practices into family routines can strengthen ties and enhance emotional well-being within households. Encouraging families to set aside time for regular dinners can not only improve communication among members but also instill a sense of stability and support. By making shared meals a priority, families can promote mindfulness and create lasting, joyful memories, significantly enriching their emotional health.
Cultural Perspectives on Dining and Happiness
The cultural significance of shared meals varies across different societies, yet their core essence as facilitators of joy and connection remains universal. In many cultures, communal dining traditions are rituals laden with history and meaning, reinforcing social values while promoting collective happiness. These cultural practices reflect the richness of human interactions, which can be pivotal for fostering social ties and community cohesion.
As ethnographic studies suggest, cultural context can greatly influence how shared meals contribute to individuals’ happiness. For instance, Mediterranean cultures often emphasize long, leisurely meals as central to daily life, inherited from generations, which nurtures strong familial and social bonds. Acknowledging and respecting these diverse perspectives can enhance our understanding of the intricate relationship between food, culture, and well-being, paving the way for future studies that appreciate the depth of shared meal experiences.
The Role of Technology in Dining Experiences
In an increasingly digital world, technology plays a significant role in redefining how we engage in shared meals. Virtual dining experiences and online meal-sharing platforms have emerged as innovative ways for individuals to connect over food, even from afar. This adaptation not only supports current social distancing measures but also provides opportunities for individuals to foster friendships and fulfill their desire for companionship during challenging times.
However, while technology can facilitate connections, it is essential to ensure that it does not replace the richness of face-to-face dining experiences. Balancing virtual engagements with in-person meals can harness the best of both worlds, promoting both social connections and happiness. As our society becomes more connected technologically, it is crucial to leverage these advancements to enhance rather than replace the communal aspects of dining.
Future Research Directions in Shared Meals and Happiness
As scholars like Micah Kaats point out, future research should delve deeper into the causal relationships between shared meals and happiness. Understanding whether shared dining experiences elevate happiness or if happier individuals are more inclined to share meals can have profound implications for public policy and personal well-being. Such research could lead to more effective interventions aimed at promoting mental health through fostering social connections.
Additionally, identifying specific elements of shared meals — such as the type of food, atmosphere, and participants — can further illuminate how these factors contribute to overall happiness. By dissecting these elements, researchers can develop targeted strategies that enhance the positive impacts of shared meals on well-being, ultimately guiding communities toward healthier social practices.
Building a Culture of Togetherness Through Meals
Cultivating a culture that prioritizes shared meals can lead to transformative benefits for individual and collective happiness. When communities recognize the value of dining together, they create environments where social connections thrive, bridging gaps between diverse populations. This cultural shift is not just beneficial for mental health but also enriches societal fabric, fostering empathy and understanding among individuals from different backgrounds.
Promoting a culture of togetherness through meals can have lasting impacts, resulting in improved community ties and resilience against social isolation. Initiatives aimed at celebrating diversity in culinary traditions can serve as powerful tools for enhancing social bonds. By emphasizing inclusivity in dining practices, communities benefit from a rich tapestry of experiences that enhance the overall sense of happiness among their members.
Frequently Asked Questions
How do shared meals influence happiness?
Shared meals have a profound impact on happiness as they foster social connections and strengthen relationships. Research indicates that individuals who regularly dine with others experience increased life satisfaction and express more positive emotions. This correlation suggests that enjoying meals together can enhance well-being and contribute to overall happiness.
What are the mental health benefits of dining with others?
Dining with others offers significant mental health benefits by reducing feelings of loneliness and promoting a sense of belonging. Engaging in shared meals allows for meaningful conversations and social interactions, which are crucial for emotional well-being. This enhances overall happiness and can combat the isolation often felt in modern society.
Is sharing meals a reliable indicator of well-being?
Yes, sharing meals has been identified as a reliable indicator of well-being. Studies show that the frequency of shared meals correlates closely with happiness levels, often as strongly as factors like income or employment status. This suggests that the social aspect of dining plays a critical role in enhancing life satisfaction.
Can increasing shared meals improve social connections and happiness?
Yes, increasing shared meals can significantly improve social connections and overall happiness. By prioritizing communal dining, individuals can build stronger relationships and enhance their emotional well-being. As research indicates, integrating more shared meals into daily life may serve as a simple yet effective way to boost happiness.
What role does happiness research play in understanding shared meals?
Happiness research plays a crucial role in understanding the dynamics of shared meals, highlighting how communal dining relates to social connections and emotional health. By empirically examining the links between shared meals and happiness, researchers offer insights into how fostering these interactions can lead to improved well-being and overall quality of life.
Are there trends in how people currently approach shared meals?
Recent trends indicate a decline in shared meals, with more individuals reporting eating alone. This shift is concerning, as it correlates with increased social isolation and lower reported happiness levels. Addressing this trend by encouraging communal dining could help reverse the decline in social connections and enhance overall well-being.
How can policymakers promote shared meals to enhance community happiness?
Policymakers can promote shared meals by organizing community dining events, supporting local food initiatives, and creating spaces designed for communal eating. Such efforts can enhance social connectivity and improve mental health, addressing loneliness and contributing to higher levels of community happiness.
What is the significance of shared meals in happiness research?
The significance of shared meals in happiness research lies in their ability to serve as an objective measure of social connections and well-being. Unlike subjective measures, the frequency of shared meals provides clear data that can be used to assess happiness and inform interventions aimed at improving overall mental health in communities.
| Key Points |
|---|
| Dining with others is linked to higher life satisfaction and positive emotions. |
| Sharing meals may be as predictive of happiness as income and employment status. |
| Americans are increasingly dining alone; a significant rise since 2003. |
| The link between shared meals and happiness is important for research and policy. |
| Future research may determine if shared meals create happiness or if happy people share more meals. |
| Encouraging shared meals may help address social isolation and improve mental well-being. |
Summary
Shared meals and happiness are intricately connected, as shared dining experiences have been shown to significantly enhance individual well-being. Research indicates that people who consume meals with others report higher satisfaction and joy, hinting at a deeper social need for connection. Therefore, fostering environments where communal dining occurs could play a pivotal role in combatting loneliness and promoting mental health. In a world where social isolation is on the rise, simply gathering around a table may be a powerful step toward enhancing happiness for many.
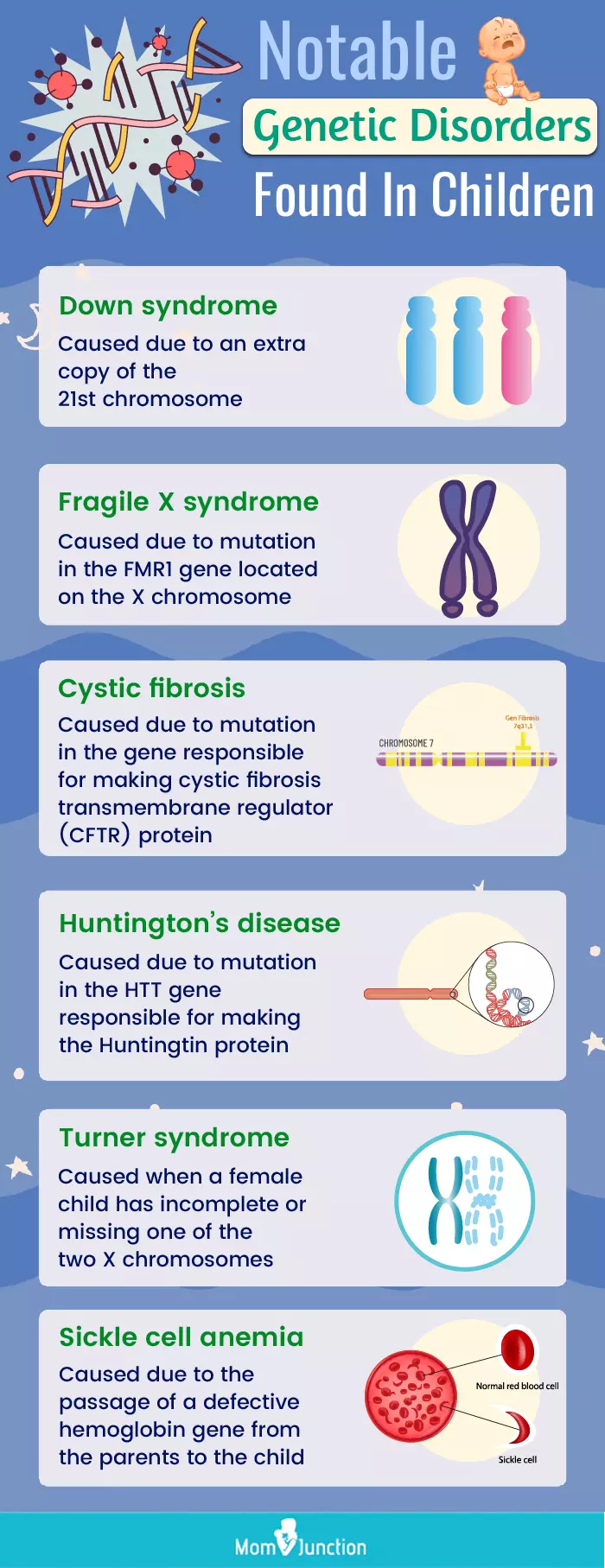
Genetic Disorders Treatable Before Birth: New Research Insights
Genetic disorders treatable before birth represent a groundbreaking advancement in prenatal care, offering hope and potential solutions for families facing the daunting realities of genetic conditions. Recent studies indicate that nearly 300 genetic disorders can now be identified and treated during pregnancy or shortly after birth, opening doors to innovative early intervention strategies. With the help of prenatal genetic screening and genomic sequencing, healthcare providers can detect these treatable fetal conditions much earlier, leading to timely and effective management. As the landscape of prenatal care advances, parents are increasingly empowered with knowledge and options that can improve health outcomes for their unborn children. Early intervention in pregnancy is becoming not just a possibility but a necessity in reshaping the future of pediatric health.
The field of prenatal medicine has made remarkable strides in identifying and managing genetic anomalies that can be addressed before birth. These treatable fetal conditions encompass a range of disorders that can be effectively treated through interventions initiated during pregnancy or immediately after delivery. Through advancements in prenatal genetic screening and genomic analysis, parents now have access to critical information that enables them to make informed decisions regarding their unborn children’s health. Such proactive measures not only mitigate risks associated with certain genetic disorders but also highlight the importance of early intervention techniques that can significantly alter disease progression. The evolving landscape of prenatal care emphasizes the need for comprehensive support systems that guide families through these complex choices and care pathways.
The Necessity of Prenatal Genetic Screening
Prenatal genetic screening has emerged as a critical component of modern obstetrics, aimed at identifying genetic disorders in the fetus before birth. This proactive approach allows for the early detection of treatable fetal conditions, enabling parents to make informed decisions regarding their pregnancy and the potential management of any identified issues. Increased awareness and advancements in technology have led to refined screening methods, enhancing the ability to detect genetic anomalies sooner and more accurately than ever before.
The benefits of prenatal genetic screening extend beyond mere detection; they also encompass the possible interventions that can be initiated based on the information gathered. By establishing a robust framework for prenatal screenings, healthcare providers can now devise personalized care plans that address identified risks. As a result, this practice not only facilitates better health outcomes for the newborn but also alleviates anxiety among expectant parents, who can prepare for potential challenges ahead.
Frequently Asked Questions
What are genetic disorders treatable before birth?
Genetic disorders treatable before birth include conditions identified through prenatal genetic screening that can be managed during pregnancy or immediately after birth. Recent studies have identified nearly 300 conditions that allow for early intervention in pregnancy, improving outcomes for the fetus when diagnosed timely.
How do treatable fetal conditions impact prenatal care?
Treatable fetal conditions significantly impact prenatal care by expanding the options available to families. With advancements in prenatal genetic screening and early detection, healthcare providers can offer interventions during pregnancy that may change disease trajectories and reduce morbidity.
What role does genomic sequencing play in prenatal genetic screening?
Genomic sequencing plays a vital role in prenatal genetic screening by identifying genetic abnormalities and potential treatable conditions. It helps healthcare providers understand the genetic basis of ultrasound abnormalities and uncover treatable fetal conditions, enhancing early intervention strategies.
What are the benefits of early intervention in pregnancy for genetic disorders?
Early intervention in pregnancy for genetic disorders can lead to improved health outcomes for the fetus. By detecting and treating conditions promptly, healthcare providers can reduce the risk of severe complications and facilitate better management strategies, making it possible to prevent irreversible harm.
How can prenatal care advancements help manage treatable fetal conditions?
Prenatal care advancements, such as improved genetic screening and the identification of treatable fetal conditions, enable healthcare professionals to implement early interventions during pregnancy. This proactive approach contributes to better health outcomes for both the baby and the mother, highlighting the importance of timely and accurate diagnosis.
| Key Points | Details |
|---|---|
| Study Overview | Research identifies nearly 300 genetic disorders treatable during pregnancy or shortly after birth. |
| Significance | Timely detection of these disorders may reduce morbidity and allow for early interventions. |
| Research Conducted By | Researchers from Harvard Medical School, Mass General Brigham, and Duke University School of Medicine. |
| Use of Technology | Genomic sequencing helps identify genetic disorders through tests and family history. |
| Treatable Conditions | 296 identified genetic disorders with varying degrees of treatment options available. |
| Goal of Research | To empower families with information to make informed decisions regarding prenatal interventions. |
| Challenges Ahead | Ethical considerations regarding overwhelming information and the emotional impact on families. |
Summary
Genetic disorders treatable before birth are a vital area of research that can significantly impact prenatal care. By identifying nearly 300 genetic conditions that can be addressed during pregnancy or shortly after birth, researchers have opened up new avenues for early intervention. This proactive approach not only aims to improve outcomes for affected fetuses and infants but also empowers families with essential information, offering them choices during a critical time. However, challenges remain, particularly in addressing the ethical considerations and emotional responses of families navigating this complex health information.

Manage Stress During Apocalypse: Expert Tips for Survival
Managing stress during an apocalypse can feel like an insurmountable challenge. With threats ranging from climate change to viral outbreaks continuously looming, it’s easy to succumb to overwhelming anxiety. However, understanding effective stress management techniques is crucial to maintaining psychological resilience in such trying times. Embracing community support during crises can also foster a sense of solidarity and adventure, turning fear into collective strength. By incorporating practical apocalypse survival tips into our daily lives, we can learn to navigate uncertainty with greater ease and confidence.
Navigating the intense pressures brought on by catastrophic events requires innovative strategies and a resilient mindset. During times of upheaval, the importance of emotional well-being cannot be overstated. Finding effective ways to alleviate stress not only enhances our ability to cope with unforeseen troubles but also empowers us to thrive amidst chaos. Transformative support systems and shared experiences can lay the groundwork for overcoming anxiety in tough times, enabling individuals to bond through adversity. Thus, building a framework that fosters cooperation and understanding is essential for both personal and communal growth.
Understanding the Psychological Impact of Crises
In times of crisis, individuals often experience a range of psychological effects that can severely impact their mental well-being. Factors such as uncertainty about the future, loss of routine, and social isolation can lead to increased anxiety and stress levels. It’s crucial to acknowledge these feelings, as they are a natural response to overwhelming situations. Understanding the psychological ramifications of living through crises can help individuals better prepare and manage their stress during these tumultuous times.
Moreover, focusing on psychological resilience is essential in overcoming the anxiety that accompanies major crises. By implementing healthy coping mechanisms such as mindfulness, exercise, or creative outlets, individuals can strengthen their mental fortitude. Recognizing that stress is manageable and that it is normal to feel overwhelmed allows people to navigate their feelings and respond to crises with a more calm and informed approach.
Effective Stress Management Techniques
To effectively manage stress during an apocalypse, it’s important to adopt specific stress management techniques that can provide relief and clarity. Techniques such as deep breathing, meditation, and physical exercise can drastically improve one’s emotional state. Finding time to pause and recalibrate allows individuals to focus on the present rather than succumbing to fears about the future. Implementing these practices daily can help enhance overall mental health, making it easier to face ongoing challenges.
Additionally, maintaining a structured daily routine can greatly benefit individuals struggling to manage stress. Creating a schedule that includes time for work, relaxation, and enjoyable activities promotes a sense of normalcy even in chaotic circumstances. Developing these routines strengthens resilience and encourages a proactive approach to facing external stressors, ultimately leading to greater stability and peace of mind during difficult times.
Building Community Support During Crises
Community support plays a vital role in stress management, especially during an apocalypse. Having a trusted support system can significantly alleviate feelings of isolation and anxiety. Engaging with neighbors, participating in local groups, and forming alliances can build a sense of belonging and safety. When people come together, they share resources, information, and emotional support, creating a buffer against the stress of external chaos.
Moreover, the act of helping others within the community fosters a sense of purpose and connection. Strengthening social bonds not only benefits those receiving help but also uplifts those who are providing it. As individuals engage in mutual support, they build a network of care that is essential for psychological resilience. This connectedness allows individuals to overcome obstacles more effectively and fosters a collective spirit of cooperation.
Cultivating Curiosity and Playfulness in Crisis Management
During stressful times, it can be easy to lose touch with joy and curiosity. However, incorporating elements of playfulness into daily life can significantly counteract feelings of dread and anxiety. Engaging in hobbies, exploring nature, and allowing time for creative expression become vital practices that nourish the spirit. Emphasizing curiosity about the world around us can ignite our passion for life, leading to improved emotional health as we navigate through tough times.
Furthermore, discovering joy in small everyday moments can help shift focus away from apocalyptic fears. Laughter, creativity, and hobbies can act as powerful stress management techniques, resulting in improved morale and enhanced perspective. By fostering a playful outlook and encouraging exploration, individuals can build resilience in the face of adversity, ultimately cultivating an environment of hope rather than despair.
Learning to Accept Uncertainty
Accepting uncertainty is a critical skill to develop during crises, as it allows individuals to navigate with greater ease. The unpredictable nature of apocalyptic situations can lead to heightened anxiety when we cling to the desire for control. Embracing uncertainty means acknowledging that not everything can be anticipated or planned, which can remove pressure and promote a more adaptable mindset.
Additionally, it is important to recognize that uncertainty can also bring opportunity. By viewing challenges as chances for growth, individuals can shift their perspectives and break free from paralyzing fear. This newfound acceptance encourages exploration and innovation, empowering people to take proactive steps for their well-being, even amidst a backdrop of chaos and unpredictability.
Harnessing the Power of Storytelling
Storytelling has long been recognized as a powerful tool for connection and healing. Using narrative techniques can provide individuals with a chance to process their experiences and emotions in a meaningful way. Sharing stories during crises helps individuals articulate their struggles, fears, and hopes, allowing for communal healing and understanding. Moreover, weaving personal stories into broader narratives fosters a sense of solidarity and shared purpose, essential for overcoming apocalyptic stress.
In addition, storytelling offers a unique opportunity for individuals to envision hopeful futures. By expressing their dreams and aspirations through narrative, they can create a sense of agency and direction despite overwhelming circumstances. These stories help reframe the crisis, reminding individuals of their strengths and building resilience in the face of adversity.
Practical Apocalypse Survival Tips
When facing an apocalypse, practical survival tips can be invaluable. Building an emergency kit with essential supplies, such as food, water, and first aid materials, ensures a degree of preparedness. Additionally, engaging in training or educational courses on survival techniques can boost confidence and readiness for unexpected situations. Coupling these skills with mental preparedness enhances the ability to cope during crises, ultimately reducing stress.
Furthermore, forming and participating in community preparedness groups can drastically improve individual survival chances. These groups provide valuable skills, knowledge sharing, and physical resources. As individuals collaborate and teach one another, they reinforce social bonds that are crucial during difficult times, ensuring that both physical and emotional needs are met.
Developing Psychological Resilience
Psychological resilience is the capacity to recover from setbacks, adapt well to change, and maintain a positive outlook during stressful times. Cultivating this resilience requires intentional practices such as mindfulness, self-reflection, and emotional awareness. Engaging in regular practice of these techniques can fortify mental toughness and enable individuals to effectively manage their stress during apocalyptic scenarios.
Moreover, psychological resilience can also be fostered through positive social connections and support networks. Building strong relationships with friends, family, and community members offers essential emotional support that can buoy individuals in times of crisis. As people share experiences and provide encouragement, they collectively enhance their resilience, creating a culture of mutual support that can thrive amid adversity.
Preparing for Future Challenges
Preparation for future crises involves not only tangible preparations but also emotional and mental readiness. Being proactive about potential scenarios helps reduce the feeling of helplessness that often accompanies crises. Developing plans, practicing scenarios, and discussing fears openly with trusted individuals form a foundation of resilience that empowers individuals during challenging times.
Additionally, cultivating a growth mindset encourages ongoing learning and adaptability. Individuals can view challenges as opportunities for development rather than insurmountable obstacles. This proactive approach not only reduces stress but also equips individuals with the tools and perspective necessary to navigate through future challenges confidently.
Fostering Mutual Aid and Cooperation
In apocalyptic situations, fostering mutual aid and cooperation becomes paramount for survival. Developing systems of support where communities help each other can be critical for reducing feelings of isolation and anxiety among individuals. These cooperative efforts enhance social bonds and create a sense of collective responsibility, where everyone works towards the common good, ultimately alleviating stress and uncertainty.
Moreover, the practice of sharing resources and knowledge within communities establishes a robust network of support. These initiatives can include food banks, informal childcare, and skill-sharing workshops, all of which empower individuals and strengthen community resilience. By emphasizing collaboration, individuals are more likely to thrive during crises, fostering a mindset geared towards building a supportive and resilient society.
Frequently Asked Questions
What are some effective stress management techniques during an apocalypse?
Effective stress management techniques during an apocalypse include gathering accurate information to reduce uncertainty, engaging in community support for collective resilience, and practicing mindfulness to stay grounded. It’s essential to integrate activities that foster curiosity and connection with others to combat anxiety and build psychological resilience.
How can community support during crises help manage stress in an apocalyptic scenario?
Community support during crises is vital for managing stress in an apocalyptic scenario. Strong social bonds provide emotional assistance, practical resources, and collaborative problem-solving opportunities, which can alleviate feelings of anxiety and isolation. Forming mutual aid networks can enhance the sense of security and resilience in uncertain times.
What role does psychological resilience play in managing stress during an apocalypse?
Psychological resilience is crucial for managing stress during an apocalypse. It allows individuals to adapt to changing circumstances, maintain hope, and bounce back from adversity. Building resilience involves cultivating a positive mindset, fostering social connections, and developing effective coping strategies to navigate the challenges of survival.
Can overcoming anxiety in tough times improve survival skills during an apocalypse?
Yes, overcoming anxiety in tough times can significantly improve survival skills during an apocalypse. By managing stress effectively and developing a focused approach, individuals can think clearer, make better decisions, and take constructive actions to ensure their safety and well-being in crisis situations.
What are some practical apocalypse survival tips for managing stress in chaotic environments?
Practical apocalypse survival tips for managing stress include establishing a routine to create stability, prioritizing essential tasks, utilizing stress relief techniques such as deep breathing, and seeking support from others. Engaging in community-driven initiatives can also enhance emotional strength and foster a sense of purpose.
| Key Point | Description |
|---|---|
| Managing Stress | Gather information about risks to determine what is worth stressing over. |
| Cooperation and Community | Working together and forming mutual aid relationships can help during crises. |
| Perspective Taking | Assess threats from multiple angles for a clearer understanding. |
| Curiosity and Play | Engage in curious and playful activities to build resilience. |
| Social Bonds | Leverage friendships and community ties to provide support during tough times. |
Summary
To effectively manage stress during an apocalypse, it is essential to gather and analyze information about potential risks rather than succumbing to fear and anxiety. Building strong community ties, promoting cooperation, and engaging in playful activities can foster resilience and better preparedness for future challenges. Embracing curiosity and viewing apocalyptic situations as opportunities for growth can help navigate these tumultuous times.
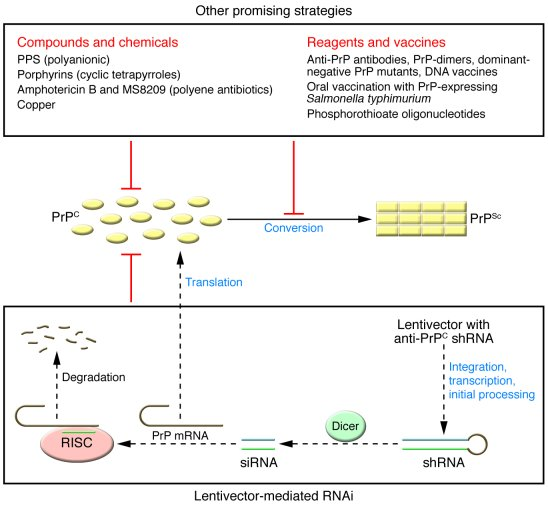
Prion Disease Treatment: Breakthroughs in Gene Editing
Prion disease treatment has emerged as a beacon of hope for those afflicted by these devastating neurological disorders, such as Creutzfeldt-Jakob disease and fatal familial insomnia. Researchers like Sonia Vallabh and Eric Minikel are leading the charge in developing innovative therapies, particularly through the promising approach of gene editing therapy. Recent breakthroughs published in the journal Nature Medicine offer a glimmer of optimism, demonstrating that modifying specific genes can significantly reduce harmful protein levels in the brain of lab mice. This remarkable achievement not only extended the mice’s lifespans but also highlights the potential for these techniques to translate into human clinical trials in the future. As this research progresses, the scientific community eagerly anticipates the implications for effective treatment against prion diseases, which have remained largely untreatable until now.
The pursuit of effective therapies for prion diseases, those rare and fatal brain disorders caused by misfolded proteins, is gaining momentum. In this context, innovative techniques such as genetic modification are being explored by dedicated researchers who personally understand the stakes involved. Groundbreaking studies have revealed that targeted alterations in specific genes can lead to a significant decrease in toxic protein levels, creating possibilities for impactful treatments. As scientists forge ahead, their efforts resonate deeply within the community, especially for those like Vallabh and Minikel, who are not just researchers but also patient-advocates. The quest for solutions to prion diseases, often characterized by conditions like Creutzfeldt-Jakob disease and fatal familial insomnia, represents a pivotal moment in medical research.
Understanding Prion Diseases: An Overview
Prion diseases comprise a group of rare neurodegenerative conditions that lead to severe brain damage and cognitive decline. They are characterized by the misfolding of prion proteins, which can induce normal proteins in the brain to also misfold, leading to the formation of aggregates that are toxic to neural cells. Some well-known examples of prion diseases include Creutzfeldt-Jakob disease, fatal familial insomnia, and Gerstmann-Sträussler-Scheinker disease. These conditions can be sporadic, occurring without any known genetic mutation, or familial, linked to inherited mutations in the prion protein gene.
The impact of prion diseases is profound, primarily due to their fatal nature and the lack of effective treatment options. Patients suffering from these disorders experience progressive neurological symptoms, which eventually lead to death. Understanding the underlying mechanisms of prion diseases is essential not only for developing potential therapies but also for raising awareness and facilitating early diagnosis, which can be critical for families who may carry genetic predispositions to such conditions.
The Potential of Gene Editing Therapy in Prion Disease Treatment
Recent advancements in gene editing technology, particularly those pioneered by researchers like Sonia Vallabh and Eric Minikel at the Broad Institute, offer new hope for treating prion diseases. The innovative gene editing therapy focuses on creating precise alterations in the genetic code responsible for the production of misfolded prion proteins. In laboratory studies with mice, researchers demonstrated that by changing just a single base pair in the gene, they could reduce the levels of harmful proteins in the brain by half, significantly extending the lifespan of the subjects by an impressive 52%.
This milestone marks a significant leap forward in the quest for developing effective treatments for prion diseases. The technique, which employs base editing to directly manipulate the gene encoding prion proteins, has shown promising results. Nevertheless, it is important to approach the clinical applications with caution as researchers continue to navigate the complexities of translating these findings from animal models to human trials. The road ahead includes rigorous testing and refining of these therapies to ensure they are both safe and effective for patients afflicted with conditions like Creutzfeldt-Jakob disease and fatal familial insomnia.
As Vallabh and Minikel note, their work is not just academic but deeply personal, stemming from their own connections to fatal familial insomnia. Their unique perspective as patient-scientists enhances their commitment to finding a viable treatment, highlighting the extraordinary potential of collaborative research that brings together scientific ingenuity and personal experience.
Challenges and Precautions in Researching Prion Diseases
Conducting research on prion diseases presents unique challenges due to the infectious nature of prions. Unlike other pathogenic agents, prions are non-traditional infectious proteins that can cause neurodegeneration without the typical inflammatory response associated with bacteria or viruses. This peculiarity demands rigorous safety protocols during experiments to prevent accidental exposure, as evidenced by unfortunate incidents such as the death of a researcher from prion disease caused by accidental exposure in a lab. As researchers strive to develop gene editing therapies, safety is paramount.
Furthermore, the complexity of prion diseases necessitates thorough research before any new therapies can reach the clinic. For example, even the promising gene-editing approaches face hurdles; the teamwork between experts at the Broad Institute, including specialized engineers focusing on vector technology, is critical to refining the delivery of therapies. Optimizing the vector used to deliver gene editing tools into cells while minimizing risks of toxicity is an ongoing area of investigation. This meticulous work is vital to ensure that once human trials commence, the treatment will not only be effective but also safe for those in desperate need of solutions.
Patient-Scientists Leading the Charge for Hope
The collaboration between patient-scientists like Sonia Vallabh and Eric Minikel and their colleagues at the Broad Institute represents a transformative approach in scientific research. Their lived experience with fatal familial insomnia propels them to innovate tirelessly toward solutions that can alter the course of prion diseases. This personal connection fuels their passion and emphasizes the importance of integrating patient perspectives in medical research. As they navigate the scientific landscape, their story embodies hope not just for those with prion diseases, but for everyone involved in the fight against seemingly insurmountable health challenges.
This patient-centric model of research highlights the importance of collaboration across disciplines and institutions. Vallabh and Minikel’s efforts have inspired researchers to engage more deeply with the implications of their work, reminding them that the ultimate aim is to alleviate suffering and enhance patients’ quality of life. This mission drives a collective pursuit of knowledge that is both scientific and deeply human, with the promise of breakthroughs that could lead to effective treatments for prion diseases and beyond.
The Future of Therapeutic Strategies for Prion Diseases
Looking ahead, the future of therapeutic strategies for prion diseases appears to be bright, thanks to breakthrough technologies like gene editing. The collaborative work of researchers, patient-advocates, and institutions positions them well to navigate the complexities of developing viable treatments. The emergence of new techniques, along with increased funding and public engagement, provides a fertile ground for innovation. As research progresses, it is likely that we will continue to see a wave of developments aimed at not only treating prion diseases but also enhancing our understanding of their underlying biology.
However, the path to clinical application will require patience and perseverance. While the exciting results from preclinical studies are promising, researchers must ensure that all safety and efficacy concerns are addressed before embarking on human trials. As collective efforts intensify, the scientific community remains hopeful that persistence and innovation will converge to yield breakthrough treatments that can change lives and perhaps even pave the way towards cures for prion diseases like Creutzfeldt-Jakob disease and fatal familial insomnia.
Collaboration: The Key to Advancements in Prion Disease Research
Collaboration is paramount in advancing the field of prion disease research, especially given the intricate nature of these disorders. The synergy between geneticists, neurologists, and patient advocates, such as Vallabh and Minikel, demonstrates how multifaceted approaches can lead to significant breakthroughs. By working together, these experts can share insights, techniques, and resources that enhance the overall quality of research and accelerate progress toward viable gene editing therapies.
In addition to interdisciplinary collaboration, utilizing various research models—including both human and animal studies—is essential for understanding the full impact of prion diseases. The ongoing partnership between labs and institutions fosters an environment of shared knowledge and innovation, which is crucial in tackling the challenges posed by these rarely studied conditions. As the body of research grows, so does the potential for discovering novel treatment pathways that will ultimately benefit patients suffering from debilitating prion diseases.
The Role of Funding and Resources in Prion Disease Research
Funding and resources are critical components for the success of research endeavors focused on prion diseases. Initiatives funded by organizations such as the National Institutes of Health and private foundations not only support exploratory research but also enable scientists to conduct comprehensive studies that lead to potential therapeutic breakthroughs. As research teams like Vallabh and Minikel’s continue to innovate and develop gene editing technologies, securing adequate funding remains a pivotal challenge that can dictate the pace and extent of their progress.
Moreover, increased public interest and investment in rare diseases can help sustain ongoing research efforts. Cultivating partnerships between academic institutions, pharmaceutical companies, and government agencies can create a more robust funding landscape, allowing researchers to explore uncharted territories in prion biology and treatment innovation. As interest in gene editing technology grows, the potential for developing effective interventions for conditions like Creutzfeldt-Jakob disease and fatal familial insomnia becomes increasingly feasible, underlining the importance of communal support for scientific inquiry.
The Importance of Early Diagnosis in Prion Diseases
Early diagnosis of prion diseases is crucial for optimizing patient outcomes and tailoring treatment strategies. Due to the progressive nature of these disorders, timely identification can not only help manage symptoms but also provide families with essential information regarding genetic risks associated with the conditions. This understanding is particularly important for inherited cases, such as fatal familial insomnia, where family members may wish to explore genetic testing and counseling options.
As research continues to uncover the mechanisms behind prion diseases, incorporating advanced diagnostic tools that leverage genetic and biochemical markers could significantly enhance early detection capabilities. Efforts aimed at educating healthcare providers and increasing awareness among the general public can facilitate earlier referrals to specialists and ultimately lead to more informed decisions for affected families. Thus, early diagnosis emerges as a key pillar in addressing the challenges posed by prion diseases and improving the trajectory of patient care.
Patient Advocacy and Its Influence on Prion Disease Research
Patient advocacy plays a transformative role in shaping the research landscape for prion diseases. Individuals like Sonia Vallabh, who share their personal journeys, illuminate the pressing need for research and innovation in the field. Their stories resonate with both the scientific community and policymakers, driving public awareness and support for funding initiatives that target prion diseases. By channeling their experiences into advocacy, patient-advocates not only elevate the conversation around prion diseases but also inspire a new generation of researchers to engage with these critical issues.
Moreover, patient-advocates often bring unique insights into the complexities of their conditions, highlighting gaps in knowledge and unmet needs that guide research priorities. By fostering collaboration between scientists and patients, advocacy groups can ensure that research efforts remain aligned with the real-world challenges faced by individuals living with prion diseases. This collaboration ultimately lays the groundwork for developing therapies that are informed directly by the experiences of those affected, creating a more holistic approach to treatment.
Frequently Asked Questions
What advancements have been made in prion disease treatment involving gene editing therapy?
Recent research has made significant strides in prion disease treatment by utilizing gene editing therapy. Scientists at the Broad Institute of MIT and Harvard have demonstrated that altering a single base in the gene responsible for producing harmful prion proteins can reduce their levels in mice by half. This groundbreaking work has shown an extension of the mice’s lifespan by 52%, providing hope for future treatments of prion diseases such as Creutzfeldt-Jakob disease and fatal familial insomnia.
Who are Sonia Vallabh and Eric Minikel, and what is their role in prion disease treatment research?
Sonia Vallabh and Eric Minikel are pivotal figures in the field of prion disease treatment research, particularly known for their personal connection to the disease. Vallabh has tested positive for fatal familial insomnia, which has driven both her and Minikel to retrain as scientists. They now lead a research lab at the Broad Institute, focusing on developing effective therapies for prion diseases using innovative gene editing technologies.
What is the significance of the milestone reached in prion disease treatment?
The recent milestone in prion disease treatment, highlighted in a study published in ‘Nature Medicine,’ signifies a crucial breakthrough in understanding how to combat diseases like Creutzfeldt-Jakob disease. The application of a gene editing approach that effectively reduces the production of toxic prion proteins in a mouse model underscores the potential pathway toward human clinical trials and effective treatments.
What challenges remain in developing prion disease treatment before human trials?
Despite the promising results from gene editing therapy for prion diseases, several challenges must be overcome before human trials can commence. Researchers must refine the base editing technology to improve its safety and efficiency, enhance targeting mechanisms to minimize off-target effects, and determine optimal dosing methods. These steps are critical to ensure the therapeutic interventions are safe and effective in humans.
How do prion diseases like fatal familial insomnia and Creutzfeldt-Jakob disease differ?
Prion diseases, including fatal familial insomnia and Creutzfeldt-Jakob disease, are caused by misfolded proteins leading to brain damage and dementia. Fatal familial insomnia is hereditary and associated with specific genetic mutations, whereas Creutzfeldt-Jakob disease occurs sporadically or can be inherited. Both diseases are invariably fatal and represent a significant focus for developing effective treatments through innovative approaches like gene editing therapy.
What role does animal research play in advancing prion disease treatment therapies?
Animal research, particularly using mouse models of human prion diseases, is crucial for advancing potential prion disease treatments. These models allow researchers to assess the effectiveness of gene editing therapies in reducing prion protein levels and evaluating safety profiles before moving to human trials. Successful outcomes in these models can provide the necessary evidence to support transitioning to clinical testing.
| Key Points | Details |
|---|---|
| Research Milestone | Breakthrough in gene-editing therapy showing potential for prion disease treatment. |
| Research Collaboration | Involvement of patient-scientists Sonia Vallabh and Eric Minikel, with personal stakes in prion disease. |
| Prion Disease Overview | Includes Creutzfeldt-Jakob disease, Gerstmann-Straüssler-Scheinker disease, and fatal familial insomnia. |
| Scientific Approach | Altering the gene producing toxic proteins in mouse models has shown to reduce protein levels and increase lifespan. |
| Future Steps | Multiple milestones and specific refinements are necessary before human trials can occur. |
Summary
Prion disease treatment is making remarkable strides as new research offers hope for developing effective therapies. This research, initiated and driven by patient-scientists, highlights the potential of gene-editing technologies to combat the effects of these rare and fatal disorders. With continued efforts, there is optimism that a viable treatment pathway is within reach.

Breakthrough Prizes 2025: Harvard Scientists Receive Awards
The Breakthrough Prizes 2025 have once again highlighted groundbreaking advancements in science, with three esteemed Harvard scientists taking the spotlight. This year’s award recipients include Alberto Ascherio, recognized for his pivotal research revealing the Epstein-Barr virus as a major cause of multiple sclerosis, a condition that affects millions worldwide. Joel Habener’s work on GLP-1 has also transformed diabetes treatment, significantly impacting the fight against obesity and insulin resistance. Additionally, David Liu’s innovative gene editing technologies have set new standards in genetic research, promising revolutionary treatments for a variety of disorders. Together, these laureates embody the essence of scientific exploration, showcasing how rigorous research can lead to profound societal benefits and inspire future generations in tackling complex health challenges.
In the realm of scientific achievements, the 2025 Breakthrough Prizes stand as a prestigious recognition for impactful research contributions. Celebrated as the “Oscars of Science,” these awards emphasize the importance of advancements in fields like gene editing, epidemiology, and hormone research. The groundbreaking discoveries of Harvard’s top scientists, including significant findings related to multiple sclerosis, diabetes treatments, and genetic therapies, demonstrate the power of innovation in addressing critical health issues. This honor not only recognizes individual excellence but also underscores the collaborative efforts that lead to transformative solutions in medicine and biology. The Breakthrough Prizes provide a platform for acknowledging those who push the boundaries of our understanding, ultimately striving for a healthier future.
Alberto Ascherio’s Groundbreaking Research on Epstein-Barr Virus and MS
Alberto Ascherio’s recent recognition at the 2025 Breakthrough Prizes highlights the escalating understanding of the Epstein-Barr virus (EBV) as a leading cause of multiple sclerosis (MS). His extensive research, which spanned over 25 years, has profoundly impacted MS research by establishing a solid link between EBV infection and MS onset. The results of his study, based on a remarkable data set of over 10 million U.S. soldiers, are pivotal as they provide compelling evidence for targeting EBV in future MS treatments. Ascherio’s transformative discovery not only reshapes our understanding of MS but also paves the way for innovative vaccine designs and antibody therapies aimed at combating this debilitating disease.
This acknowledgment from the Breakthrough Prizes underscores the importance of scientific inquiry into chronic diseases like multiple sclerosis, which currently affects millions worldwide. Ascherio’s persistent efforts exemplify how long-term research can lead to significant breakthroughs, inspiring a new wave of studies focused on viral infections as an underlying cause of autoimmune conditions. Moreover, his findings advocate for a more proactive approach in public health strategies aimed at controlling EBV to mitigate subsequent MS risks.
Ascherio’s contributions evoke critical discussions regarding the broader implications of his work in epidemiology and viral pathology. The advent of a potential vaccine, stemming from this research, could revolutionize how we treat and prevent MS, changing the narrative for patients suffering from the disease. Given that MS has long been regarded as an unpreventable ailment, identifying EBV as a significant risk factor dramatically alters the context, suggesting that infection prevention and early intervention strategies could be vital. As research evolves, the focus may shift towards population-based studies that assess the preventive measures against EBV, leading to greater awareness and potentially reducing the incidence of MS in the long term.
GLP-1 Diabetes Treatment and its Impact on Obesity
Joel Habener’s collaborative work on glucagon-like peptide-1 (GLP-1) represents a significant milestone in diabetes management and obesity treatment, recognition that was celebrated at the 2025 Breakthrough Prizes. GLP-1 plays a central role in glucose metabolism and appetite regulation, making it a crucial target for therapeutic interventions. The recognition of this hormonal pathway has catalyzed the development of new GLP-1 receptor agonists that not only improve glycemic control in Type 2 diabetes but also promote weight loss, thus addressing two critical aspects of metabolic health simultaneously.
The implications of Habener’s research extend far beyond individual treatments. The advancement in understanding GLP-1 has sparked a wave of innovation in creating multifaceted approaches to tackle obesity, one of the leading health crises of our time. By elucidating the hormonal interactions that govern appetite and energy balance, researchers can develop more effective therapies to manage metabolic disorders and enhance patient outcomes, further solidifying GLP-1’s role in chronic disease management.
Moreover, the widespread adoption of GLP-1 based treatments highlights an urgent need for healthcare systems worldwide to integrate these findings into clinical practice. As the landscape of diabetes and obesity treatment evolves, the recognition of the interplay between various hormones offers a holistic approach to managing these conditions. Advances in GLP-1 research not only support better therapeutic outcomes but also underscore the significance of multidisciplinary collaboration in science. By fostering partnerships among endocrinologists, nutritionists, and researchers, it is possible to create comprehensive management programs that empower patients to achieve lasting health improvements.
David Liu’s Innovations in Gene Editing Technologies
David Liu’s groundbreaking contributions to gene editing technologies, particularly base editing and prime editing, were celebrated with a prestigious award at the 2025 Breakthrough Prizes. These cutting-edge techniques have revolutionized the field of genetic research by enabling precise genetic modifications with unprecedented accuracy. Base editing allows researchers to directly convert one DNA base into another without causing double-strand breaks, thereby minimizing potential off-target effects. Meanwhile, prime editing opens new avenues for genomic manipulation, permitting not just substitutions but also insertions and deletions, thus addressing a broader spectrum of genetic variances that underlie many diseases.
The implications of Liu’s work extend beyond academia into clinical applications, as the promise of applicable treatments for genetic disorders advances significantly. With these technologies already included in various clinical trials, many lives stand to benefit from innovations that transform genetic anomalies into treatable conditions. Liu’s emphasis on collaborative efforts behind these technologies highlights the importance of teamwork in scientific advancements, showcasing how collective innovation is the key to unlocking the therapeutic potential of genome editing.
Furthermore, with Liu’s gene editing methodologies rapidly gaining traction in laboratories around the globe, we are poised on the verge of a new era in medicine that could lead to cures for previously untreatable genetic diseases. The societal impact of these advancements could be monumental, changing the narrative surrounding genetic conditions and providing hope for a healthier future. Liu’s insistence on the crucial role played by graduate students and postdoctoral researchers in these breakthroughs serves as a reminder of the vitality of mentorship and education in science, ensuring that the next generation of scientists will continue to push the boundaries of what is possible in genetic research.
Frequently Asked Questions
What are the Breakthrough Prizes 2025 and who were the winners?
The Breakthrough Prizes 2025, known as the ‘Oscars of Science’, recognized three notable Harvard scientists: Alberto Ascherio for his groundbreaking research on Epstein-Barr virus as a leading cause of multiple sclerosis (MS), Joel Habener for contributions to GLP-1 diabetes treatments, and David Liu for his pioneering work in gene editing technologies including base editing and prime editing.
How did Alberto Ascherio’s research on Epstein-Barr virus impact multiple sclerosis studies in the 2025 Breakthrough Prizes?
Alberto Ascherio’s research, honored at the 2025 Breakthrough Prizes, established the Epstein-Barr virus as a significant risk factor for developing multiple sclerosis (MS). This crucial finding has transformed MS research, leading to advances in vaccine development and therapeutic antibodies targeting the virus, thereby marking a pivotal shift in understanding and combating MS.
What role does GLP-1 play in diabetes treatment recognized at the 2025 Breakthrough Prizes?
The 2025 Breakthrough Prizes highlighted Joel Habener’s work on GLP-1, a hormone vital for regulating blood sugar and appetite. This research led to the creation of GLP-1 based drugs that effectively manage Type 2 diabetes and obesity, showcasing a significant advancement in diabetes treatment.
What are base editing and prime editing as related to the Breakthrough Prizes 2025?
David Liu was recognized at the 2025 Breakthrough Prizes for his development of base editing and prime editing technologies. These innovative gene editing platforms can correct most genetic variations causing diseases, with real-world applications already seen in 15 clinical trials, offering hope for many genetic disorders.
How have the Breakthrough Prizes 2025 impacts the fields of MS, diabetes, and gene editing?
The Breakthrough Prizes 2025 celebrated key advancements in multiple sclerosis research, GLP-1 diabetes treatments, and gene editing technologies. Alberto Ascherio’s findings on Epstein-Barr virus, Joel Habener’s contributions to diabetes management, and David Liu’s revolutionary gene editing techniques illustrate significant strides in scientific research aimed at solving complex health challenges.
What significance do the Breakthrough Prizes hold for researchers like those at Harvard?
The Breakthrough Prizes, awarded in 2025 to Harvard scientists, signify the highest level of recognition in scientific achievement. They celebrate monumental contributions to health and medicine, encouraging ongoing research and innovation in fields like MS, diabetes, and genetic diseases, and fostering a culture of excellence among researchers.
Where can I find more detailed information on the Breakthrough Prizes 2025 winners?
Further information on the 2025 Breakthrough Prizes winners, including their individual contributions—such as Ascherio’s MS research on Epstein-Barr, Habener’s work on GLP-1, and Liu’s gene editing—can be explored through reputable scientific news outlets and the official Breakthrough Prize website.
| Scientist | Affiliation | Contribution | Significance |
|---|---|---|---|
| Alberto Ascherio | Harvard T.H. Chan School of Public Health & Harvard Medical School | Identified Epstein-Barr virus as a leading cause of multiple sclerosis (MS) | Groundbreaking findings led to a vaccine and antibody drugs for MS. |
Summary
The 2025 Breakthrough Prizes celebrated the outstanding achievements of Harvard scientists in significant health advancements. Alberto Ascherio, Joel Habener, and David Liu were honored for their groundbreaking research that revolutionizes our understanding of diseases such as multiple sclerosis, diabetes, and hereditary conditions through innovative gene editing techniques. Their work not only advances scientific knowledge but also holds the potential to transform treatments, highlighting the vital role of research in paving the way for future medical breakthroughs.